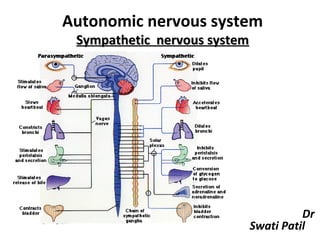
2. sympathetic nervous system
- 1. Autonomic nervous system Sympathetic nervous system Dr Swati Patil 1
- 2. • Autonomic nervous system -History -Introduction -Types :- Sympathetic –Development -Introduction -Course -Types -Applied 2
- 3. Autonomic Nervous System • Self regulating • History: – 1898 - J.N.Langley assigned the term Autonomic Nervous System – 1921 – subdivided ANS into • Sympathetic • Parasympathetic • Enteric 3
- 4. 4
- 5. Autonomic Nervous System • Introduction – Visceral component of nervous system , function closely related to somatic nervous system – Visceral afferent pathways resemble somatic afferent – Peripheral processes – auotonomic ganglia – somatic nerves 5
- 6. Visceral Afferents -Cell bodies –unipolar – present in cranial sensory or dorsal root ganglia -Central processes –with somatic afferents into CNS –establish connections 6
- 7. Visceral Efferent • Visceral efferent pathways in ANS differ from their somatic equivalents • pre-ganglionic neurons: – Somata are located in • visceral efferent nuclei & • in lateral grey columns – axons are • myelinated , • pass to peripheral ganglia • synapse with postganglionic neurons 7
- 8. Visceral Efferents Pre-ganglionic Post-ganglionic ganglion 8
- 9. • Post-ganglionic neurons –axons are unmyelinated , more numerous 9
- 10. Subdivisions of ANS • Sympathetic • Parasympathetic • Enteric 10
- 11. • Sympathetic –mass response - Constriction of cutaneous arteries - Cardiac acceleration - Rise in blood pressure - Contraction of sphincters - Depression of peristalsis • Sympathetic: mobilization & increased metabolism “fight, flight or fright” or “fight, flight or freeze” 11
- 12. Neurotransmitters: • pre-ganglionic neurons of both are cholinergic • post-ganglionic – parasympathetic –cholinergic – sympathetic –nor-adrenergic • principal co-transmitters – ATP , Neuropeptide Y 12
- 13. Sympathetic Nervous System • Development :- -During 5th week, neural crest cells migrate along sides of spinal cord ganglia - dorsolateral to aorta -Some neural crest cells migrate ventral to aorta pre-aortic ganglia – celiac & mesenteric ganglia 13
- 14. • Other neural crest cells migrate to heart, lungs, GIT terminal ganglia • Axons of sympathetic neurones in intermediolateral cell column of thoracolumbar seg of spinal cord pass through ventral root of spinal nerve & white ramus communicans to reach paravertebral ganglia 14
- 15. • Synapse with neurons – ascend / descend in sympathetic trunk • Other presynaptic fibers – pass through paravertebral ganglia without synapsing – splanchnic nerves to viscera • Post synaptic fibres –grey rami from sympathetic ganglion into spinal nerve • Sympathetic trunk – ascending & descending fibres 15
- 16. Sympathetic Trunk • Two ganglionated nerve cords –either side of vertebral column • White & grey rami communicantes • Location –neck ,thorax, abdomen, pelvis 16
- 17. Preganglionic neurones: • Cell bodies of preganglionic sympathetic neurons –in lateral horn • Axons –myelinated ,diam -1.5 - 4 microm • Leave cord in ventral nerve roots – pass into spinal nerves, soon leave in white rami communicants 17
- 18. Behaviour of Preganglionic Fibres • Synapse with neurons in nearest ganglion or may ascend or descend • Fibres terminate in single ganglion or through collateral branches – synapse • Fibres may ascend or descend without synapsing –emerge in branches of sympathetic trunk –synapse in ganglia of autonomic plexus 18
- 19. Postganglionic Neurones of Sympathetic Nervous System • Somata of postganglionic neurons –in ganglia of sympathetic trunk • Axons –unmyelinated, return to spinal nerve through grey ramus just proximal to white ramus & then form dorsal & ventral ramus 19
- 20. Cervical Sympathetic Trunk • B/w Carotid sheath and prevertebral muscles • Internal carotid nerve • Three cervical ganglia – Superior – Middle – Inferior 20
- 21. Superior Cervical Ganglion • Largest ganglion • Lies in front of transverse processes of C2 and C3 vertebrae • Branches – Medial – Lateral 21
- 22. Middle Cervical Ganglion • Smallest of the Cervical ganglion • Lies on the C6 vertebra in front or behind Inf. thyroid artery • Branches – grey rami communicantes – Cardiac branch – Vascular Branch 22
- 23. Stellate Ganglion • Formed by the fusion of C7,C8 andT1 ganglia • Lies b/w neck of 1st Rib and transverse process of C7 vertebra • Branches – Grey rami communicans – Vascular branches 23
- 24. Sympathetic supply – Head and Neck • Preganglionic fibres – T1-T5 segments of Spinal Cord • Ascend in Sympathetic Trunk • Synapse in cervical ganglia 24
- 25. Thoracic Sympathetic Trunk • Comprises of 11 ganglia • Ganglia lie against the heads of ribs • Branches – Grey rami communicans – Pul. And cardiac Plexus – Splanchnic Nerves 25
- 26. Coeliac Plexus • Situated around the origin of coeliac artery • Formed by greater Splanchnic Nerves and Ist lumbar sympathetic nerves • Nerves from the plexus supply abdominal viscera via blood vessels 26
- 27. Lumbar Sympathetic Trunk • Lies retroperitoneally on the anterolat. surface of lumbar vertebrae • Rt side – overlapped by IVC • Lt side – overlapped by Aorta • Branches – Splanchnic nerves – Grey rami communicantes 27
- 28. Hypogastric Plexuses • Superior hypogastric plexus:- -location -formation -branches • Inferior hypogastric plexus :- -location -formation -branches 28
- 29. Adrenal Medulla • Neural crest cells – secretary cells of medulla • Sympathetic supply – preganglionic sympathetic neurons • Secretary cells – postganglionic sympathetic neurons –lack axons or dendrites • Larger secretory cells – secrete adrenaline & NA 29
- 30. Summary 30
- 31. Sympathetic Ganglion Histology : • Connective tissue, ganglion, capsule cells • Nerve cells –multipolar, smaller • Nucleolus –prominent eccentric 31
- 32. Sympathetic Ganglion 32
- 33. Enteric Nervous System • Myenteric (Auerbach’s) plexus & submucosal (Meissner) plexus • Plexus –small enteric ganglia –joined by thin nerves –unmyelinated • Avascular –nutrition by diffusion • Neurones –excitatory & inhibitory • Afferents to ENS -2 types – cholinergic & NA 33
- 34. Pain Afferents • Sensory neurones –pain in thoracic & abdominal organs • Cell bodies –dorsal root ganglia • Peripheral processes – white communicating rami –sympathetic trunk –viscera 34
- 35. • Referred pain –diffuse localization & radiation • Zone of reference of pain from int organ coincides with part of body served by somatic sensory neurons assoc with same segment of spinal cord 35
- 36. Referred Pain • Heart –middle & inferior cervical cardiac nerves, thoracic cardiac branches of left sympathetic chain • Gall bladder –greater splanchnic nerve , diaphragm –phrenic nerve 36
- 37. • Stomach –epigastrium – Rt & Lt greater splanchnic nerves • Duodenal ulcer –AAW – T9 T10 • Appendix –lesser splanchnic nerves –T10 • Pelvis & ureter –least splanchnic nerves –loin & groin 37
- 38. Surgical Sympathectomy • Indications – Peripheral vascular disease –sympathectomy –temporary vasodilatation –development of collaterals – Hyperhidrosis –sympathectomy –permanent relief – Relief of Pain –a) visceral pain –excision / destruction – coeliac ganglia –Ca pancreas, chronic pancreatits – b) causlgia –intense pain 38
- 39. Upper Thoracic and Cervical Sympathectomy • Upper limb -2 & 3 thoracic ganglia with rami & intervening part • 1st thoracic –not removed, preganglionic fibres not arise above T2 (removal – Horner’s syndrome) 39
- 40. Kuntz Nerve • Communicating branch B/w T1and T2 nerves • Receives Grey rami from Stellate and T2 ganglia • Clinical relevance –failure to identify during thoracic sympathectomy 40
- 41. Lumbar Sympathectomy • Gangliectomy -3 & 4 lumbar ganglia & intervening trunk • Removal of LI is harmful – interferes with ejaculation 41
- 42. Horner’s Syndrome • Preganglionic –white ramus of T1 –sympathetic trunk – superior cervical ganglion – postganglionic fibres (ICA) – ophthalmic –nasociliary – long ciliary branches • Damage –vascular lesions of cortex / brainstem, cervical rib, Ca lung, thyroid, oesophagus 42
- 43. Clinical features of Horner’s syndrome: • Miosis –failure dilation – unopposed parasympathetic activity • Partial ptosis –paralysis of LPS • Anhydrosis –lesion of superior cervical ganglion 43
- 44. Central Control of Sympathetic Nervous System • Hypothalamus –controlling &integrating center • Hypothalamus –autonomic nuclei –spinal cord – reticular formation • Posterior & lateral nuclei – noradrenergic response 44
- 45. THANK YOU… 45
