Pcr all aap 9.28.12 ppp
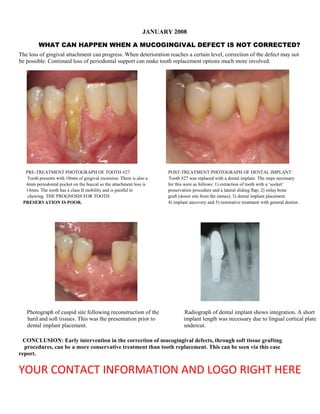
- 1. JANUARY 2008 WHAT CAN HAPPEN WHEN A MUCOGINGIVAL DEFECT IS NOT CORRECTED? The loss of gingival attachment can progress. When deterioration reaches a certain level, correction of the defect may not be possible. Continued loss of periodontal support can make tooth replacement options much more involved. PRE-TREATMENT PHOTOGRAPH OF TOOTH #27: POST-TREATMENT PHOTOGRAPH OF DENTAL IMPLANT: Tooth presents with 10mm of gingival recession. There is also a Tooth #27 was replaced with a dental implant. The steps necessary 4mm periodontal pocket on the buccal so the attachment loss is for this were as follows: 1) extraction of tooth with a ‘socket’ 14mm. The tooth has a class II mobility and is painful to preservation procedure and a lateral sliding flap; 2) onlay bone chewing. THE PROGNOSIS FOR TOOTH graft (donor site from the ramus); 3) dental implant placement PRESERVATION IS POOR. 4) implant uncovery and 5) restorative treatment with general dentist. Photograph of cuspid site following reconstruction of the Radiograph of dental implant shows integration. A short hard and soft tissues. This was the presentation prior to implant length was necessary due to lingual cortical plate dental implant placement. undercut. CONCLUSION: Early intervention in the correction of mucogingival defects, through soft tissue grafting procedures, can be a more conservative treatment than tooth replacement. This can be seen via this case report. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 2. EDUCATE YOUR DENTAL COMMUNITY ON WHY THEY SHOULD SEND THEIR PERIODONTAL & IMPLANT PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 3. FEBRUARY 2008 TREATMENT SOLUTIONS FOR THE MANDIBULAR EDENTULOUS PATIENT OPTION 1: MINI-IMPLANTS - 4 to 6 mini-implants required - provide improved retention for the denture. - based on mechanical lock of implants to bone opposed to biological integration - uncertain life-span -smallest financial investment for patient OPTION 2: IMPLANT OVERDENTURE -2-4 dental implants; can use locator abutments, ball abutments or a bar. -there still can be some movement of the denture -based on osseo-integration, so has OPTION 3: IMPLANT OVER-DENTURE WITH HADER BAR -4-6 dental implants -very high degree of retention; usually no movement during function -predictable esthetics -very high degree of success OPTION 4: FIXED IMPLANT SUPPORTED BRIDGE -6-10 dental implants -may require bone grafting -can be challenging esthetically -teeth are non-removable -largest financial investment for patient The options listed above range from least to most involved. Treatment selection depends on clinical and patient factors. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 4. REMIND YOUR DENTAL COMMUNITY ON WHY THEY SHOULD SEND THEIR PERIODONTAL & IMPLANT PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 5. MARCH 2008 Treatment of a primary periodontal, secondary endodontic lesion related to food impaction from an open contact. Radiograph and photograph reveal extensive deterioration associated with tooth #30 distal. The radiograph reveals a vertical bone defect that extended to the apex of the root. The photograph shows the periodontal probe extending down 12mm. Tooth 30 is temporized to close the open contact that had caused the periodontal damage. The tooth was determined to be non-vital by the endodontist. Flap elevation reveals the Photograph shows the bone graft Photograph shows a Bio-Gide membrane infrabony defect between teeth 30 in place. A synthetic growth placed over the bone graft. This membrane is and 31. The temporary crown has factor has been used to stimulate resorbable and provides epithelial cell been removed for better access to periodontal regeneration. exclusion to promote periodontal regeneration. the periodontal defect. Six month follow up radiograph reveals dramatic bone fill of the defect. Also seen is the root canal which helped to eliminate periodontal pathogens that had migrated into the root canal system. The area now probes 3-4mm. Differentiating between periodontal and endodontic etiology can be difficult. Radiographic and clinical evaluation can help determine if the diagnosis is 1) primary periodontal, secondary endodontic or 2) primary endodontic, secondary periodontal or 3) a combined periodontal-endodontic lesion. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 6. MOTIVATE YOUR DENTAL COMMUNITY TO SEND THEIR PERIODONTAL & IMPLANT PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 7. APRIL 2008 BENEFITS OF FLAP ACCESS IN THE TREATMENT OF PERIODONTAL DISEASE Dental calculus is mineralized, mature plaque covered on its surface with non- mineralized plaque, material alba, desquamated epithelial cells and formed blood elements. Root calculus is usually more strongly adherent to tooth surfaces than that found on enamel surfaces. Patient #1 Patient #1 The attachment of subgingival calculus is complicated by microscopic irregularities in cementum. These irregularities include cemental tears, cemental voids once occupied by Sharpey’s fibers, resorption bays and other surface cemental defects. For this reason, calculus can be very difficult to remove from root surfaces during scaling and root planing. The microbial composition of calculus provides bacterial factors that produce Patient #2 Patient #2 an inflammatory reaction in tissue. The persistent presence of inflammation is what leads to periodontal destruction and tooth loss in the susceptible patient. Numerous university studies indicate that the effectiveness of calculus removal dramatically decreases as pocket depths deepen. Patient #3 Patient #3 The photographs to the left show flap elevation of three different patients that had received scaling and root planing within the last six months. The photographs to the right show the benefits of flap elevation in allowing for visualization and access to the calculus. With direct access, more effective calculus removal can be achieved. This allows for a much improved prognosis for tooth retention. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 8. BRAND YOUR PRACTICE AS THE PREMIER PERIODONTAL & DENTAL IMPLANT PRACTICE IN YOUR COMMUNITY THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 9. MAY 2008 PERIODONTAL SITE DEVELOPMENT IN PREPARATION FOR A DENTAL IMPLANT Pre-treatment photograph Post-treatment photograph The photograph to the left shows the pre-treatment condition of tooth #10. The tooth presented with 4mm.of gingival recession, class III mobility and 7mm probing depth on the distal. The patient desired the best esthetic outcome possible. She was motivated to do whatever was necessary to achieve this result. The photograph to the right shows the completed case with a dental implant, an improved gingival margin position and a reduction in the amalgam tattoo. The black arrows show the difference in gingival margins relative to the central incisor. Without gingival augmentation, the final implant crown would look unusually tall. These radiographs show the pre- and post-treatment views. The radiograph to the left shows an apical radiolucent area and a suspicious position for the post. The radiograph to the right shows a well integrated dental implant. The above two photographs show tissue manipulation following The photograph to the left shows an improved gingival margin extraction of tooth 10. By covering the bone graft, following location. The photograph on the right shows a free gingival extraction, with a rotated pedicle flap, correction of the pre- graft to correct the amalgam tattoo following removal of the existing gingival recession could be accomplished. amalgam ‘flash’ in the tissue. CONCLUSION: HAVING THE PROPER TISSUE SUPPORT IS IMPORTANT IN ACHIEVING ESTHETIC RESULTS. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 10. FREQUENTLY REMIND YOUR DENTAL COMMUNITY WHY THEY SHOULD SEND PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 11. JUNE 2008 BIOLOGIC WIDTH The distance established by the connective tissue (1.07mm), the junctional epithelium (0.97mm) and the gingival sulcus (0.69mm). It has a combined dimension of 3.03mm. Violation of the biologic width can lead to chronic pain, chronic inflammation and unpredictable loss of alveolar bone. Pre-treatment photograph shows severely worn dentition. Gingivectomy is performed. A scalpel is used instead of a laser These short clinical crowns do not provide enough tooth since osseous recontouring is to be performed. This was determined structure for retention of planned restorations. In in the pre-treatment assessment when the alveolar crest of bone was addition, current tooth proportions (width to height ratio) sounded. The frenum has been released as well. are not conducive to an esthetic result. Flap reflection reveals alveolar crest of bone to be at the Osseous recontouring has been provided to allow for 3 mm of space cemento-enamel junction of teeth 8, 9 and 10. Black arrows from the adjusted crest of bone (black arrows) to the proposed final indicate current bone level. On teeth 6, 7 and 11, the crest of crown margin. Without this space, there is not enough room for the bone is where the final crown margins are planned. gingival attachment between the restorative margin and the crest of bone. Restorative margins too close to the alveolar crest can result in unsightly cyanotic tissue margins. Six week healing photograph shows enhanced tooth exposure. This will provide improved retention for the restorations. It will also allow for establishment of improved tooth proportions (80% width to height). The incisal edge will be extended coronally 1-2mm. The final gingival margins were probed and found to be 3mm from the alveolar crest. This will eliminate the possibility of chronic inflammation once the teeth are restored through establishment of the BIOLOGIC WIDTH. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 12. EDUCATE YOUR DENTAL COMMUNITY ON WHY THEY SHOULD SEND THEIR PERIODONTAL & IMPLANT PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 13. JULY 2008 IDEAL TREATMENT OF CERVICAL EROSION DEFECTS Combined restorative and periodontal treatment to restore lost and damaged tissue. Pre-treatment photograph shows cervical erosion of Post-treatment photograph shows restoration of both the teeth teeth 18-23. Previous restorations have failed on and periodontium. Connective tissue grafting to the cemento- several occasions. In addition, there is only 1-2mm enamel junction has restored the periodontal support and of keratinized attached tissue. This puts the teeth at increased the amount of keratinized attached tissue. Bonding risk for continued periodontal deterioration. was provided by the restorative dentist to replace the enamel. The area has been stable for 3 years. ETIOLOGY: Toothbrush abrasion is often blamed. University studies indicate causes are usually multi-factorial. *Predisposing Factors to Gingival Recession: • Anatomic narrow zone of attached gingiva • Excessive use/pressure with oral hygiene devices • Tooth malposition/thin buccal plate of bone or tissue • Periodontal diseases, including NUG and viral infections *Loss of Tooth Structure Predisposing Factors: • Erosion • • Abfraction Crown preparation • Abrasion • • Anatomic zone of exposed dentin at CEJ Combined effects • Attrition TREATMENT: Sequencing can vary. However, typically gingival grafting is provided first. This involves replacement of soft tissue support to where the cemento-enamel junction was. This allows for connective tissue fibers to re-attach to the dentin (instead of soft tissue adhesion). Following this, restorative dentistry is provided to replace the missing tooth structure. The results are typically excellent and stable over time. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 14. REMIND YOUR DENTAL COMMUNITY ON WHY THEY SHOULD SEND THEIR PERIODONTAL & IMPLANT PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 15. AUGUST 2008 ESTHETIC CROWN LENGTHENING A periodontal treatment that recontours the tissue to allow for a more esthetic tooth form. A width to height ratio of 75-80% for the crown is deemed preferable. Crown lengthening combined with restorative dentistry can remarkably improve dental esthetics. Pre-treatment photograph case #1 Post-treatment photograph case #1 Pre-treatment photograph case #2 Post-treatment photograph case #2 Pre-treatment photographs reveal the chief complaints Post-treatment photographs reveal enhanced dental esthetics of these patients: 1) Short, square shaped clinical crowns. and pleased patients. Improvement has been accomplished by: This can give an aged appearance to the patient. 1) Increasing the height to width ratio of the crowns with 2) Excessive gingival display on smiling. crown lengthening that included osseous recontouring. 3) Asymmetry between crowns for case #1. 2) Adjusting the gingival margins to follow the lip line. 4) Mal-content with the shades of the crowns in case #1 3) The restorative dentist providing esthetic crowns. and the teeth in case #2. SOME CRITICAL FEATURES IN SMILE DESIGN ARE AS FOLLOWS: 1. Incisal edge position 3. Gingival margins follow the lip line 2. Tooth form (width to height ratio of 75-80%) 4. Symmetry between the teeth YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 16. SEPTEMBER 2008 INFLAMMATION AND BONE LOSS IN PERIODONTAL DISEASE New concepts about the role of chronic inflammation as a destructive mechanism to the human body are being discovered. At a 2008 periodontal conference, information was shared by leading researchers from around the world. Inflammatory reactions involve interactions among various genes, environmental factors and chemicals from different parts of the body. The above photographs are examples of the destruction to the alveolar bone that is seen in different patients with periodontal disease when the gingival tissues are reflected. This periodontal destruction is primarily a result of the inflammatory system. The innate immune system is activated by bacterially derived factors and antigens. Inflammatory mediators, such as prostaglandins and interleukins, and enzymes, such as matrix metalloproteinases, are involved in the destruction of periodontal tissues. Eventually a cascade of events leads to osteoclastogenesis and bone loss. This occurs by altering expression levels of a protein called Receptor Activator of Nuclear factor-kappa B ligand (RANKL) on the osteoblast surface. Acquired and inherited environmental risk factors explain the susceptibility of certain individuals to periodontal disease. Although our genes do not change, the control of how certain genes are expressed in specific tissues can change substantially (EPIGENETICS) throughout our lives. Factors such as diet, stress, smoking and bacteria can modify gene expression. THE WHOLE BODY: 1. Inflammatory mediators spread throughout the body via the circulatory system. 2. Although an inflammatory response to injury is necessary, chronic diseases, such as coronary heart disease and diabetes, may develop because of unchecked inflammatory responses that have maladapted over decades. For example, the earliest changes in atherosclerosis occur in the endothelium. This can lead to a cascade of inflammatory responses, such as accumulation of monocytes and T cells, migration of leukocytes into the intima, monocyte differentiation and proliferation, and lesion and fibrous cap development. 3. Inflammation is now known to play a critical role in diseases that are not usually classified as inflammatory diseases, such as cardiovascular disease, diabetes, rheumatoid arthritis, Parkinson’s and Alzheimer’s disease. Although this conclusion is the results of many years of research, much of the knowledge has crystallized into coherent concepts only very recently. CONCLUSION: As the role of inflammation and its control in periodontal disease management are more fully understood, new prevention and treatment strategies should quickly emerge based on the concepts of blocking or resolving destructive host inflammatory pathways. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 17. FREQUENTLY REMIND YOUR DENTAL COMMUNITY WHY THEY SHOULD SEND PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 18. OCTOBER 2008 TIMING FOR THE PLACEMENT OF DENTAL IMPLANTS The decision as to when a dental implant should be placed is critical. The implant can be placed immediately after the tooth is removed (immediate implant placement) or weeks to months later (delayed implant placement). There are advantages and disadvantages to each approach. Pre-operative photograph and radiograph of tooth #8. The patient Post-treatment photograph and radiograph showing the replacement has had a frustrating 4 year history of chronic problems that have of tooth 8 with a dental implant. Seen in this view is the outstanding not been resolved. New crowns and endodontic re-treatment have shade and shape of the implant crown. Also seen is the symmetry been attempted, to no resolve. The tooth was recently diagnosed and nice adaptation of the gingival tissues. The radiograph shows a as fractured by an endodontist. The patient has high demands well integrated dental implant. The patient is pleased with the result regarding the esthetic outcome. and is pain free. This photograph shows atraumatic tooth This shows placement of the bone This shows a free gingival graft sutured in place over removal. This will help maintain soft and xenograft into the extraction socket. the bone graft. This will help to augment the soft hard tissue support. tissue ensuring symmetric gingival margins. CONCLUSION: Several treatment approaches can be selected in cases like this one. Given the history of chronic pain, it was decided to remove the tooth and not replace it right away. With this delayed approach to dental implant placement, we could 1) make sure the pain would resolve, 2) ensure a stable and healthy tissue foundation and 3) augment the soft tissue to meet the patients esthetic demands. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 19. BRAND YOUR PRACTICE AS THE PREMIER PERIODONTAL & DENTAL IMPLANT PRACTICE IN YOUR COMMUNITY THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 20. NOVEMBER 2008 RIDGE PRESERVATION Loss of labial crestal bone following tooth removal remains one of dentistry’s greatest challenges. The importance of maintaining an adequate bone volume prior to implant placement cannot be overstated. A procedure that can restore and maintain the alveolar ridge following tooth extraction is ‘ridge preservation’. Without ridge preservation, the alveolar bone will resorb from 30- 60% within 6 months. At least 1mm of vertical bone height will also be lost without ridge preservation. Photograph 3 months following extraction and ridge preservation Treatment photograph following extraction of tooth #7. The ridge shows impressive regeneration of the alveolar bone. The alveolar defect is due to years of infection. Most interesting is the thinness ridge has been restored to its original anatomy. This is the most of the buccal plate of bone and apical extent of bone loss (seen at predictable way to ensure successful dental implant integration and arrows). Without a ridge preservation this bone would resorb further restore the boney architecture. due to a lack of vascularity in the cortical layer of bone. Photograph shows Flap elevation shows Photograph shows Placement of a resorbable Suturing to obtain Photograph shows soft tissue swelling severe bone loss on the a bone xenograft in collagen membrane primary closure. vertical root fracture. associated with buccal of tooth #7. place. provides epithelial cell tooth #7. exclusion. CONCLUSION: Variables exist as far as the extent of regeneration which can be achieved with ridge preservation. Variables include 1) the extent of the initial bone defect, 2) the type of bone grafting material used, 3) surgical technique and 4) healing capability of the patient. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 21. EDUCATE YOUR DENTAL COMMUNITY ON WHY THEY SHOULD SEND THEIR PERIODONTAL & IMPLANT PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 22. DECEMBER 2008 GUIDED TISSUE REGENERATION TO PRESERVE TEETH Periodontal regeneration is the formation of new bone, new cementum and new periodontal ligament. This creates a new functional attachment apparatus over a pathologically exposed root surface, improving the prognosis for tooth retention. Photograph of tooth #6 with the gingival tissue reflected Photograph six months following the guided tissue regeneration following root surface debridement. Seen is the bone loss that procedure. Seen is the remarkable regeneration of bone; particularly wraps around to the mesial surface. Plans had been to remove the on the buccal and mesial surfaces. This has dramatically improved tooth, but with flap reflection we thought we could improve the the prognosis for tooth retention. The reason for the re-entry prognosis for tooth retention. procedure is that patient is receiving a dental implant to replace tooth #5, which was a pontic space. SURGICAL SEQUENCE: 1 2 3 4 Photograph 1: Pre-clinical view of tooth #6 shows draining fistula tract. This was after a week of antibiotics. Photograph 2: Flap elevation shows heavy calculus build up and loss of alveolar bone. Photograph 3: View following root surface debridement and antibiotic conditioning. Photograph 4: A composite bone graft of Bio-Oss and Demineralized Freeze Dried Bone was placed into the defect. The synthetic growth factor GEM21-S was used to enhance the regenerative process. A Bio-Gide membrane was placed to allow for regeneration through epithelial cell exclusion. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 23. JANUARY 2009 PROGRESSIVE GINGIVAL RECESSION The apical migration of the gingival margin can progress if left untreated. The more things decline, the less the chances for complete restoration. A classification system is present to allow predictions to be made about the degree of improvement that can be achieved. The above photographs from different patients show examples of severe gingival recession. The degree of deterioration present reduces the chances for complete root coverage. The above cases all lack attached tissue. CLASSIFICATION: Class I: Full height of papillae, recession within attached gingiva, no loss of interproximal bone; 100% coverage possible. Class II: Full height of papillae, recession at or beyond mucogingival junction, no loss of interdental bone; 100% coverage possible. Class III: Reduced papilla height; recession at/beyond the mucogingival junction, loss of interdental bone apical to the cemento- enamel junction, but coronal to the apical extent of the marginal tissue recession; Coverage only to level related to papilla height. Class IV: Gross flattened loss of papillae, interdental bone loss level to or apical to the gingival recession; Complete coverage not possible. CONCLUSIONS: 1. Early intervention is the easiest and best time to completely reconstruct a gingival defect. 2. The etiology is usually multi-factorial. Toothbrush abrasion gets blamed a lot and can be a factor. Tooth position, gingival biotype, root prominence, occlusion and plaque are other contributing factors. 3. The presence of keratinized attached tissue is very beneficial in preventing progressive gingival recession. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 24. FEBRUARY 2009 CORRECTION OF MUCOGINGIVAL DEFECTS THROUGH GINGIVAL GRAFTING Creating gingival tissue reduces the likelihood of further recession. Gingival grafting also helps cover exposed roots, enhances the appearance of teeth and protects roots from decay and sensitivity. Pre-treatment patient #1 Post-treatment patient #1 Pre-treatment patient #2 Post-treatment patient #2 Pre-treatment photographs show the following: Post-treatment photographs show: 1) Gingival recession ranging from 2-5mm 5mm (black 1) Complete root coverage and restoration of gingival arrows). tissues. 2) Very thin zone of attached tissue. 2) Increased zone of attached tissue has been provided This puts the teeth at risk for continued periodontal (red arrows). This strengthens the gingival attachment. deterioration and possible loss. The restoration of gingival tissue has improved the prognosis for tooth retention significantly. CONCLUSIONS: 1. Early intervention is the easiest and best time to completely reconstruct a gingival defect. 2. The etiology is usually multi-factorial. Toothbrush abrasion gets blamed a lot and can be a factor. Tooth position, gingival biotype, root prominence, occlusion and plaque are other contributing factors. 3. The presence of keratinized attached tissue is very beneficial in preventing progressive gingival recession. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 25. FREQUENTLY REMIND YOUR DENTAL COMMUNITY WHY THEY SHOULD SEND PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 26. MARCH 2009 PERIODONTITIS ASSOCIATED WITH A MEDICATION Many medications can cause gingival hyperplasia as a side effect. The hyperplastic tissue can trap plaque. This retained plaque can lead to periodontitis or other inflammatory related medical conditions. PRE-TREATME PATIENT #1 POST-TREATMENT PATIENT #1 PRE-TREATMENT PATIENT #2 POST-TREATMENT PATIENT #2 Pre-treatment photographs show medication induced Post-treatment photographs show restored gingival health. Treatment gingival hyperplasia. Bleeding on probing was present. consisted of: 1) Using alternative medications with the consent of the Calculus and plaque were present subgingivally. physicians, 2) Gingivectomy with scaling and root planing and 3) Oral hygiene instruction BLOOD PRESSURE MEDICATIONS ANTI-CONVULSANT IMMUNOSUPPRESSANTS Generic Name (Trade Name) Generic Name (Trade Name) Generic Name (Trade Name) Generic Name ( Trade Name) Diltiazem (Cardizem) Nimodipine (Nimotop) Phenytoin (Dilantin) Cyclosporine-A (Sandimmune) Felodipine (Plendil) Nisoldipine (Syscor) Isradipine (Prescal) Nitrendipine (Bayotensil) Nifedipine(Procardia, Verapamil (Calan) Adalat, Tenif) YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 27. EDUCATE YOUR DENTAL COMMUNITY ON WHY THEY SHOULD SEND THEIR PERIODONTAL & IMPLANT PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 28. APRIL 2009 DIABETES AND PERIODONTAL DISEASE Diabetic patients are three to four times more likely to develop chronic periodontal infections. The patient is a 22 year old female with type I diabetes. She presents Due to the severity of deterioration present, periodontal tooth with the chief complaint of “difficulty eating due to looseness of her preservation procedures would have had a poor long term upper front teeth.” She reports that her blood sugar levels have been prognosis. The patient was interested in a definitive treatment. high for several months. Probing depths on the anterior teeth ranged An incredible amount of calculus accumulation is present on from 6-12mm with bleeding upon probing and exudate expressed extracted teeth 7-10. The patient understood that eliminating from teeth 8 and 10. The teeth had a class III mobility. infection from her mouth would help to control her diabetes. The patient reports that she has had several “deep cleanings” over the last several years. The radiograph to the left reveals severe bone loss. It is amazing to see this amount of bone loss in a 22 year old. Periodontal infections can impair the ability of the body to process insulin, which can make diabetes more difficult to control. In addition, a periodontal infection may be more severe in a diabetic patient than in someone without diabetes. It is important for diabetic patients to have their periodontal diseases treated to control or eliminate the infection as one more way to achieve optimal control of their blood sugar levels. In the early stages of periodontal diseases, treatment usually involves scaling and root planning to remove plaque and tartar. More advanced cases may require additional treatment combined with antibiotics. Earlier intervention, with more complete treatment, in the above case may have saved the patient’s teeth. The link between diabetes and periodontal disease is a two- way street. University studies indicate that periodontal treatment can improve blood sugar levels in diabetic patients, and may decrease their need for insulin. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 29. MAY 2009 COMMON QUESTIONS ABOUT PERIODONTAL DISEASE Periodontitis is an infectious disease and is manifested as local inflammation of the periodontium. The above photograph and radiograph show severe periodontal destruction between teeth 18 and 19. The bone loss extends all the way to the apex of the distal root of tooth 19. The etiologic agent was calculus that wrapped around the root surface. The patient has received regular ‘cleanings’ twice a year. WHAT CAUSES PERIODONTAL DISEASE? Research over the past 30 years has added to our understanding of the pathogenesis of periodontal disease. Bacteria produce toxins that pass through the epithelial attachment triggering the immune response. White blood cells, particularly neutrophils, come to the area to phagocytize the bacteria , destroying healthy connective tissue in the process. Other immune cells then trigger osteoclasts to destroy the bone surrounding the tooth. DOES PERIODONTAL DISEASE AFFECT SYSTEMIC HEALTH? The relationship between periodontal disease and systemic health has been well recognized through epidemiologic studies during the last decade. Patients with periodontal disease have a higher incidence of cardiovascular diseases and strokes that are exemplified by increases in peripheral white blood cell count and C-reactive protein. Many of the diseases associated with periodontal disease are also considered to be systemic inflammatory disorders, including cardiovascular disease, diabetes, rheumatoid arthritis, chronic kidney disease and even certain forms of cancer, suggesting that inflammation itself may be the basis for the connection. WHAT ARE TREATMENT OPTIONS FOR PERIODONTAL DISEASE? The goal of periodontal treatment is to eliminate the destructive bacteria (plaque and calculus) from above and below the gum line. The best treatment approach is determined by the depth of bacterial penetration. An additional goal of periodontal treatment is to reduce pocket depths so that patients can be effective with their home care. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 30. BRAND YOUR PRACTICE AS THE PREMIER PERIODONTAL & DENTAL IMPLANT PRACTICE IN YOUR COMMUNITY THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 31. JUNE 2009 eplacement of a worn and deteriorated dentition with an implant supported over-denture Pre-treatment photograph shows severely decayed teeth Post-treatment photograph shows the implant supported over- with periodontal involvement as well as missing posterior denture in place. Health, esthetics and function for the patient have teeth. The prognosis for preserving these teeth is poor. been greatly improved. The patient is very pleased with the results. The long term prognosis for this treatment is excellent. View of locator abutments in place with View of the inside of the over-denture These are the locator inserts. The blue insert the prosthesis removed. Locators are with locator inserts. One of the inserts has a retentive capacity of 1.5 pounds, the attached to dental implants that are needed to be removed because the pink 3.0 pounds and the clear, 5.0 pounds. firmly integrated in the jaw bone. retention was so strong that the patient For example, the use of 4 dental implants could not remove the prosthesis for with locators and the clear male inserts can cleansing. offer a retention of 20 pounds. CONCLUSION: The standard of care for an edentulous patient is to have a minimum of two dental implants in the mandible. With the above patient, the long term prognosis with dental implants was felt to be better than preserving worn and deteriorated teeth. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 32. FREQUENTLY REMIND YOUR DENTAL COMMUNITY WHY THEY SHOULD SEND PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 33. JULY 2009 FURCATIONS Maxillary molars are statistically the first teeth lost due to periodontal disease. Root anatomy and poor access for both home care and professional treatment are the main factors for early loss of these teeth. -These photographs depict maxillary molar teeth lost due to deterioration of periodontal support. This deterioration was due to calculus accumulation that could not be accessed and removed. Calculus in the furcation becomes more difficult to remove as the defect advances. -Bowers (1979) reported that 81% of all furcation entrance diameters measure < 1mm and 58% < .75mm. Since commonly used curettes have blade face widths ranging from .75 to 1.10 mm, it is unlikely that proper instrumentation of furcations can be achieved with curettes alone; due to INACCESSIBILITY of the area. This issue can be seen in the photograph on the right. CLASSICIFATION SYSTEM: A variety of classification systems exist. One of the more common classifications is the ‘Hamp’ system which divides furcation invasion into 3 grades of severity: Degree I: Horizontal loss of periodontal tissue support < 3mm. Degree II: Horizontal loss of periodontal tissue support > 3mm but not encompassing the total width of the furcation. Degree III: Horizontal through-and-through destruction of the periodontal tissue in the furcation. SIGNIFICANCE OF A CLASSIFICATION SYSTEM: Teeth with more extensive furcation invasion are at greater risk for continued deterioration and future loss. In addition, the prognosis for treatment solutions worsen as the furcation deepens. A variety of treatments are available involving flap procedures that improve access to the furcation. EARLY TREATMENT, THAT IS SUCCESSFUL, IS THE BEST WAY TO PRESERVE MOLAR TEETH. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 34. AUGUST 2009 A STAGED APPROACH TO SUCCESSFUL AND ESTHETIC DENTAL IMPLANT THERAPY Pre-treatment photograph and radiograph of tooth #9 shows Post-treatment photograph and radiograph show the the following: 1) Marginal gingival inflammation, 2) Short integrated dental implant one year following the staged root that shows evidence of apical changes. Clinically the approach. Symmetry of gingival margins, crown shape and tooth has a class II mobility and there is chronic pain. shade provide for an esthetic result that the patient is quite pleased with. SURGICAL SEQUENCE FOR EXTRACTION AND RIDGE PRESERVATION: Photo 1: Atraumatic and flapless extraction of tooth #9. Photo 2: Following the extraction, the socket is explored with a periodontal probe. A bone defect is detected and can be seen at the end of the periodontal probe (arrow). Placement of an immediate implant here would be risky. Photo 3: Shows condenser compressing bone graft into the 1 2 3 extraction socket. Mild compression is provided to allow for vascularization. Photo 4: View following fill of extraction socket with bone graft. The bone graft material is a xenograft. Photo 5: Placement of a resorbable collagen membrane allows regeneration of the extraction socket. Photo 6: View of deteriorated root and calculus below the 4 5 6 crown margin. The dental implant was placed 3 months following tissue maturation and then allowed to integrate for 3 months. CONCLUSION: The timing of the placement of a dental implant is an important treatment planning decision. It is typically more predictable to have healthy, stable and sufficient soft and hard tissue. A staged approach allows for more control of each step. Higher success rates and more esthetic outcomes often can be achieved with this approach. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 35. SEPTEMBER 2009 PRESERVING TEETH THROUGH GINGIVAL GRAFTING Pre-treatment photograph of tooth #9 shows gingival Post-treatment photograph of tooth #9 shows complete root recession of 3mm. There is calculus above the class V coverage and an increase in attached tissue. The frenum pull has restoration. There is an aberrant frenum present along with also been reduced and a connective tissue graft was provided. gingival inflammation. These are all risk factors for Treatment has improved the prognosis for tooth retention and the progressive periodontal deterioration. patient is quite pleased with the improved appearance. IF GINGIVAL RECESSION PROGRESSES, IT CAN REACH A POINT WHERE REPARATIVE EFFORTS ARE NOT PREDICTABLE. A FEW EXAMPLES OF GINGIVAL RECESSION DEFECTS THAT HAVE PROGRESSED TOO FAR ARE SEEN BELOW: CONCLUSION: GINGIVAL GRAFTING IS MUCH LESS INVOLVED AND MORE PREDICTABLE WHEN THE DETERIORATION IS LESS SEVERE. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 36. EDUCATE YOUR DENTAL COMMUNITY ON WHY THEY SHOULD SEND THEIR PERIODONTAL & IMPLANT PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 37. OCTOBER 2009 PERIODONTAL DISEASE IS TYPICALLY ASYMPTOMATIC Many patients lose teeth that could have been saved because periodontal disease typically does not hurt. It can be challenging to educate patients about their risk of progressive periodontal destruction when they are unaware of an existing problem. A visual aid, such as the case below, can be helpful as a communication tool, in motivating patients about the benefits of periodontal treatment. These photographs are of a 55 year old female that presented to our office with concerns about loosening of tooth #10. The mobility of this tooth bothered her and was tender particularly while eating. Clinical examination revealed probing depths up to 13mm, gingival recession of 2-3mm, bleeding and exudate on probing and a class III mobility. Her dental history indicated that she was consistent with cleanings twice a year at her dentist’s office. She remembers being told by her dentist, years prior, that she needed to see a periodontist about tooth #10. At the time, the patient reports that she did not perceive a problem because there was no pain and declined the referral. By the time the patient came to our office, it was too late to save the tooth. She was informed that because of the extent of deterioration present, procedures to try to preserve the tooth would have a poor prognosis. The patient realized that if she had seen a periodontist at an appropriate time, she could have preserved her tooth. The photograph in the middle shows the extracted tooth. Please notice the incredible accumulation of calculus present. The calculus serves as a matrix into which plaque is retained. Plaque initiates inflammation that results in bone loss and other systemic health problems. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 38. NOVEMBER 2009 THE ONLAY BONE GRAFT A predictable treatment to increase the bone volume in preparation for dental implant tooth replacement. Pre-treatment photograph shows missing teeth 5 and 6. Tooth The photograph and radiograph reveal the final dental implants in place. 7 is too weak to serve as an abutment for a bridge. This Restoration of form and function has been achieved. The patient is thrilled with photograph shows how deceptive the clinical view can be the results. regarding the buccal-lingual thickness of bone availability. Surgical sequence: 1 2 3 4 Photograph 1: Flap elevation reveals a ridge width of 3mm. This is too narrow to properly contain the dental implants. The arrows point to the extreme thinness of the present ridge of bone. Photograph 2: Shows adaptation of onlay bone graft and stabilization with three Memfix screws. Intimate adaptation is critical. The donor site was the ramus region of the mandible. Photograph 3: Five months following bone grafting, the donor bone has fused to the recipient site. The bone is now of sufficient width to contain the dental implants. Slight resorption of the bone is evident with screw thread exposure. Once the bone is stimulated with the functioning dental implants, this resorptive process will stop. Photograph 4: Shows the dental implants in place surrounded by a solid base of bone. When there is not sufficient bone around the the dental implants, their survival is jeopardized. Note the increased thickness of bone present. CONCLUSION: IT IS IMPORTANT TO BE AWARE OF THE QUALITY AND QUANTITY OF BONE PRESENT PRIOR TO PLACING DENTAL IMPLANTS. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 39. FREQUENTLY REMIND YOUR DENTAL COMMUNITY WHY THEY SHOULD SEND PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 40. DECEMBER 2009 WHAT IS PERIODONTAL REGENERATION? The ultimate goal of periodontal therapy is replacement of the lost tooth attachment apparatus and a return to pre-disease architecture. Guided tissue regeneration allows this to happen. The following photographs demonstrate how periodontal regeneration re-grows the lost bone support. Flap elevation shows an infrabony defect associated with The above photograph shows the remarkable regeneration of tooth #18 that extended down 9mm. The defect was the bone support for the tooth. This re-entry procedure was initiated by calculus primarily along the distal root performed 8 months following the initial treatment. The surface. prognosis for tooth retention has been greatly improved. With flap elevation, access to the calculus could be Without the guided tissue regeneration procedure, the defect achieved. The area was thoroughly debrided and treated would have remained. The area would have been susceptible with tetracycline. A bone graft was then placed into the to further plaque accumulation into the defect. The presence defect mixed with a growth factor to enhance the of a periodontal pocket puts the tooth at increased risk of regenerative process. A resorbable membrane was also loss. placed to allow for regeneration through epithelial cell exclusion. -A large case series study using guided tissue regeneration in combination with root conditioning and demineralized freeze dried bone allograft showed significant gains in clinical attachment level in a variety of furcation and infrabony horn RG, McClain PK, Combined osseous grafting, root conditioning and guided tissue regeneration, Int J Periodontics Restorat 34, 1988. A subsequent study confirmed that the regenerated results were stable over five years. McClain PK, Schallhorn RG, Long-term assessment of combined osseous composite grafting, root conditioning, and guided tissue regeneration, Int J Periodontics Restorative Dent 13:9-27, 1993. MULTIPLE UNIVERSITY STUDIES SHOW THE BENEFITS OF GUIDED TISSUE REGNERATION IN PRESERVING TEETH. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 41. REMIND YOUR DENTAL COMMUNITY ON WHY THEY SHOULD SEND THEIR PERIODONTAL & IMPLANT PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 42. JANUARY 2010 LIMITATIONS OF SCALING AND ROOT PLANING Scaling and root planing is very difficult. Open flap access through periodontal treatment dramatically improves access and visualization (as can be seen in the photographs below) for the removal of calculus. The above photographs show different patients who had received scaling and root planing. At the re-evaluation appointment, incomplete healing was noted. The patient was then referred to our office for phase II periodontal treatment. The continued presence of calculus makes teeth susceptible to further periodontal deterioration and future loss. UNIVERSITY RESEARCH STUDIES INDICATE IT IS DIFFICULT TO REMOVE CALCULUS Teeth were extracted after treatment and evaluated with a microscope. With this microscope, the researchers could see the amount of calculus remaining on the root surfaces. The results of this study, for various pocket depths, are as follows: POCKET DEPTH SCALED ONLY FLAPPED AND SCALED 1-3mm 86% calculus free 86% calculus free 4-6mm 43% calculus free 76% calculus free deeper than 6mm 32% calculus free 50% calculus free “Scaling and root planning with and without periodontal flap surgery.” J. Clin Perio 3/86 CONCLUSION: It is difficult to remove calculus from root surfaces. The residual calculus following scaling and root planing is not a reflection of a lack of skill by the dentist or hygienist. The residual calculus is due to the tenacious adherence of calculus to root surfaces and inability to visualize it with the tissues in place. OPEN FLAP ACCESS CAN DRAMATICALLY IMPROVE ACCESSIBILITY AND VISIBILITY. The removal of calculus increases the prognosis for tooth retention through elimination of an etiologic factor. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 43. EDUCATE YOUR DENTAL COMMUNITY ON WHY THEY SHOULD SEND THEIR PERIODONTAL & IMPLANT PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 44. FEBRUARY 2010 INFLAMMATION AND ITS CONSEQUENCES ON SYSTEMIC HEALTH Periodontal infections are common inflammatory disorders caused by the bacteria inhabiting the biofilm of the dental plaque. Studies have suggested that periodontal infections may constitute an independent risk factor for 1) coronary artery disease, 2) pregnancy complications, including pre-term birth, lower birth weight 3) poor metabolic control in diabetes and 4) respiratory disease. Moreover, emerging associations have been described linking periodontitis and kidney disease, rheumatoid arthritis and pancreatic cancer. The above three photographs show different patients with gingival inflammation of varying degrees. Inflammation is the host’s response to an irritant. Dental plaque is a bio-film that initiates a series of events that not only leads to periodontal disease but can affect a patient’s general well-being. THE SEQUENCE OF EVENTS LEADING TO CORONARY ARTERY DISEASE: BIOFILM BACTEREMIA INFLAMMATORY RESPONSE ELEVATED C-REACTIVE PROTEIN VASCULAR EFFECTS BIOFILM: Is found floating on lakes, in plumbing lines, on the edges of vases, and on top of rivers and ponds. Biofilms grow in stacks with different types of bacteria. There is an order to the stacking of the bacteria as well as communication between the different layers. A slimy matrix forms on top of the bacteria shielding them. The biofilm in the gingival crevice is massive. There are between 10 million and 1 billion bacteria in the gingival crevice depending on the depth of the pocket. BACTEREMIA: Direct opening through the inflamed sulcular tissue allows bacteria to enter the general circulation. INFLAMMATORY RESPONSE: Cytokines, PMNs, B-cells and T-cells are produced as a result of the bacteremia. Enzymes are also produced such as: COLLAGENASE (destroys collagen); GELATINASE (hydrolyses gelatin); ELASTASE (breaks down proteins) and PROTEASE (breaks down proteins) C-REACTIVE PROTEIN (CRP): Produced by the liver as part of the normal immune system response to injury, inflammation and infection. CRP participates in the development of clots and plaques that lead to an increased risk of heart attacks and strokes. Women with elevated CRP have a seven times increased chance of a cardiovascular event. Periodontal disease increases CRP levels. Periodontal treatment reduces CRP levels. CONCLUSION: MULTIPLE STUDIES SHOW PERIODONTAL DISEASE TO BE A SIGNIFICANT RISK FACTOR FOR CORONARY ARTERY DISESAE. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 45. MARCH 2010 Improving dental health, function and esthetics through replacement of a diseased and deteriorated dentition with an implant supported over-denture Pre-treatment photograph shows an un-esthetic smile. Post-treatment photograph show improved esthetics. Retracted view shows multiple missing View of locator abutments in place with View of the inside of the over-denture teeth as well as severe damage to the the prosthesis removed. Locators are with female components. Female remaining teeth. The palate was very attached to dental implants that are components come in retentive strengths flat and there was minimal firmly integrated in the jaw bone. The of 1.5 pounds (blue), 3.0 pounds (pink) vestibular depth present. Both of dental implants were placed at the time and 5.0 pounds (clear). The above these anatomic features make of extractions (immediate implant example shows 4 blue components in retention of a traditional prosthesis placement). Treatment time for this place. These can be changed out to meet quite challenging. patient was 3 months. the patient’s retention requirements. CONCLUSION: The patient is very pleased with the results. Implant supported over- dentures are an excellent way to improve health, function and esthetics. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 46. FREQUENTLY REMIND YOUR DENTAL COMMUNITY WHY THEY SHOULD SEND PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 47. APRIL 2010 WHAT IS AN ATLANTIS ABUTMENT? A computer aided design/ computer aided machined (CAD/CAM) patient specific abutment. This custom made abutment is designed with the final tooth shape in mind, for outstanding function and esthetics. It is made from a Virtual Abutment Design software computer program. These abutments can be fabricated for the majority of dental implant systems. Atlantis patient-specific abutments are designed and fabricated to look like natural prepared teeth. Photograph shows a stock abutment on a Photograph shows an Atlantis abutment. This abutment model. This abutment is basically a one size fits has been designed and fabricated to specifically fit the all situations concept. space and tissue profile for this patient. Atlantis abutments can be made from a variety of materials depending on the clinical situation. Seen above are zirconia, titanium and a gold shaded titanium abutments. Advantages and disadvantages exist for each of these materials. CONCLUSIONS: ATLANTIS ABUTMENTS PROVIDE THE FOLLOWING ADVANTAGES: 1. Eliminates the need for ordering products, maintaining inventory and chair-side modification. 2. Patient specific shapes for the ideal emergence. 3. Variety of materials available depending on the clinical situation. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 48. BRAND YOUR PRACTICE AS THE PREMIER PERIODONTAL & DENTAL IMPLANT PRACTICE IN YOUR COMMUNITY THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 49. MAY 2010 CRESTAL BONE STABILITY AROUND DENTAL IMPLANTS IS QUITE BENEFICIAL In the past, it was acceptable for dental implants to lose 1.5mm of bone from the top of the crest, and 0.2mm during each subsequent year. This bone loss could become problematic. Today, dental implants have design features which can minimize crestal bone loss. This results in improved health, esthetic and functional stability. The radiographs to the left are examples of two patients who have lost crestal bone around dental implants that were placed in 1997. The red arrows point to where the bone level was at the time of dental implant insertion. The black arrows point to the current reduced bone level. The photograph and radiograph to the left is an example of a patient who had the dental implant placed in 2008. The radiograph shows crestal bone loss. The patient reports pain and a foul taste associated with the implant. The tissue above the implant is inflamed and exudate can be expressed from the implant sulcus. Successful long term treatment will be challenging. This is an example of a dental implant that has had no crestal bone loss since the dental implant was placed 7 years previously. This provides for stability in terms of health, function and esthetics. CONCLUSION: Maintenance of the crestal bone around dental implants is preferred. This can be accomplished with the use of a dental implant that has specific design. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 50. JUNE 2010 STABILITY OF GINGIVAL GRAFTING Practitioners and patients often inquire about the stability of gingival grafting. For gingival recession defects with Class I and Class II type defects the prognosis is good for correction of the defect and a halt to progressive deterioration. PRE-TREATMENT PHOTOGRAPH: 6 MONTH POST-TREATMENT PHOTOGRAPH: The patient and the orthodontist are quite concerned about Photograph shows the initial healing to be adequate. progressive gingival recession on tooth #25. Note The root surface has been covered, the frenum pull the lack of attached tissue and 5mm of gingival eliminated, and a band of keratinized attached tissue is recession. There was also an aberrant frenum pull. present. This will improve the long term prognosis for tooth retention. 12 YEAR FOLLOW UP PHOTOGRAPH: The periodontal tissues are within normal limits. There is a broad band of attached tissue that is firmly attached to the root surface and alveolar bone. Probing depths are 2mm. CONCLUSION: If a patient has less than 1mm of attached gingiva on a tooth and is having active recession, gingival grafting has a high predictability for success. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 51. JULY 2010 ESTHETIC CROWN LENGTHENING AND RESTORATIVE DENTISTRY This treatment plan involves periodontal recontouring followed by restorative dentistry. This two phased approach can dramatically enhance dental esthetics. pre- treatment patient 1 post-treatment patient 1 pre-treatment patient 2 post-treatment patient 2 pre-treatment patient 3 post-treatment patient 3 pre-treatment patient 4 post-treatment patient 4 The pre-treatment photographs seen above are patients who wanted to improve their smiles. Complaints ranged from asymmetry (uneven teeth for patient 1) to an aged appearance due to worn teeth (patient 2). Patients 3 and 4 did not like their “gummy smile” amongst other things. -Esthetic crown lengthening was performed by Dr. Warshawsky to: 1) Improve tooth form (width to length ratio of 80%): Creates longer teeth which look more youthful. 2) Establish biologic width (reduces chances of marginal inflammation): Places osseous crest 3mm from proposed final restorative margin. 3) Create gingival symmetry (enhances esthetics). 4) Allow gingival margin to follow the upper lip. -Restorative treatment was provided to improve the shade and shape of the teeth. This phase of the treatment was provided by local dentists. CONCLUSION: To achieve an optimal esthetic result, correction of the gummy smile, asymmetric gingival margins and short teeth are important considerations. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 52. EDUCATE YOUR DENTAL COMMUNITY ON WHY THEY SHOULD SEND THEIR PERIODONTAL & IMPLANT PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 53. AUGUST 2010 PRESERVING TEETH THROUGH THE REMOVAL OF CALCULUS The gingival appearance can be misleading in regards to the amount of calculus present beneath it. and it’s tenacity . The continued presence of calculus leads to tooth loss in the susceptible patient. Furthermore, the removal of calculus from root surfaces can be challenging due to the lack of visualization Bone loss !! Patient 1: Photograph shows the gingival Tissue flap reflection on the buccal and palatal, respectively, shows tissues around teeth 13 and14. Minimal gingival Calculus (yellow arrows) along the root surface of tooth 14. The associated inflammation is present due to good home care bone loss (black arrows) should be noted. Continued loss of bone due to the currently and bi-annual dental prophylaxis presence of calculus would lead to tooth loss. appointments. No more calculus !!! Patient 2: Photograph shows the gingival tissues Tissue reflection shows the presence of calculus on the around teeth 22 through 24. Minimal gingival root of tooth 23. The photograph on the far right shows inflammation is present due to good home care currently. the benefits of flap access in the removal of the primary No obvious indications are present of what lays beneath etiological factor in periodontal disease. the tissue. CONCLUSION: Tissue flap elevation can allow for improved visualization of calculus for more effective removal. This helps to preserve teeth. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 54. FREQUENTLY REMIND YOUR DENTAL COMMUNITY WHY THEY SHOULD SEND PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 55. SEPTEMBER 2010 GUIDED TISSUE REGENERATION: 18 MONTH FOLLOW UP Periodontal regeneration is the formation of new bone, cementum and periodontal ligament. This creates a new functional attachment apparatus over a previously pathologically exposed root surface. This case report demonstrates long term maintenance of regeneration. Pre-treatment Post-treatment Pre-treatment radiograph of tooth# 7 on the left shows severe bone loss (area between the red arrows) and calculus (yellow arrow). This condition gives the tooth a poor prognosis. The follow up (18 months following treatment) radiograph shows complete bone fill and no calculus. THE PROGNOSIS IS NOW GOOD FOR TOOTH PRESERVATION. SURGICAL SEQUENCE: Pre-treatment photograph of tooth Flap elevation reveals the bone Photograph after Photograph reveals the bone graft #7 shows periodontal probe defect and associated debridement of the root placed into the defect. The extending down 9mm. following destructive calculus. The surface and bone defect. synthetic growth factor GEM21-S anesthesia. The tooth has been black arrow points to the Flap reflection allows for was used to enhance the temporized to allow for: 1) ledge of calculus that was the best access for such regenerative process. Following Closure of the open contact that led buried sub-gingivally; the treatment. Also seen is this a barrier membrane was placed to the periodontal destruction (so yellow arrow points to the the crater like bone loss that and the tissue sutured. The food does not impact into the bone loss. The patient reports extended 1/3 down the root temporary crown was then re- surgery site) 2) Better access for a history of root planing that surface. cemented. successful periodontal treatment. could not reach the calculus. CONCLUSION: Guided Tissue Regeneration is the ideal treatment for teeth when they have lost support due to periodontal disease. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 56. REMIND YOUR DENTAL COMMUNITY ON WHY THEY SHOULD SEND THEIR PERIODONTAL & IMPLANT PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 57. OCTOBER 2010 CONSERVATIVE MANAGEMENT OF A PATIENT TAKING A BISPHOSPHONATE, WITH A FRACTURED ROOT Aredia is an intravenous bisphosphonate used in the treatment of osteoporosis, cancer and or multiple myeloma. Aredia has a dangerous side effect, jaw osteonecrosis (ONJ). ONJ is an abnormality in which part of the jaw bone is no longer alive and cannot restore itself due to a lack of blood supply, especially following tooth extractions. The following case report is about an 81 year old male patient who presented with an abscess associated with tooth #3 and multiple myeloma for which he was taking the medication Aredia. Pre-treatment photograph shows tooth #3 with a temporary crown Post-treatment photograph and radiograph show a stable in place. Seen at the arrow is a fistula tract due to a fractured mesial clinical presentation. Gingival health is present, teeth 3 and 4 are root. The pre-treatment radiograph shows the bone loss associated splinted together for stability and the radiograph reveals bone fill with the mesial root. in the mesial root socket. The prognosis is much improved. SURGICAL SEQUENCE FOR FLAPLESS MESIAL BUCCAL ROOT AMPUTATION AND SOCKET PRESERVATION: 1 2 3 4 Photograph 1 shows the temporary crown removed and the periodontal probe extending down 10mm due to bone loss associated with the fractured root. Photograph 2 shows the coronal view following the root amputation. This coronal approach, without raising a buccal flap, was used to maximize vascularity to the site to minimize the risk of ONJ. Photograph 3 shows a bone graft placed into the root socket. This will maintain the clot. Photograph 4 shows the mesial root of tooth #3 that was fractured in three separate pieces. Tissue healing following the surgery was excellent with no complications. CONCLUSION: A CONSERVATIVE SURGICAL APPROACH CAN BE USED TO MINIMIZE COMPLICATIONS ASSOCIATED WITH BISPHOSPHONATES. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 58. EDUCATE YOUR DENTAL COMMUNITY ON WHY THEY SHOULD SEND THEIR PERIODONTAL & IMPLANT PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 59. NOVEMBER 2010 WHY IS RIDGE PRESERVATION BENEFICIAL FOLLOWING TOOTH EXTRACTION? A procedure that can restore and maintain the alveolar ridge following tooth extraction is ‘ridge preservation’. Loss of labial crestal bone following tooth removal remains one of dentistry’s greatest challenges. The importance of maintaining an adequate bone volume prior to implant placement cannot be overstated. Without ridge preservation, the alveolar bone will resorb from 30-60% within 6 months. At least 1mm of vertical bone height will also be lost without ridge preservation. Photograph following extraction of tooth #7. Note the Photograph 3 months following extraction and ridge preservation thinness of the buccal plate of bone and apical extent of shows impressive regeneration of the alveolar bone. The alveolar bone loss (seen at arrows). Without a ridge preservation this ridge has been restored to its original anatomy. bone would resorb leaving a large concavity in the buccal ridge. (The dark object in the back of site 7 is a retractor holding the palatal tissue back). Photograph shows soft Flap elevation shows Photograph shows Placement of a resorbable Suturing to obtain Photograph shows tissue swelling associated severe bone loss on the a bone xenograft in collagen membrane primary closure. vertical root fracture. with tooth #7. buccal of tooth #7. place. provides epithelial cell exclusion. CONCLUSION: University studies support the concept that patients should receive grafting materials at the time of tooth extraction ( Nevins, 2006 IJPDR). This is critical in preserving the natural tissue contours at the edentulous site in preparation for either a conventional or implant supported restoration. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 60. DECEMBER 2010 PERSPECTIVES IN PERIODONTICS This case report is meant to give you the perspective we have on a daily basis. As a periodontal office, we have a unique opportunity to see underneath the gingival tissues. It is both interesting and alarming to see the destructive nature of periodontal disease. Pre-treatment photograph of tooth #11 shows minimal inflammation. The amount of inflammation does not correspond to the amount of supra-gingival plaque nor the amount of sub- gingival calculus that is present. The presence of inflammation is masked by the patients smoking habit. The pre-treatment radiograph of tooth 11 shows a severe vertical bone defect along the mesial. SURGICAL SEQUENCE: Guided Tissue Regeneration with Platelet Derived Growth Factor to preserve the tooth Proper bone level Flap elevation reveals the incredible Flap reflection allows for the best A composite bone graft of Bio-Oss and ravages of periodontal disease. The access for the removal of the Demineralized Freeze Dried Bone was placed into yellow arrows point to the bone loss. calculus. Also seen is the bone loss the defect. The synthetic growth factor The black arrow points to the calculus that extended 3/4 of the way down the GEM21-S was used to enhance the regenerative that was buried sub-gingivally. The root surface. process. Following this, a resorbable barrier patient reports a history of root planning membrane was placed and the tissue sutured to that could not reach the calculus. obtain primary closure. CONCLUSION: The continued presence of calculus can lead to the loss of the teeth. Flap elevation allows access to the calculus for its removal. Guided tissue regeneration allows for replacement of the periodontal attachment structures and thereby tooth preservation. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 61. JANUARY 2011 Esthetic Crown Lengthening and Restorative Treatment A smile is an important non-verbal method of communication. A pleasing smile conveys a friendly nature and reflects happiness and confidence. A smile is an interaction between not only the teeth, but the lip framework and the gingival scaffold. Pre-treatment photographs are the smile and retracted Post-treatment photographs show the enhanced dental views of a 45 year old female. These photographs show esthetics that now allows the patient to smile more freely. the patient’s concerns that inhibit her from smiling The patient was very pleased with her new smile. fully. 1. Crown lengthening: Involves osseous re-contouring to provide 1. Short teeth which she feels gives her an aged appearance. 3mm from the crown the margins to the alveolar bone. This prevents marginal gingival inflammation. 2. Poor tooth shape makes her teeth look like ‘chicklets’. 3. Darker colored teeth makes her embarrassed to smile. 2. Improved tooth form: Crown width to height ratio of 80% leads to a more youthful tooth appearance. 4. She does not like to smile big because it exposes so much 3. Restored teeth improves the tooth shade: Provided by of her gum tissue. restorative dentist. 4. Reducing gingival display: Marginal gingiva follows upper lip. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 62. FREQUENTLY REMIND YOUR DENTAL COMMUNITY WHY THEY SHOULD SEND PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 63. FEBRUARY 2011 Preserving teeth with gingival grafting combined with a frenectomy The apical migration of the gingival margin can progress if left untreated. The success of root coverage procedures is directly related to the severity of the recession. People generally are not born with gingival recession. There is a progression from a healthy gingival attachment to slight gingival recession leading to severe deterioration over a variable time period. PRE-TREATMENT VIEWS OF TOOTH 24 demonstrate gingival POST-TREATMENT PHOTOGRAPH OF TOOTH 24: recession and a minimal band of protective keratinized attached tissue. The Gingival recession is corrected along with an increase in the second photograph shows the etiology of the periodontal defect, the high amount of attached tissue. This was accomplished with a frenum attachment. This view was obtained by pulling the lip out. With frenectomy and addition of a gingival graft. The elimination the lip pulled out, blanching of the tissue is seen. The presence of the of the frenum pull and the presence of attached tissue will frenum and lack of keratinized tissue inhibited the patient from brushing the prevent future recession from occurring and help preserve gingival margin. Plaque (at the yellow arrows) can be seen along the the tooth. The gingival margin levels have also been gingival margin on the photograph to the left. restored to an even level which improves esthetics and facilitates more effective home care. EARLY CORRECTION OF GINGIVAL DEFECTS IS THE BEST TIME FOR A SUCCESSFUL REPAIR. PROGRESSIVE DETERIORATION CAN LEAD TO TOOTH LOSS AS SEEN IN THE CASES BELOW: PATIENT #1: The photograph on the left shows the initial PATIENT #2: The photograph on the left shows the initial presentation of tooth 24. Calculus can be observed on the root condition for tooth 27 with the associated severe gingival surface along with the resulting gingival recession. The heavy recession. The loss of tissue support resulted in class III tooth frenum attachment can also be seen. Infection had spread into the mobility that made eating difficult. An extraction was performed sub-mandibular region necessitating an emergency extraction. (as can be seen) and the tooth was eventually replaced with a dental implant. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 64. BRAND YOUR PRACTICE AS THE PREMIER PERIODONTAL & DENTAL IMPLANT PRACTICE IN YOUR COMMUNITY THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS
- 65. NOVEMBER 2010 WHY IS RIDGE PRESERVATION BENEFICIAL FOLLOWING TOOTH EXTRACTION? A procedure that can restore and maintain the alveolar ridge following tooth extraction is ‘ridge preservation’. Loss of labial crestal bone following tooth removal remains one of dentistry’s greatest challenges. The importance of maintaining an adequate bone volume prior to implant placement cannot be overstated. Without ridge preservation, the alveolar bone will resorb from 30-60% within 6 months. At least 1mm of vertical bone height will also be lost without ridge preservation. Photograph following extraction of tooth #7. Note the Photograph 3 months following extraction and ridge preservation thinness of the buccal plate of bone and apical extent of shows impressive regeneration of the alveolar bone. The alveolar bone loss (seen at arrows). Without a ridge preservation this ridge has been restored to its original anatomy. bone would resorb leaving a large concavity in the buccal ridge. (The dark object in the back of site 7 is a retractor holding the palatal tissue back). Photograph shows soft Flap elevation shows Photograph shows Placement of a resorbable Suturing to obtain Photograph shows tissue swelling associated severe bone loss on the a bone xenograft in collagen membrane primary closure. vertical root fracture. with tooth #7. buccal of tooth #7. place. provides epithelial cell exclusion. CONCLUSION: University studies support the concept that patients should receive grafting materials at the time of tooth extraction ( Nevins, 2006 IJPDR). This is critical in preserving the natural tissue contours at the edentulous site in preparation for either a conventional or implant supported restoration. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 66. DECEMBER 2010 PERSPECTIVES IN PERIODONTICS This case report is meant to give you the perspective we have on a daily basis. As a periodontal office, we have a unique opportunity to see underneath the gingival tissues. It is both interesting and alarming to see the destructive nature of periodontal disease. Pre-treatment photograph of tooth #11 shows minimal inflammation. The amount of inflammation does not correspond to the amount of supra-gingival plaque nor the amount of sub- gingival calculus that is present. The presence of inflammation is masked by the patients smoking habit. The pre-treatment radiograph of tooth 11 shows a severe vertical bone defect along the mesial. SURGICAL SEQUENCE: Guided Tissue Regeneration with Platelet Derived Growth Factor to preserve the tooth Proper bone level Flap elevation reveals the incredible Flap reflection allows for the best A composite bone graft of Bio-Oss and ravages of periodontal disease. The access for the removal of the Demineralized Freeze Dried Bone was placed into yellow arrows point to the bone loss. calculus. Also seen is the bone loss the defect. The synthetic growth factor The black arrow points to the calculus that extended 3/4 of the way down the GEM21-S was used to enhance the regenerative that was buried sub-gingivally. The root surface. process. Following this, a resorbable barrier patient reports a history of root planning membrane was placed and the tissue sutured to that could not reach the calculus. obtain primary closure. CONCLUSION: The continued presence of calculus can lead to the loss of the teeth. Flap elevation allows access to the calculus for its removal. Guided tissue regeneration allows for replacement of the periodontal attachment structures and thereby tooth preservation. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 67. JANUARY 2011 Esthetic Crown Lengthening and Restorative Treatment A smile is an important non-verbal method of communication. A pleasing smile conveys a friendly nature and reflects happiness and confidence. A smile is an interaction between not only the teeth, but the lip framework and the gingival scaffold. Pre-treatment photographs are the smile and retracted Post-treatment photographs show the enhanced dental views of a 45 year old female. These photographs show esthetics that now allows the patient to smile more freely. the patient’s concerns that inhibit her from smiling The patient was very pleased with her new smile. fully. 1. Crown lengthening: Involves osseous re-contouring to provide 1. Short teeth which she feels gives her an aged appearance. 3mm from the crown the margins to the alveolar bone. This prevents marginal gingival inflammation. 2. Poor tooth shape makes her teeth look like ‘chicklets’. 3. Darker colored teeth makes her embarrassed to smile. 2. Improved tooth form: Crown width to height ratio of 80% leads to a more youthful tooth appearance. 4. She does not like to smile big because it exposes so much 3. Restored teeth improves the tooth shade: Provided by of her gum tissue. restorative dentist. 4. Reducing gingival display: Marginal gingiva follows upper lip. YOUR CONTACT INFORMATION AND LOGO RIGHT HERE
- 68. EDUCATE YOUR DENTAL COMMUNITY ON WHY THEY SHOULD SEND THEIR PERIODONTAL & IMPLANT PATIENTS TO YOUR OFFICE THROUGH WEEKLY E- MAILS AND MONTHLY MAILERS. PROVIDED BY PERIO-PROMOTIONS