Thyroid
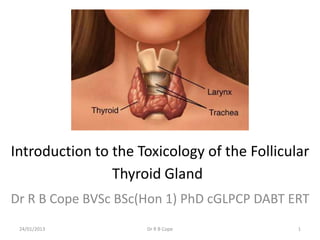
- 1. Introduction to the Toxicology of the Follicular Thyroid Gland Dr R B Cope BVSc BSc(Hon 1) PhD cGLPCP DABT ERT 24/01/2013 Dr R B Cope 1
- 2. Learning Objectives • To understand the key basic functional aspects of the thyroid; • To understand how thyroid dysfunction is detected and measures; • To understand and accurately interpret changes in thyroid parameters; • To understand and accurately interpret the human relevance of changes to thyroid parameters in rodent toxicology studies; 24/01/2013 Dr R B Cope 2
- 3. Basic Terms • Triiodothyronine = T3 = 3, 5, 3’ triiodothyronine; the most active of the follicular thyroid hormones • Reverse triiodothyronine = rT3 = 3,3’5’-triiodothyronine; a biologically inactive isomer of T3 • Thyroxine = T4 = 3,5,3’,5’ tetraiiodothyronine; has some activity in the periphery but mostly functions in vivo as a pro- hormone (converted to T3 in the periphery) • Thyroglobulin = Tg; a 660 kDa dimeric protein produced by the follicular cells of the thyroid and used to produce T3 and T4. Tg forms the colloid in the follicular thyroid gland 24/01/2013 Dr R B Cope 3
- 4. Basic Terms • MIT = monoiodotyrosine; forms part of the thyroid colloid. Colloid thryoperoxidase enzymatically binds iodine to tyrosine residues in Tg in the thyroid colloid • DIT = diiodotyrosine; synthesis is similar to that of MIT • MIT + DIT combine to form T3 or r-T3 • DIT + DIT combine to form T4 24/01/2013 Dr R B Cope 4
- 5. Basic Thyroid Histology 24/01/2013 Dr R B Cope 5
- 6. Basic Concepts: Synthesis of Thyroid Hormones • Tg is synthesized in the RER and follows the secretory pathway to enter the colloid in the lumen of the thyroid follicle by exocytosis. • - Meanwhile, a sodium-iodide (Na/I) symporter pumps iodide (I-) actively into the cell • - I- enters the follicular lumen from the cytoplasm by the transporter pendrin • - In the colloid, I- is oxidized to iodine (I0) by an enzyme called thyroperoxidase. • - I0 is very reactive and iodinates the Tg at tyroine residues in its protein chain. • During conjugation, adjacent tyrosine residues are paired together. • The entire complex re-enters the follicular cell by endocytosis. • Proteolysis by various proteases liberates T3, rT3 and T4 which enter the blood by largely unknown mechanisms. 24/01/2013 Dr R B Cope 6
- 7. Important Species Differences in Thyroperoxidases • Thyroperoxidase in rats, mice and dogs are sensitive to inhibition by xenobiotics • Result of inhibition is disruption of T4 synthesis increased thyroid load (see thyroid economy below) increased sensitivity to thyroid follicular hyperplasia/neoplasia • Thioamides (sulfonamides) are notably inhibitors of thyroperoxidase • Other notable inhibitors: propylthiouracil (PTU), methimazole, aminotriazole, acetoacetamide 24/01/2013 Dr R B Cope 7
- 8. T3 and T4 Transport in the Blood • Normal ratio of T4 to T3 in blood is about 20:1 • In most species the majority of T3 and T4 in plasma is bound to proteins • TBG is the critical protein – affinity for T4 is about 1000 times higher than that of other proteins • Bound T3 and T4 are not biologically active; only the unbound T3 and T4 are biologically active (important when measuring/interpreting plasma or serum T3 and T4 levels) • Protein binding of T3 and T4 is very important – increases the circulating T½ of the hormones, which in turn protects the 24/01/2013 Dr R B Cope 8 follicular thyroid gland
- 9. T3 and T4 Transport in the Blood • There is a critical difference with big biological consequences in rodents (notably rats): – The plasma T½ for T4 in rats is short (12-24 hours compared with 5 – 9 days in humans) – Plasma T½ for T3 is about 1 day in most species (what are the implications?) – Rats have low plasma TBG – T4 binding is primarily limited to albumin and prealalbumin which have much lower binding affinities – What are the implications of all of this? 24/01/2013 Dr R B Cope 9
- 10. T3 and T4 Transport in the Blood • There is a critical difference with big biological consequences in rodents (notably rats): – Net result is that rats have to produce about 10 times more T4 per unit body weight than humans – T3 in humans is transported in the plasma mostly bound to TBG, however in rats and mice, T3 does not bind to TBG faster T3 turnover in rats versus humans greater thyroid demand – Overall result is that rats and mice have a substantially lower thyroid economy compared with humans much greater sensitivity to developing thyroid hyperplasia and neoplasia than humans 24/01/2013 Dr R B Cope 10
- 11. Thyroid Hormones in the Periphery • T4 is converted to the active T3 within cells by deiodinases (5'- iodinase) – All three isoforms of the deiodinases are selenium- containing enzymes, thus dietary selenium is essential for T3 production. • These are further processed by decarboxylation and deiodination to produce inactive iodothyronamine (T1a) and thyronamine (T0a). 24/01/2013 Dr R B Cope 11
- 12. Actions of T3 in the Periphery • Increases cardiac output • Increases heart rate • Increases ventilation rate • Increases basal metabolic rate • Potentiates the effects of catecholamines (i.e. increases sympathetic activity) • Potentiates brain development • Thickens endometrium in females • Increases metabolism of proteins and carbohydrates 24/01/2013 Dr R B Cope 12
- 13. Metabolism and Excretion of T3 and T4 UGT = UDP-glucuronosyltransferases SULT = Sulfotransferases 24/01/2013 Dr R B Cope 13
- 14. Regulation of Thyroid Hormones: The Hypothalamic-Pituitary-Thyroid Axis • TSH is released from the anterior pituitary gland in response to thyroid releasing hormone from the hypothalamus and causes the synthesis and secretion of T3 and T4 by the thyroid gland. This is acheived by stimulation of the thyroid follicular cells by binding of TSH to the receptor on the basal surface of the cell and activation of acetylate cyclase. This leads to increased iodide uptake. • T3 and T4 exert negative feedback on both the pituitary production of TSH and the hypothalamic production of TRH. • Other factors affecting release of TRH from the hypothalamus include blood levels glucose and the body's metabolic rate. • Somatostatin inhibits TSH secretion and estrogen has been shown, in rats, to reverse the negative feedback affect of T3 and T4 on the TSH response to TRH. • SS is produced by the GI, pancreas and hypothalamus – important in regulation of body size and in obesity 24/01/2013 Dr R B Cope 14
- 15. Sex Differences in TSH Drive • There is a critical difference with big biological consequences in male rats: – TSH levels are higher in males than in females – Effect is related to testosterone levels – Higher TSH levels in males greater demand on the follicular thyroid increased sensitivity to thyroid neoplasia compared with female rats 24/01/2013 Dr R B Cope 15
- 16. Measurement of Thyroid Status: Thyroid Function Tests • Typically a combination of measures are required – single tests are frequently insufficient to determine thyroid status! • Available measures are: – Serum TSH – Total Serum T4 – Free Serum T4 – Total Serum T3 – Free Serum T3 – Serum T3:T4 ratio – Serum TBG = T3 resin uptake test (T3U) – Serum Tg • 123I uptake • Imaging • Histopathology/fine needle aspirate (really a human thing) 24/01/2013 Dr R B Cope 16
- 17. Thyroid Function Tests: Serum TSH • TSH levels peak in the evening and are lowest in the afternoon, with marked variations due to physiologic conditions such as illness, and low energy intake. • A variety of drugs can result in artifactual or biological changes to TSH levels 24/01/2013 Dr R B Cope 17
- 18. Thyroid Function Tests: Serum TSH • Increases in TSH are associated with loss of negative feedback on the hypothalamic-pituitary-thyroid axis due to: – Primary hypothyroidism due to disruption of T4 or T3 synthesis (iodine deficiency, disruption of I- uptake, inhibition of thyroperoxidase, inhibition of Tg synthesis, inhibition of T3/T4 release) – Increased utilization/destruction of T4 or T3 in the periphery (e.g. induction of 5’ iodinases) – TSH producing pituitary tumor (rare) – Pituitary resistance to T3 and T4 (disruption of negative feedback) – Increased demand for T3 and T4 e.g. hypermetabolic states 24/01/2013 Dr R B Cope 18
- 19. Thyroid Function Tests: Serum TSH • Decreases in TSH are associated with excessive negative feedback on the hypothalamic-pituitary-thyroid axis due to: – Hyperthyroidism – Pituitary (secondary) hypothyroidism (decreased TSH production; rare) – Some non-thyroid related diseases (rare) 24/01/2013 Dr R B Cope 19
- 20. Thyroid Function Tests: Total Serum T4 (Thyroxine) • Increased total T4 occurs in hyperthyroid states or if there is an increased TBG (can be acquired) or if the animals are treated with thyroxine • Decreased total T4 occurs in hypothyroid states or with TBG deficiency – Heritable TBG deficiency occurs in humans and is non-harmful; heritable gene difference – Acquired TBG deficiency can be caused by protein malnutrition, chronic liver and kidney disease, glucocorticoids and androgenic steroids • Remember that total T4 is a relatively insensitive measure of the T4 biological activity (T4 has to be non-protein bound to be biologically available) – In some senses it is a measure of the readily available reserve of free (biologically active) T4 and T3 24/01/2013 Dr R B Cope 20
- 21. Thyroid Function Tests: Serum Free T4 (Thyroxine) and Free T4 Index • Despite the names, these are an indirect estimate of unbound T4 in the blood • The advantage is that the biologically available form is measured, correcting for variations in TBG levels • The disadvantage is that no currently available test accounts for all the currently known T4 protein binding abnormalities 24/01/2013 Dr R B Cope 21
- 22. Thyroid Function Tests: Serum Total T3 • Advantage: measuring the ultimate hormone rather than a pro-hormone • Disadvantage: high inter-laboratory variability in measurement and normal ranges • Again, the measurement reflects the circulating storage pool of T3 rather than the small fraction of unbound T3 that is biologically active 24/01/2013 Dr R B Cope 22
- 23. Thyroid Function Tests: Serum Free T3 • Rarely performed because of variation in the normal range across different populations and inter-laboratory variation • Has the advantage that you are measuring the biologically available levels of the ultimate-hormone 24/01/2013 Dr R B Cope 23
- 24. Thyroid Function Tests: Serum T3:T4 ratio • The T3/T4 ratio is a simply calculated index reflecting thyroid function and the action of hormones on the tissues • In normal subjects the T3/T4 ratio is influenced neither by the body weight nor by the physical activity level, sex, or the blood sampling conditions • The nutritional status can influence the ratio if there is inadequate iodine intake or if there is weight loss 24/01/2013 Dr R B Cope 24
- 25. Thyroid Function Tests: Serum T3:T4 ratio • T3/T4 is increase in hyperthyroid states because of increased T3 secretion relative to T4 secretion by the thyroid • T3/T4 is increased in hypothyroid states because of increased T3 secretion relative to T4 secretion + higher relative decline in blood T4 levels (increased tissue 5’-deiodinase activity) 24/01/2013 Dr R B Cope 25
- 26. Thyroid Function Tests: Serum TBG = T3 resin uptake test (T3U) • This test does not measure any of the thyroid hormones, it simply provides an indication of the amount TBG present • It is called "T3" resin uptake because T3 is used in the test procedure. • The normal range varies considerable among laboratories • The test is designed so that the higher the value, the lower the amount of binding globulin (TBG) which is present. 24/01/2013 Dr R B Cope 26
- 27. Thyroid Function Tests: Serum rT3 • Serum rT3 is increased if 5’-deiodinases are inhibited • Not routinely available • rT3 increases if 5’-deiodinases are blocked because: – T4 accumulates which is subsequently converted to rT3 in the periphery – T3 accumulates which is subsequently converted to rT3 in the periphery 24/01/2013 Dr R B Cope 27
- 28. Thyroid Function Tests: Radioactive Iodine Uptake Test (RAIU) + Thyroid Scan • Determines the uptake by the thyroid of 123I by the thyroid • Extremely sensitive • Critical test if the xenobiotic is suspected of disrupting I uptake by the thyroid • Generally low uptake is an indicator of hypothyroidism (either primary or secondary) 24/01/2013 Dr R B Cope 28
- 29. Thyroid Function Tests: Radioactive Iodine Uptake Test (RAIU) + Thyroid Scan • A high uptake of tracer spread evenly in the thyroid gland is an indicator of general hyperthyroidism • An uneven spread of tracer in the thyroid gland (with either low or high areas of uptake) may mean that hyperthyroidism is caused by a nodular hyperplasia or nodular thyroid tumors. 24/01/2013 Dr R B Cope 29
- 30. 24/01/2013 Dr R B Cope 30
- 31. Nodular goiter 24/01/2013 Dr R B Cope 31
- 32. Thyroid tumor 24/01/2013 Dr R B Cope 32
- 33. Practical Use of the Thyroid Function Tests • General screening for thyroid dysfunction: at the minimum, total serum T4 + serum TSH should be performed – Both experimental + historical controls (normal ranges) are critical for interpretation – Normal ranges must be for the strain being used and the age of animals being used (and preferably developed specifically for the testing lab) • Additional tests should be included if there is any indications that the xenobiotic may result in thyroid disruption 24/01/2013 Dr R B Cope 33
- 34. Mechanisms of Thyroid Toxicity • Inhibition of thyroid hormone synthesis (primary hypothyroidism) – Inhibition of iodine uptake – Inhibition of thyroperoxidase and other organification defects • Blockage of T3 and T4 secretion (primary hypothyroidism) • Thyroid pigmentation and other changes in colloid • Increased T4 clearance associated with hepatic microsomal enzyme induction • Inhibition of 5’ deiodenases • Thyroid carcinogenesis 24/01/2013 Dr R B Cope 34
- 35. Inhibition of Iodine Uptake and Iodine Trapping • Involves blockage of or competition for the Na I symporter (NIS) – Note: NIS is also found in the salivary gland, gastric mucosa, choroid plexus, ciliary body of the eye, lactating mammary gland • Common NIS competitive inhibitors – Perchlorate (ClO4-) – Thiocyanates (SCN-) e.g. brassica-based foods, cassava etc – Pertechnetate • Sodium chlorate (NaClO3) is a common NIS inhibitor • Net result is hypothyroidism (decreased T3, T4 + increased TSH) + goiter (follicular cell hypertrophy and hyperplasia due to increased TSH and excessive thyroid stimulation) 24/01/2013 Dr R B Cope 35
- 36. Inhibition of thyroperoxidase and other organification defects • Thionamides – Propylthiouracil used to treat hyperthyroidism is the classical example – Sulfonamide antibiotics • Anilines • Substituted phenols • Can act either by inhibiting thyroperoxidase or the coupling reactions (i.e. reaction of MIT + DIT to form T3 and T4) • Humans are relatively resistant to these effects compared with rodents and dogs • Net result is hypothyroidism (primary) 24/01/2013 Dr R B Cope 36
- 37. Blockage of T3 and T4 Secretion • High doses of iodine – mode of action is uncertain • Lithium – classical side effect of the use of lithium to treat manic states is hypothyroidism and goiter 24/01/2013 Dr R B Cope 37
- 38. Thyroid Pigmentation and Colloid Abnormalities • Many xenobiotics localize and concentrate in colloid • May result in pigmentation or clumping of colloid or increased basophilic staining of colloid • Accumulation of xenobiotics in colloid may or may not disrupt thyroid function 24/01/2013 Dr R B Cope 38
- 39. Increased T3 and T4 Excretion: Hepatic Microsomal Enzyme Induction • Hepatic glucuronidation is the rate-limiting step for biliary excretion of T4 • Hepatic sulfation (primarily phenol sulfotransferase) is the rate-limiting step for biliary excretion of T3 • Induction of these enzymes results in increased T3 and T4 clearance in rats this combined with the lower thyroid economy in rats results in reduced negative feedback on the hypothalamic-pituitary-thyroid axis increased TSH increased thyroid stimulation + hypothyroidism increased incidence of thyroid hyperplasia and thyroid follicular cell neoplasia 24/01/2013 Dr R B Cope 39
- 40. Increased T3 and T4 Excretion: Hepatic Microsomal Enzyme Induction • Classical examples are phenobarbital and Ah receptor agonists (e.g. arochlors/co-planar PCBs) and pyrethrins induce UDP-GT increased glucuronidation increased rate of T4 excretion • Can also occur via activation of the AhR, CAR, PXR and PPARα xenosensor systems • Hepatic microsomal enzyme inducers also increase the uptake of T4 into the liver and biliary excretion of unconjugated T4 (presumably by upregulating membrane transporters) 24/01/2013 Dr R B Cope 40
- 41. Increased T3 and T4 Excretion: Hepatic Microsomal Enzyme Induction • Increased T4 excretion as a mechanism of disruption of the hypothalamic- pituitary thyroid axis (hypothyroidism) and thyroid follicular carcinogenesis appears to be rat specific and is regarded as not relevant to humans – Epidemiology of patients treated with barbituates for seizure disorders indicate no increased risk – Increases of serum TSH are not seen in humans with microsomal induction – Sustained abnormally high TSH levels do not appear to increase the risk of thyroid cancer in humans – Thyroid economy is much greater in humans than in rodents – The only verified cause of thyroid cancer in humans is ionizing radiation exposure (123I and similar) 24/01/2013 Dr R B Cope 41
- 42. Increased T3 and T4 Excretion: Hepatic Microsomal Enzyme Induction • Disruption of the hypothalamic-pituitary-thyroid axis and thyroid follicular tumors secondary to increased thyroid demand is an extremely common finding in rodent toxicology studies • Thyroid follicular tumors induced by this MOA in rodents is a classical example of non-genotoxic (non-mutagenic) carcinogenesis • Provided the necessary criteria are met (see below), this MOA is generally not regarded as relevant to humans 24/01/2013 Dr R B Cope 42
- 43. Human Relevance of Thyroid Follicular Cell Tumors and Disruption of the Hypothalamic-Pituitary-Thyroid Axis in Rodents • US EPA guidance documents: http://www.epa.gov/raf/publications/thyroid-follicular-cell- tumor.htm • IPCS guidance document: http://www.inchem.org/documents/harmproj/harmproj/harmpr oj4.pdf 24/01/2013 Dr R B Cope 43
- 44. Human Relevance of Thyroid Follicular Cell Tumors and Disruption of the Hypothalamic-Pituitary-Thyroid Axis in Rodents – US EPA/IPCS takes the extremely conservative stance that rodents and humans are equally sensitive to thyroid effects due to disruption of the hypothalamic-pituitary-thyroid axis unless there is chemical- specific data – However, if the MOA is clearly due to hepatic enzyme induction, the effects are regarded as not relevant to humans 24/01/2013 Dr R B Cope 44
- 45. Human Relevance of Thyroid Follicular Cell Tumors and Disruption of the Hypothalamic-Pituitary-Thyroid Axis in Rodents • US EPA/IPCS guidance documents: – Must establish the following to demonstrate the MOA: • NOT MUTAGENIC or CLASTENOGENIC or CLASSICALLY GENOTOXIC • Induction of hepatic UGT activity • increase in hepatic metabolism and biliary excretion of T4 • decrease in serum T4 half-life and concentration • increase in circulating TSH concentration • Resulting cellular thyroid hypertrophy and follicular cell hyperplasia • Appropriate temporal relationships i.e. UGT induction occurs before decreased serum T4 T½ which occurs before increases in TSH which occurs before follicular hypertrophy and hyperplasia which occurs before the tumors 24/01/2013 Dr R B Cope 45
- 46. Human Relevance of Thyroid Follicular Cell Tumors and Disruption of the Hypothalamic-Pituitary-Thyroid Axis in Rodents • US EPA/IPCS guidance documents: – KEY THINGS TO CHECK AND THINK ABOUT WHEN INTERPRETING THIS TYPE OF DATA: • Is the weight of evidence sufficient to establish a mode of action (MOA) in animals? • Can human relevance of the MOA be reasonably excluded on the basis of fundamental, qualitative differences in key events between experimental animals and humans? • Can human relevance of the MOA be reasonably excluded on the basis of quantitative differences in either kinetic or dynamic factors between experimental animals and humans? 24/01/2013 Dr R B Cope 46
- 47. Inhibition of 5’ Monodeiodinase • Classical example is FD&C Red No. 3 (eythrosine) food and cosmetic dye • The effects include: – Functional hypothyroidism and increased thyroid demand since T4 cannot be converted into the more active T3 – Increases TSH due to decreased negative feedback on the hypothalamic-pituitary-thyroid axis – Long-term stimulation of the thyroid due to increased TSH thyroid follicular hypertrophy and hyperplasia thyroid follicular neoplasia • MOA is not regarded as human-relevant 24/01/2013 Dr R B Cope 47
- 48. Case Study 1 24/01/2013 Dr R B Cope 48
- 49. Instructions and Objectives • From the data provided below: – Determine if there is evidence of thyroid abnormalities associated with the administration of this xenobiotic – Propose a MOA for any putative effects – Compose a table that provides a comparison of key events in rats versus humans for the effects you have observed in the study – Can human relevance of the MOA be reasonably excluded on the basis of fundamental, qualitative differences in key events between experimental animals and humans? Please provide a detailed justification for your answer – Can human relevance of the MOA be reasonably excluded on the basis of quantitative differences in either kinetic or dynamic factors between experimental animals and humans? Please provide a detailed justification for your answer 24/01/2013 Dr R B Cope 49
- 50. Results of Genotoxicity Studies • Ames test with and without metabolic activation – clearly negative all strains • In vitro miconucleus test - clearly negative • Chromatid exchange test – clearly negative • In vitro chromosome aberration assay – clearly negative 24/01/2013 Dr R B Cope 50
- 51. 24/01/2013 Dr R B Cope 51
- 52. 24/01/2013 Dr R B Cope 52
- 53. 24/01/2013 Dr R B Cope 53
- 54. Case Study 2 24/01/2013 Dr R B Cope 54
- 55. New Data • New studies for the xenobiotic examined in Case Study 1 have become available • The new data indicates: – The chemical concentrates in the thyroid colloid – The chemical substance is a substrate for thyroperoxidase – A highly reactive intermediate is generated in the reaction catalyzed by thyroperoxidase – The reactive intermediate has the potential to produce DNA adducts in vitro • Would you change your conclusions regarding the human relevance of the MOA of the thyroid neoplastic effects? If so, why? • What additional studies would you perform to examine the human relevance of the MOA of the thyroid neoplastic effects? 24/01/2013 Dr R B Cope 55
