Refractory periodontitis
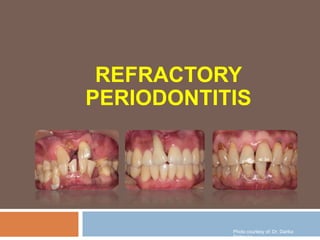
- 1. REFRACTORY PERIODONTITIS Photo courtesy of: Dr. Darika Saitawee
- 2. Refractory periodontitis periodontal disease is a chronic infectious disease of the supporting tissue of the teeth Nowadays, a large majority of patients with periodontitis respond well to conventional therapies However, a small percentage of patients respond poorly of treatment “ Refractory periodontitis ”
- 3. Characteristic of RP (Haffajee et al, 2004; Colombo et al, 2012) Poor responder or refractory of treatment AL and/or >3 sites AL >2.5 mm from the baseline visit to any monitoring visit 1 year post-therapy Refractory periodontitis Photo courtesy of: Dr. Darika Saitawee
- 4. About 10–15% of US adults are ‘refractory’ to therapy for chronic periodontitis Recently, studies suggest that these patients have investigation was to identify of this disease “ proper treatment “ Refractory periodontitis
- 5. Clinical and Laboratory Antibody response Real-Time Quantitative Polymerase Chain Reaction Human Oral Microbe Identification Microarray Diagnosis for refractory periodontitis http://www.bio-rad.com/en-us/applications-technologies/what-real-time-pcr- qpcr
- 6. Clinical and laboratory parameters Colombo et al. 1999 investigation was to use baseline clinical and laboratory parameters to distinguish subjects refractory to conventional periodontal therapy Baseline clinical microbial host parameters
- 7. 27 refractory subjects poor response after both SRP and surgery with systemic tetracycline Clinical and laboratory parameters clinic • Att gain & no site with new att loss • Gingival redness • BOP • Suppuration • Supragingival plaque accumulation • PD • AL microbial • Level of 40 subgingival texa (subging sample) • Checker board DNA-DNA hybridization Immune • Serum Ab to 85 subging species (IgG) • Checker board immunoblotting
- 10. Clinical and laboratory parameters Ab↑-odd↑ Refractory
- 11. selected by stepwise discriminant analysis: namely, number of species exhibiting serum antibody ±50 mg/ml % of S. constellatus in plaque (similar previous study Colombo 1998) % of sites with attachment level ±6 mm Clinical and laboratory parameters
- 12. Clinical and laboratory parameters Discriminant analysis using these variables provided Sensitivity 0.66 Specificity 0.92 Positive predictive value 0.80 Negative predictive values 0.85
- 13. The relatively high sensitivities, specificities and predictive values of the clinical, microbiologic and immunologic variables these tests may distinguish a relatively common form of refractory disease Refractory periodontitis subjects could be distinguished using a subset of clinical, microbiological and immunological parameters Clinical and laboratory parameters
- 14. Antibody-based diagnostic Levine et al. 2002 this study was to determine whether an elevated IgG Ab response to lysine decarboxylase, alone or with antibody to bacterial Ag and baseline clinical measurements predict the ‘refractory’ patients Gingival microbiota were found to inhibit the growth of cultured mammalian cells by depleting them of “lysine”
- 15. Eikenella corrodens and Capnocytophaga spp. Are major sources of the responsible enzyme, lysine decarboxylase Lysine decarboxylase Lysine inhibit the turnover of the most coronally situated, dentally attached (DAT) cells and JE basal cells that lie remote from capillaries cells stop proliferating causing the intermediate layer of JE to become attenuated and weaken the epithelial barrier Antibody-based diagnostic
- 16. Lysine decarboxylase activity Effect of DAT cell High - Inhibit DAT cell turnover Low - DAT cell can turnover - Maintaining oral hygiene and - Low levels of bacteria in the sulcus or pocket (retard accumulation) - Stop attachment loss Antibody-based diagnostic
- 17. IgG antibody contents to a purified antigen from Actinomyces spp. (A-Ab) Streptococcal d-alanyl glycerol lipoteichoic acid (S-Ab) related in ‘refractory’ patients Antibody-based diagnostic
- 20. Antibody-based diagnostic E. Corrodens : major sources lysine decarboxylase Similar of Colombo (1999) study
- 21. Antibody-based diagnostic A strong correlation between A-Ab and S-Ab responses was noted in ‘refractory’
- 22. Antibody-based diagnostic -Prediction of ‘refractory’ response moderate periodontitis, 2– 4mm mean att loss at baseline -Sensitivity 86.4% -Specificity 86.7%
- 23. Subjects with advanced disease need for a diagnostic test the immunoassay is proposed for use in subjects with moderate periodontitis (mean attachment loss level of 2–4mm) HKL-Ab facilitated an accurate prediction of therapeutic outcome in subjects with moderate periodontitis Antibody-based diagnostic
- 24. Real-Time Quantitative Polymerase Chain Reaction Marconcini et al. 2011 “Genetic risk factors” were proposed to influence the natural history of periodontitis The study use this technology evaluate the expression levels of leader genes in the leukocytes of refractory pt Blood samples
- 25. PCR efficiencies were calculated with a relative standard curve derived from a five cDNA dilution series in triplicate The standard curves were obtained using 1. glyceraldehyde-3-phosphate dehydrogenase (GAPDH) 2. growth factor bound protein (GRB2) 3. casitas B-lineage lymphoma (CBL) 4. nuclear factorKB1 (NFKB1) 5. REL-A (gene for transcription factor p65) Real-Time Quantitative Polymerase Chain Reaction
- 26. Real-Time Quantitative Polymerase Chain Reaction Results : levels of CBL and GRB2 were statically significant in patients with periodontitis compared to healthy patients characteristics of GRB2, CBL and NFKB1 : a specific role during inflammation and process of bone resorption
- 27. CBL oncogene part of a transforming retrovirus GRB2 signal transduction pathwayThis gene has never been associated with periodontitis Molecular studies, our hypothesis CBL played during the phase of bone resorption that can be supposed to be the acute phase of the disease GRB2 might play a central role during the inflammation process that gave the onset at the periodontitis acute phase Genes are important role in refractory chronic periodontitis develop a treatment plan reduce risk factors and to focus of therapy Real-Time Quantitative Polymerase Chain Reaction
- 28. Human Oral Microbe Identification Microarray (HOMIM) Colombo et al. 2012 investigation evaluated the post-therapy changes on the subgingival microbiota of periodontitis patients who were RP or GR as measured by using the HOMIM technique Tx: SRP + OHI + MWF + ABT (Amoxy 500 mg+Metro 250 mg)
- 29. The HOMIM methodology used a total of 400 16S rRNA-based, reverse-capture oligonucleotide probes targeting >300 bacterial taxa 16S rRNA genes were PCR amplified from DNA extracts labeled 16S amplicons were hybridized overnight to probes on the slides After washing, the microarray slides were scanned and crude data were extracted using software for microarray image analysis Human Oral Microbe Identification Microarray (HOMIM)
- 30. Human Oral Microbe Identification Microarray (HOMIM) * * *
- 31. Human Oral Microbe Identification Microarray (HOMIM)
- 32. The majority of species evaluated decreased in prevalence in both groups after treatment Species that increased or persisted in high frequency in RP but were significantly reduced in GR included Human Oral Microbe Identification Microarray (HOMIM) Bacteroidetes sp. Porphyromonas endodontalis Porphyromonas gingivalis Prevotella spp. Tannerella forsythia Dialister spp. Selenomonas spp. Catonella morbi Eubacterium spp. Filifactor alocis Parvimonas micra Peptostreptococcus sp. OT113 Fusobacterium sp. OT203 Pseudoramibacter alactolyticus Streptococcus intermedius /Streptococcus constellatus Shuttlesworthia satelles
- 33. In contrast Capnocytophaga sputigena, Cardiobacterium hominis, Gemella haemolysans, Haemophilus parainfluenzae, Kingella oralis, Lautropia mirabilis, Neisseria elongata, Rothia dentocariosa, Streptococcus australis, and Veillonella spp. associated with therapeutic success Human Oral Microbe Identification Microarray (HOMIM)
- 34. GR patients able to maintain low frequency and proportions of these organisms RP patients rapidly colonized by these species incapable of maintaining low levels of putative periodontal pathogens attributable to host impairment and/or colonization by a more virulent periodontal microbiota Human Oral Microbe Identification Microarray (HOMIM)
- 35. Haffajee et al. 2004 Clinical and microbiological changes associated with the use of combined antimicrobial therapies to treat ‘‘refractory’’ periodontitis Combine therapies SRP periodontal surgery locally delivered tetracycline at pockets ≥ 4 mm systemically administered amoxicillin (500 mg, t.i.d. for 14 days) metronidazole (250 mg, t.i.d. for 14 days) professional removal of supragingival plaque weekly for 3 months f/u every 3 months post-therapy for 2 years Treatment of refractory periodontitis
- 36. Combined antimicrobial therapies to treat ‘‘refractory’’ periodontitis - 3 mo. plaque, gingival redness, BOP, suppuration & PD ↓ - 6-24 mo. AL improved
- 37. Combined antimicrobial therapies to treat ‘‘refractory’’ periodontitis members of the green, orange and red complexes as well as some of the species in the other category were significantly elevated in the periodontitis subjects compared with the refractory subjects
- 38. Combined antimicrobial therapies to treat ‘‘refractory’’ periodontitis - No sig this time - Low level of
- 39. Combined antimicrobial therapies to treat ‘‘refractory’’ periodontitis 3 mo Actinos & orange
- 40. Combined antimicrobial therapies to treat ‘‘refractory’’ periodontitis Mean count of
- 41. conventional periodontal therapies could be successfully treated using a combination of mechanical and antimicrobial therapies combine therapies that were known to affect the subgingival microbiota and provide a beneficial clinical response (synergistic effects) Mean PD reduction was 0.83 ± 0.13 mm Mean attachment level gain was 0.44 ±0.12 mm Combined antimicrobial therapies to treat ‘‘refractory’’ periodontitis
- 42. SRP lower the biomass on the tooth surface and PD Local drug delivery directly diminish the pathogen load in any residual pockets of ≥4 mm Systemically administered amoxicillin plus metronidazole rapidly lower the level of pathogens throughout the oral cavity/poor clinical access, and to attempt to control pathogenic species that might have entered the host’s tissues Repeated professional supragingival plaque Combined antimicrobial therapies to treat ‘‘refractory’’ periodontitis
- 43. conclusion The combined antibacterial therapy was successful in controlling disease progression in refractory periodontitis Proposed reasons for ‘‘refractory’’ disease have included differences in the subgingival microbiota host response Environmental factors (smoking) All of these hypotheses were presented with the understanding that proper home care procedures and treatment of refractory patients
Hinweis der Redaktion
- lo