Alan moelleken-md-santa-barbara-spondylolisthesis
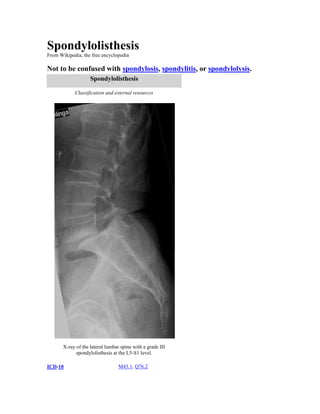
- 1. Spondylolisthesis From Wikipedia, the free encyclopedia Not to be confused with spondylosis, spondylitis, or spondylolysis. Spondylolisthesis Classification and external resources X-ray of the lateral lumbar spine with a grade III spondylolisthesis at the L5-S1 level. ICD-10 M43.1, Q76.2
- 2. ICD-9 738.4, 756.12 OMIM 184200 DiseasesDB 12318 MedlinePlus 001260 eMedicine radio/651 MeSH D013168 Spondylolisthesis is the anterior or posterior displacement of a vertebra or the vertebral column in relation to the vertebrae below. The variant "listhesis," resulting from misdivision of this compound word, is sometimes applied in conjunction with scoliosis.[1] These "slips" (aka "step-offs") occur most commonly in the lumbar spine. Spondylolysis (a defect or fracture of the pars interarticularis of the vertebral arch) is the most common cause of spondylolisthesis. This is not to be confused with a slipped disc, where one of the spinal discs in between the vertebrae has ruptured. A hangman's fracture is a specific type of spondylolisthesis where the C2 vertebra is displaced anteriorly relative to the C3 vertebra due to fractures of the C2 vertebra's pedicles. Contents 1 Classification o 1.1 Grading 2 Signs and symptoms o 2.1 Low-grade isthmic o 2.2 High-grade isthmic o 2.3 Degenerative 3 Pathophysiology 4 Treatment o 4.1 Conservative management o 4.2 Surgical 4.2.1 Low-grade isthmicspondylolisthesis 4.2.2 High-grade isthmicspondylolisthesis 5 Prognosis 6 History 7 See also 8 References 9 External links Classification Spondylolisthesis is officially categorized into five different types:. [2][3] Dysplasticspondylolisthesis is a rare congenital spondylolisthesis occurring because of a malformation of the lumbosacral junction resulting in small, incompetent facet joints.[citation needed]
- 3. X-ray picture of a grade 1 isthmicspondylolisthesis at L4-5 Isthmicspondylolisthesis is the most common form of spondylolisthesis. Isthmicspondylolisthesis (also called spondylolyticspondylolisthesis) is a common condition with a reported prevalence of 5–7 percent in the US population. A slip or fracture of the intravertebral joint is usually acquired between the ages of 6 and 16 years, but remains unnoticed until adulthood. Roughly 90 percent of these isthmic slips are low-grade (less than 50 percent slip) and 10 percent are high-grade (greater than 50 percent slip).[3] Degenerativespondylolisthesis is a disease of the older adult that develops as a result of facet arthritis and joint remodeling. Joint arthritis, and ligamentumflavum weakness, may result in slippage of a vertebrae. Degenerative forms are more likely to occur in women, persons older than fifty, and African-Americans.[3] Traumaticspondylolisthesis is very rare and results from acute fractures in various areas of the neural arch, other than the pars.[4] Pathologicspondylolisthesis has been associated with damage to the posterior elements[which?] from metastases or metabolic bone disease. These slips have been reported in cases of Paget's disease of bone, tuberculosis, giant-cell tumors, and tumor metastases.[citation needed] Grading The most common grading system for spondylolisthesis is the Meyerding grading system for severity of slip. The system categorizes severity based upon measurements on lateral X-ray of the distance from the posterior edge of the superior vertebral body to the posterior edge of the adjacent inferior vertebral body. This distance is then reported as a percentage of the total superior vertebral body length: Grade 1 is 0–25 percent Grade 2 is 25–50 percent Grade 3 is 50–75 percent Grade 4 is 75–100 percent Over 100 percent is Spondyloptosis, when the vertebra completely falls off the supporting vertebra.[citation needed] Signs and symptoms General stiffening of the back and a tightening of the hamstrings, with a resulting change in both posture and gait. A leaning-forward or semi-kyphotic posture may be seen, due to compensatory changes. A "waddle" may be seen in more advanced causes, due to compensatory pelvic rotation due to decreased lumbar spine rotation. A result of the change in gait is often a noticeable atrophy in the gluteal muscles due to lack of use.[citation needed]
- 4. MRI of L5-S1 Spondylolisthesis Generalized lower-back pain may also be seen, with intermittent shooting pain from the buttocks to the posterior thigh, and/or lower leg via the sciatic nerve. Additional symptoms may include tingling and numbness. Coughing and sneezing can intensify the pain. An individual may also note a "slipping sensation" when moving into an upright position. Sitting and trying to stand up may be painful and difficult.[citation needed] Low-grade isthmic Isthmicspondylolisthesis refers to spondylolisthesis due to degeneration of the pars interarticularis[2] When symptomatic, patients with symptomatic low-grade (<50 percent slippage) isthmicspondylolisthesis typically present with activity-related back pain and often with radicular symptoms as well. [citation needed] Patients with low grade spondylolisthesis are usually young adults (90 percent adults and 10 percent adolescents) who present with low back pain and often with radiculopathy. High grade spondylolisthesis may also present with back pain, but may also present with cosmetic deformity, hamstring tightness, radiculopathy, abnormal gait, or it may be asymptomatic.[5] High-grade isthmic
- 5. X-ray of a grade 4 spondylolisthesis at L5-S1 with spinal misalignment indicated High-grade isthmicspondylolisthesis and dysplasticspondylolisthesis are regarded as separate clinical entities from low-grade isthmic slips. High-grade slips are defined as those with greater than 50 percent forward displacement. These slips are also accompanied by a significant amount of lumbosacralkyphosis, which is forward bending of the L5 vertebral body over the sacral promontory. Rounding of the sacral body and trapezoidal deformation of L5 are also common features. High-grade slips are much rarer than lowgrade slips, representing less than 10 percent of all isthmic slips, and the vast majority present during adolescence, most during the early teenage years.[citation needed] Unlike low-grade slips, many patients present without pain. Instead symptoms like bodily deformity, neurologic abnormalities, tight hamstrings, and abnormal gait are often the reason for consultation. [citation needed] Degenerative Patients with isthmicspondylolisthesis almost universally have a neural arch defect, meaning widening of the central spinal canal at the level of the slip. In contrast, in degenerative spondylolisthesis the forward translation of the vertebral body also causes narrowing of the central spinal canal at the level of the slip, termed the "napkin ring effect" depecting the spinal canal as a series of napkin rings with one of the rings slid forward in comparison to the others. The classic symptomology of patients with symptomatic degenerative spondylolisthesis are similar to those with symptomatic lumbar spinal stenosis; either neurogenicclaudication or radiculopathy (either unilateral or bilateral radiculopathy) with or without low back pain.[citation needed] Neurogenicclaudication is thought to result from central canal narrowing that is exacerbated by the listhesis (forward slip). The classic symptoms of neurogenicclaudication are bilateral (both legs) posterior leg pain that worsens with activity, but is relieved by sitting or forward bending. Pathophysiology This section needs additional citations for verification. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged and removed. (December 2008)
- 6. In the late 1890s, several cadaver studies demonstrated the characteristic pars defect of isthmicspondylolisthesis, leading to many different theories concerning the etiology of the defect. The first theory proposed a failure of ossification during embryonic development, leading to a pars defect at birth, which then progressed to an isthmic slip after the infant began ambulating. Following the development of the Roentgenogram in 1895, population X-ray studies showed that isthmicspondylolisthesis is, in fact, quite common. There have been reports that the defect is more common among athletes who participate in sports with repeated hyperextension, such as gymnastics, ballet, and American football.[citation needed] Spondylolysis also runs in families and is more prevalent in some populations, suggesting a hereditary component, such as a tendency toward thin vertebral bone. For example, the frequency of spondylolisthesis among the Inuit has been found to be 30–50 percent, as compared with an incidence in the general population of 4–6 percent. It is theorized that the nomadic Inuit have a higher incidence of spondylolysis due to trauma acquired as infants by being carried in an amauti. While in an amauti, the baby is put into compressive extension with each step taken by the mother. [6] Pain. The cause of pain in patients with isthmicspondylolisthesis remains unclear [citation needed]. The first theory of pain production was segmental instability with excessive forward translation during flexion. however, this has not been demonstrated radiographically.[citation needed] A more contemporary theory of pain generation is excessive tension on the annulus of the inferior disc and foraminalstenosis at the level of the slip.[citation needed] However, this theory has not explained the variance in symptoms experienced by patients. Foraminalstenosis is also thought to play a role, but long-term studies on surgical outcome have shown that many patients have poor results following decompression alone. Though, most likely pain in patients with Spondylolisthesis is simply caused by the actual slippage of the disc in the spinal column. Treatment The appropriate treatment of patients with isthmicspondylolisthesis is controversial. [citation needed] For the purposes of treatment and study, patients with isthmicspondylolisthesis are usually divided into two general classes: low grade isthmicspondylolisthesis (<50 percent slip) and high grade isthmicspondylolisthesis (>50 percent slip).[5] Conservative management Patients with symptomatic isthmicspondylolisthesis are initially offered conservative treatment consisting of activity modification, pharmacological intervention, and a physical therapy consultation. physical therapy can evaluate and address postural and compensatory movement abnormalities such as hyperlordosis and hip flexor and lumbar paraspinal tightness. Other modalities such as thermal treatment, electrical stimulation and lumbar traction can help with reactive muscle spasm, but should be coupled with therapeutic exercise.[citation needed] Anti-inflammatory medications (NSAIDS) in combination with acetaminophen (Tylenol) can be tried initially. If severe radicular component is present, a short course of oral steroids such as Prednisone or Methylprednisolone can be considered. Epidural steroid injections, either interlaminarl or transforaminal, performed under fluoroscopic guidance can help with severe radicular (leg) pain. Lumbosacralorthoses may be of benefit for some patients but should be used on a temporary basis to prevent spinal muscle atrophy and loss of proprioception. Surgical Degenerative spondylolisthesis with spinal stenosis is one of the most common indications for spine surgery among older adults, and current evidence suggests that patients have much better success rates and more clinical benefit with decompression and fusion than with decompression alone.[citation needed] Low-grade isthmicspondylolisthesis Surgical treatment is only considered after at least 6 weeks and often only after 6–12 months of nonoperative therapy has failed to relieve symptoms.[citation needed] Modalities of surgical treatment include: Posterolateral fusion.
- 7. Posterolateral fusion in adult lumbar isthmicspondylolisthesis results in a significant improvement in 2-year outcomes, but the difference between surgical and nonsurgical treatment narrows with time. [7] There has been one randomized controlled trial for low-grade isthmicspondylolisthesis that compared non-operative therapy to surgery.[8][9][10] The study evaluated the severity of pain and limitations of daily function in patients with 'lumbar isthmicspondylolisthesis of any grade, at least 1 year of low back pain or sciatica, and a severely restricted functional ability in individuals 18 to 55 years of age'. At two years follow-up, patients who underwent surgery had significantly better scores for both pain and daily function. [8][9] The benefits were reduced after nine years.[10] Nevertheless, posterolateral fusion for isthmicspondylolisthesis has been one of the least controversial surgeries for spinal pathology and has consistently demonstrated good outcomes[citation needed]. The success of stand-alone posterolateral fusion for treating adolescent isthmicspondylolisthesis led several authors, including Dr Leon Wiltse and Dr Eugene Carriagee, to speculate about the effectiveness of posterolateral fusion without a decompression for adult patients with both back and leg pain. In 1989, Drs. Peek and Wiltse, et al. reported on eight cases of adults with high-grade spondylolisthesis who presented with back pain and severe radicular pain.[11] These patients were all treated with an in situ uninstrumentedposterolateral fusion and followed for an average of 5.5 years. At final follow-up, all eight patients reported complete relief of their back pain and leg pain, no patients were taking analgesics for back pain, and all patients were unrestricted with respect to work and recreational activities. The mean time to complete resolution of symptoms was 2.8 months and all patients achieved a solid fusion. No patients underwent subsequent surgery for either back pain or leg pain throughout the follow-up period. This was the first report of excellent relief of leg pain in cases of isthmicspondylolisthesis from posterolateral fusion without decompression. Fusion with decompression The addition of decompression does not appear to improve clinical outcome in addition to fusion for the treatment of low-grade isthmicspondylolisthesis in patients without serious neurological deficit. A randomized controlled trial compared fusion with a decompression to fusion without a decompression in adult cases of isthmicspondylolisthesis . The study enrolled 42 patients and showed no benefit to performing a decompression for isthmicspondylolisthesis; in fact, patients undergoing decompression had worse clinical outcomes and a higher rate of pseudoarthrosis. [12] High-grade isthmicspondylolisthesis This section needs additional citations for verification. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged and removed. (December 2008) There are several forms of surgery that have been advocated for the treatment of high-grade isthmicspondylolisthesis, including posterior interlaminar fusion, in situ posterolateral fusion, in situ anterior fusion (ALIF), in situ circumferential fusion, instrumented posterolateral fusion, and surgical reduction with instrumented posterior lumbar interbody fusion (iPLIF). Advocates of these different techniques all cite specific advantages of each approach, but they all have established risks and some are much more complication-prone than others.[citation needed] The role of surgical reduction in the treatment of high-grade isthmic is a controversial topic.[citation needed] Advocates of surgical reduction state that fusion in situ leaves too much residual deformity and impairs the natural mechanics of the lumbar spine. Patients with high-grade isthmic tend to have hyper-lordosis of the lumbar spine that compensates for the lumbosacralkyphosis associated with the severe slip and many feel that this hyper-lordosis will lead to early arthritis and low back pain. Seitsalo, et al. reported on the largest, long-term cohort of adolescents operated on for high-grade isthmicspondylolisthesis with 87 patients and mean follow-up of 14 years. Of the patients, 54 had posterior interlaminar fusions, 30 had posterolateral fusion, and 3 had an anterior interbody fusion (ALIF). The authors found a significant progression of lumbosacralkyphosis in many of their patients. They also noted that patients undergoing single-level fusions had much worse outcomes (p<0.0001) and they recommend fusing patients to L4 in virtually all cases. The authors also concluded that the clinical outcome, while much better than prior to surgery, still
- 8. left several patients with significant symptoms and progression of deformity. The authors felt that reduction may offer patients a better chance of excellent long-term outcomes.[citation needed] Reduction became feasible with the development of pedicle screws, allowing the reduction to be maintained. Several authors have published the results of reduction with pedicle screws and posterior interbody fusion with posterolateral fusion. While the improvement in percent slipped and lumbosacralkyphosis is significant, many have noted a 10–20 percent rate of nerve root injury and a few cases reports of complete caudaequina, especially with complete reduction of the deformity. While many of these injuries improve, several patients are left with permanent deficits. The clinical outcomes after reduction and instrumentation do not appear to be significantly superior to fusion in situ using modern techniques, despite the higher complication rate. It should also be noted that recurrence of deformity is common after reduction and many patients will either bend their hardware or bend at the sacrum, which is often fully segmented during adolescence. These facts have tarnished the notion of reduction and instrumentation for high-grade slips, but the technique is still utilized with theoretical benefits and some authors, particularly Dr Harry Shufflebarger, has reported both low complication rates and good clinical outcomes. Dr. Shufflebarger currently performs reductions for all high-grade slips that are referred to him and is a leading advocate of the technique. It should also be noted that the use of pedicle screw fixation is much more extensive in the US than other countries and that these surgeons are somewhat more inclined to reduce patients, at least partially, while instrumenting. The routine use of pedicle screws for one or two level pediatric fusions (not long fusions for correcting scoliosis) is without proven benefit in clinical outcome or fusion rate, but is associated with more blood loss, increased rate of nerve root injury, and more cases of reoperation.[citation needed] Until very recently,[when?] there was no data comparing the long-term outcome of reduction with instrumented fusion to an uninstrumented in situ fusion. Poussa, et al. recently [when?] published the first long-term follow-up report comparing reduction with instrumented posterolateral fusion to uninstrumented circumferential fusion in situ with a mean follow-up of 14.8 years, and concluded that reduction and instrumented fusion resulted in poorer long-term outcome than fusion in situ and that the deformity tended to recur following reduction. The increased risks and more extensive surgery associated with reduction did not translate into better outcomes or permanent correction of deformity. [citation needed] In addition to the ongoing debate of reduction versus fusion in situ, there is also new evidence emerging as to what form of fusion is most effect for eliminating symptoms and controlling deformity. This discussion of surgical technique has been much enhanced recently by the publication of a long-term follow-up study comparing three different techniques of fusion in situ for treating high-grade spondylolisthesis. The study by Helenius, et al. compared the outcomes for posterolateral fusion, anterior interbody fusion (ALIF), and circumferential fusion that is a combination of posterolateral and anterior fusion.[citation needed] Anterior fusion is a relatively new technique to spine surgery, emerging during the last two decades. It involves either a retroperitoneal or transperitoneal (through the abdomen) approach to the lumbosacral junction with mobilization of the iliac arteries and veins. The surgeon then performs a total discectomy and places a bone graft into the intervertebral space; the graft is usually either a tricortical iliac crest or a femoral ring allograft. For circumferential fusion, after completing the anterior fusion, the patient is turned and a one or two level posterolateral fusion without instrumentation is performed. Circumferential fusion can either be performed under one run of general anesthesia with patient repositioning or the procedure can be staged. Helenius, et al. followed 70 patients for a mean period of 17 years who had been treated by one of the above procedures and concluded that circumferential fusion provided the best long-term outcomes among the three techniques with excellent long-term outcomes and a low complication rate.[citation needed] Prognosis The majority of low-grade slips are asymptomatic and do not progress past a patient’s initial presentation. Prospective studies on children with low-grade slips have demonstrated that once a slip occurs, it rarely worsens, even after 40+ years of follow-up. However, high-grade slips do continue to progress in many cases and are much more likely to cause pain. One natural history study by a Swedish researcher, Saraste, found that roughly 60 percent of patients with slips greater than 15 mm (which is roughly a Meyerding
- 9. grade 2 or greater) had persistent daily symptoms, including both back pain and radiculopathy. The lowgrade slips in Saraste's study were symptomatic in only 10 percent of patients. [citation needed] Some cases do eventually progress to complete spondyloptosis and prevention of progression is the primary focus of surgery for high-grade slips. Why low-grade slips tend not to progress and why certain slips ultimately become severe is not known. There have been few long-term follow-up studies on patients with high-grade spondylolisthesis who did not undergo surgery. Harris and Weinstein reported on eleven patients after a mean follow-up of 18 years, all of which had greater than 50 percent slip and did not have surgery. Thirty-six percent of patients were asymptomatic, 55 percent of patients had relatively mild symptoms, and only one (9 percent) was disabled. The patients with mild symptoms were all able to work and participate in recreational activities, although they did need to make modifications to their lifestyle. No patient developed fulminantcaudaequina syndrome, severe neurologic symptoms, or incontinence. Fortyfive percent of patients had some neurologic abnormalities on exam, including weakness, paresthesias, and diminished deep tendon reflexes. Patient symptoms were primarily related to mild to moderate neurologic symptoms, muscle weakness, especially abdominal muscles, inactivity/deconditioning, obesity, lack of spinal mobility, and the late development of degenerative scoliosis with lateral listhesis (a deformity associated with advanced osteoarthritis of the lumbar spine). The patients in this study were a group of 21 patients who had undergone classic posterior interlaminar fusion from L4 to S1 for their severe slip with. The surgically treated patients were less symptomatic with 57 percent reporting no symptoms and no limitations, 36 percent reporting mild symptoms, and 5 percent reporting severe symptoms12. It should also be noted that the outcomes of posterior interlaminar fusions were poorer than newer posterolateral and circumferential techniques now utilized. Patients with posterior-only fusions tend to have more progression of their spondylolisthesis following surgery and more pain as well. [citation needed] History It was first described in 1782 by Belgianobstetrician, Dr. Herbinaux.[13] He reported a bony prominence anterior to the sacrum that obstructed the vagina of a small number of patients.[14] The term “spondylolisthesis” was coined in 1854 from the Greekσπονδυλος = "vertebra" and "ὁ λισθος" = "slipperiness," "a slip."[15] See also Spondylosis Failed back syndrome References 1. 2. 3. 4. 5. 6. 7. 8. Jump up ^"Natural History of Adult Scoliosis". ^ Jump up to: abWiltse, LL; Newman, PH; Macnab, I (1976 Jun). "Classification of spondylolisis and spondylolisthesis.". Clinical orthopaedics and related research (117): 23–29. PMID 1277669. ^ Jump up to: abc"Adult Spondylolisthesis in the Low Back". American Academy of Orthopaedic Surgeons. Retrieved 9 June 2013. Jump up ^http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2843565/ ^ Jump up to: ab de Loubresse CG, Bon T, Deburge A, Lassale B, Benoit M (1996). "Posterolateral fusion for radicular pain in isthmicspondylolisthesis". Clin. Orthop. Relat. Res. (323): 194–201. PMID 8625579. Jump up ^ (eds.), Behrooz A. Akbarnia, MuharremYazici, George H. Thompson (2010). The growing spine management of spinal disorders in young children. Heidelberg: Springer. pp. 325– 26. ISBN 3540852077. Jump up ^Deyo RA, Nachemson A, Mirza SK, (2004). "Spinal-fusion surgery - the case for restraint". NEJM350 (7): 722–6. doi:10.1056/NEJMsb031771. PMID 14960750. ^ Jump up to: abMöller H, Hedlund R (2000). "Surgery versus conservative management in adult isthmicspondylolisthesis--a prospective randomized study: part 1". Spine25 (13): 1711–15. doi:10.1097/00007632-200007010-00016. PMID 10870148.
- 10. 9. 10. 11. 12. 13. 14. 15. ^ Jump up to: abMöller H, Hedlund R (2000). "Instrumented and noninstrumentedposterolateral fusion in adult spondylolisthesis--a prospective randomized study: part 2". Spine25 (13): 1716–21. doi:10.1097/00007632-200007010-00017. PMID 10870149. ^ Jump up to: abEkman P, Möller H, Hedlund R (2005). "The long-term effect of posterolateral fusion in adult isthmicspondylolisthesis: a randomized controlled study". The spine journal : official journal of the North American Spine Society5 (1): 36–44. doi:10.1016/j.spinee.2004.05.249. PMID 15653083. Jump up ^ Peek RD, Wiltse LL, Reynolds JB, Thomas JC, Guyer DW, Widell EH (1989). "In situ arthrodesis without decompression for Grade-III or IV isthmicspondylolisthesis in adults who have severe sciatica". The Journal of bone and joint surgery. American volume71 (1): 62–68. PMID 2913004. Jump up ^Carragee EJ (1997). "Single-level posterolateralarthrodesis, with or without posterior decompression, for the treatment of isthmicspondylolisthesis in adults. A prospective, randomized study". The Journal of bone and joint surgery. American volume79 (8): 1175–80. PMID 9278077. Jump up ^ Newman PH (1955). "Spondylolisthesis: its cause and effect". Ann CollSurgEngl16: 305. Jump up ^Spondylolisthesis of the fifth lumbar vertebra causes pelvic abnormalities that affect the birth canal, usually requiring a Caesarean section in the case of pregnant women with the condition. This phenomenon has long been recognized by medical practitioners; see Henry Jacques Garrigues (1902). A text-book of the science and art of obstetrics. pp. 490–93. Jump up ^"IsthmicSpondylolisthesis and Spondylolysis". Beutler WJ, Fredrickson BE, Murtland A, Sweeney CA, Grant WD, Baker D (2003). "The natural history of spondylolysis and spondylolisthesis: 45-year follow-up evaluation". Spine28 (10): 1027–35; discussion 1035. doi:10.1097/01.BRS.0000061992.98108.A0. PMID 12768144. Bradford DS, Boachie-Adjei O (1990). "Treatment of severe spondylolisthesis by anterior and posterior reduction and stabilization. A long-term follow-up study". J Bone Joint Surg Am72 (7): 1060–66. PMID 2384506. Carragee EJ (1997). "Single-level posterolateralarthrodesis, with or without posterior decompression, for the treatment of isthmicspondylolisthesis in adults. A prospective, randomized study". J Bone Joint Surg Am79 (8): 1175–80. PMID 9278077. Cartlidge NE, McCollum JP, Ayyar RD (1972). "Spinal cord compression in Paget's disease". J. Neurol. Neurosurg. Psychiatr.35 (6): 825–28. doi:10.1136/jnnp.35.6.825. PMC 494187. PMID 4647855. de Loubresse CG, Bon T, Deburge A, Lassale B, Benoit M (1996). "Posterolateral fusion for radicular pain in isthmicspondylolisthesis". Clin. Orthop. Relat. Res. (323): 194–201. PMID 8625579. Fischgrund JS, Mackay M, Herkowitz HN, Brower R, Montgomery DM, Kurz LT (1997). "Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressivelaminectomy and arthrodesis with and without spinal instrumentation". Spine22 (24): 2807–12. doi:10.1097/00007632-199712150-00003. PMID 9431616. Floman Y (2000). "Progression of lumbosacralisthmicspondylolisthesis in adults". Spine25 (3): 342–47. doi:10.1097/00007632-200002010-00014. PMID 10703107. Fredrickson BE, Baker D, McHolick WJ, Yuan HA, Lubicky JP (1984). "The natural history of spondylolysis and spondylolisthesis". J Bone Joint Surg Am66 (5): 699–707. PMID 6373773. Gill GG (1984). "Long-term follow-up evaluation of a few patients with spondylolisthesis treated by excision of the loose lamina with decompression of the nerve roots without spinal fusion". Clin. Orthop. Relat. Res. (182): 215–19. PMID 6692617. Gill GG, Binder WF (1980). "Autoamputation of the first sacral nerve roots in spondyloptosis". Spine5 (3): 295–97. doi:10.1097/00007632-198005000-00014. PMID 7394667. Helenius I, Lamberg T, Osterman K, et al. (2005). "Scoliosis research society outcome instrument in evaluation of long-term surgical results in spondylolysis and low-grade isthmicspondylolisthesis in young patients". Spine30 (3): 336–41. doi:10.1097/01.brs.0000152375.13316.6a. PMID 15682016. Helenius I, Lamberg T, Osterman K, et al. (2006). "Posterolateral, anterior, or circumferential fusion in situ for high-grade spondylolisthesis in young patients: a long-term evaluation using the
- 11. Scoliosis Research Society questionnaire". Spine31 (2): 190–96. doi:10.1097/01.brs.0000194843.94071.09. PMID 16418639. Henderson ED (1966). "Results of the surgical treatment of spondylolisthesis". J Bone Joint Surg Am48 (4): 619–42. PMID 15580735. Hu SS, Bradford DS, Transfeldt EE, Cohen M (1996). "Reduction of high-grade spondylolisthesis using Edwards instrumentation". Spine21 (3): 367–71. doi:10.1097/00007632-199602010-00023. PMID 8742214. Kim YJ, Bridwell KH, Lenke LG, Rinella AS, Edwards C, Edward C (2005). "Pseudarthrosis in primary fusions for adult idiopathic scoliosis: incidence, risk factors, and outcome analysis". Spine30 (4): 468–74. doi:10.1097/01.brs.0000153392.74639.ea. PMID 15706346. Kim YJ, Lenke LG, Bridwell KH, Kim KL, Steger-May K (2005). "Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure". J Bone Joint Surg Am87 (7): 1534–41. doi:10.2106/JBJS.C.00978. PMID 15995121. Lamberg TS, Remes VM, Helenius IJ, et al. (2005). "Long-term clinical, functional and radiological outcome 21 years after posterior or posterolateral fusion in childhood and adolescence isthmicspondylolisthesis". Eur Spine J14 (7): 639–44. doi:10.1007/s00586-004-0814-1. PMID 15690214. Luhmann SJ, Lenke LG, Kim YJ, Bridwell KH, Schootman M (2005). "Thoracic adolescent idiopathic scoliosis curves between 70 degrees and 100 degrees: is anterior release necessary?". Spine30 (18): 2061–67. PMID 16166896. McGuire RA, Amundson GM (1993). "The use of primary internal fixation in spondylolisthesis". Spine18 (12): 1662–72. doi:10.1097/00007632-199309000-00015. PMID 8235847. Molinari RW, Lenke LG (2003). "Pediatric Spondylolysis and Spondylolisthesis". In Wiesel, Sam W; Frymoyer, John W; Howard S, Md An; Scott D, MdBoden; William C, MdLauerman; Lawrence G, MdLenke; Robert F, Md McLain. The Adult and Pediatric Spine: Principles, Practice, and Surgery (3rd ed.). Hagerstwon, MD: Lippincott Williams & Wilkins. ISBN 0-78173549-1. Möller H, Hedlund R (2000). "Surgery versus conservative management in adult isthmicspondylolisthesis--a prospective randomized study: part 1". Spine25 (13): 1711–15. doi:10.1097/00007632-200007010-00016. PMID 10870148. Möller H, Hedlund R (2000). "Instrumented and noninstrumentedposterolateral fusion in adult spondylolisthesis--a prospective randomized study: part 2". Spine25 (13): 1716–21. doi:10.1097/00007632-200007010-00017. PMID 10870149. Osterman K, Lindholm TS, Laurent LE (1976). "Late results of removal of the loose posterior element (Gill's operation) in the treatment of lytic lumbar spondylolisthesis". Clin. Orthop. Relat. Res. (117): 121–28. PMID 1277661. Peek RD, Wiltse LL, Reynolds JB, Thomas JC, Guyer DW, Widell EH (1989). "In situ arthrodesis without decompression for Grade-III or IV isthmicspondylolisthesis in adults who have severe sciatica". J Bone Joint Surg Am71 (1): 62–68. PMID 2913004. Poussa M, Remes V, Lamberg T, et al. (2006). "Treatment of severe spondylolisthesis in adolescence with reduction or fusion in situ: long-term clinical, radiologic, and functional outcome". Spine31 (5): 583–90; discussion 591–92. doi:10.1097/01.brs.0000201401.17944.f7. PMID 16508556. Sailhan F, Gollogly S, Roussouly P (2006). "The radiographic results and neurologic complications of instrumented reduction and fusion of high-grade spondylolisthesis without decompression of the neural elements: a retrospective review of 44 patients". Spine31 (2): 161–69; discussion 170. doi:10.1097/01.brs.0000194780.17528.6b. PMID 16418634. Schneider G, Pearcy MJ, Bogduk N (2005). "Abnormal motion in spondylolyticspondylolisthesis". Spine30 (10): 1159–64. doi:10.1097/01.brs.0000162400.06685.37. PMID 15897830. Seitsalo S, Osterman K, Hyvärinen H, Schlenzka D, Poussa M (1990). "Severe spondylolisthesis in children and adolescents. A long-term review of fusion in situ". J Bone Joint Surg Br72 (2): 259–65. PMID 2312566. Shufflebarger HL, Geck MJ (2005). "High-grade isthmicdysplasticspondylolisthesis: monosegmental surgical treatment". Spine30 (6 Suppl): S42–48. PMID 15767886.
- 12. Vogt MT, Rubin DA, San Valentin R, et al. (1999). "Degenerative lumbar listhesis and bone mineral density in elderly women. The study of osteoporotic fractures". Spine24 (23): 2536–41. doi:10.1097/00007632-199912010-00016. PMID 10626317. Vogt MT, Rubin D, Valentin RS, et al. (1998). "Lumbar olisthesis and lower back symptoms in elderly white women. The Study of Osteoporotic Fractures". Spine23 (23): 2640–7. doi:10.1097/00007632-199812010-00020. PMID 9854764. Weinstein SL (2000). "Bristol-Myers Squibb/Zimmer award for distinguished achievement in orthopaedic research. Long-term follow-up of pediatric orthopaedic conditions. Natural history and outcomes of treatment". J Bone Joint Surg Am82–A (7): 980–90. PMID 10901313. Wiltse LL (1962). "The etiology of spondylolisthesis". J Bone Joint Surg Am44–A: 539–60. PMID 14040287. SANTA BARBARA BEST SPINE AND ORTHOPEDIC DOCTORS IN CALIFORNIA 401 East Carrillo Street, Santa Barbara, CA 93101 PH 805-563-3307 FAX 805-563-0998 Attending Staff Alan Moelleken, MD Michael Price, MD Michael Kenly, MD David Lee, MD David Pires, DO Ken Nisbet, PA-C, MSPAS Jesse Jacobs, PA-C, MSPAS Darren Richards, PA-C, MSPAS Matt Ebling, PA-C, MSPAS Andrew Fairburn, PA-C Jessica Jacobs, PA-C Mitch Fallon, PA-C Andrea Lewis, LAc SANTA MARIA BEST SPINE AND ORTHOPEDIC DOCTORS IN CALIFORNIA 326 West Main Street, Suite 120 Santa Maria, CA 93458 PH 805-925-9997 FAX 805-925-9988 Alan Moelleken, MD
- 13. Michael Price, MD Michael Kenly, MD David Lee, MD David Pires, DO Ken Nisbet, PA-C, MSPAS Terry Brightwell, DC Jesse Jacobs, PA-C, MSPAS Darren Richards, PA-C, MSPAS Matt Ebling, PA-C, MSPAS Andrew Fairburn, PA-C Jessica Jacobs, PA-C Mitch Fallon, PA-C Tona Marquez, LAc BAKERSFIELD BEST SPINE AND ORTHOPEDIC DOCTORS IN CALIFORNIA 2725 16th Street Bakersfield, CA 93301 PH 661-864-1150 FAX 661-864-1145 Attending Staff Alan Moelleken, MD Michael Price, MD Michael Kenly, MD David Lee, MD David Pires, DO Tony Kim, DC Adam Sverdlin, DC Jesse Jacobs, PA-C, MSPAS Darren Richards, PA-C, MSPAS Matt Ebling, PA-C, MSPAS Andrew Fairburn, PA-C Mitch Fallon, PA-C Jen Lewis, PA-C, MSPAS Kerby Pierre-Louis, PA-C Darla Kyle, PA-C Avis Chiu, LAc
- 14. OXNARD BEST SPINE AND ORTHOPEDIC DOCTORS IN CALIFORNIA 640 South B Street Oxnard, CA 93030 PH 805-485-7042 FAX 805-485-0716 Attending Staff Alan Moelleken, MD Michael Price, MD Michael Kenly, MD Adam Sverdlin, DC Daniel Chang, DC Ken Nisbet, PA-C, MSPAS Jesse Jacobs, PA-C, MSPAS Darren Richards, PA-C, MSPAS Matt Ebling, PA-C, MSPAS Andrew Fairburn, PA-C Mitch Fallon, PA-C Kerby Pierre-Louis, PA-C Jaewoo You, LAc Darren Lisle, LAc VAN NUYS BEST SPINE AND ORTHOPEDIC DOCTORS IN CALIFORNIA 6326 Vesper Ave Van Nuys, CA 91411 PH 818-779-1500 FAX 818-779-1551 Attending Staff Alan Moelleken, MD Michael Price, MD David Lee, MD Paul Cabrera, DC Jen Lewis, PA-C, MSPAS Kerby Pierre-Louis, PA-C Jesse Jacobs, PA-C, MSPAS Jaewoo You, LAc
- 15. SANTA BARBARA BEST SPINE AND ORTHOPEDIC DOCTORS AT THE SPINE AND ORTHOPEDIC PHYSICAL REHABILITATION CALIFORNIA 119 N Milpas Santa Barbara, CA 93103 PH 805-730-1914 FAX 805-963-7550
