Lefort 1 osteotomy
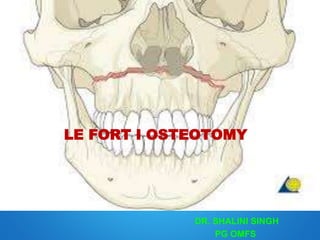
- 1. LE FORT I OSTEOTOMY DR. SHALINI SINGH PG OMFS
- 2. Contents Introduction/History Anatomical Considerations Biologic Basis For Maxillary Osteotomies Indication Outline of treatment Types Classic Lefort I osteotomy Quadrangular Lefort I osteotomy Surgically Assisted Maxillary Expansion Segmental Lefort I osteotomy Anterior maxillary osteotomy Posterior maxillary osteotomy Complications & Management References
- 3. Introduction
- 4. *“Lefort I osteotomy has become the work horse of Orthognathic surgical procedures .Its technical ease ,its broad application to resolve many functional and aesthetic problems and the dependability of its results support this evolution.” Blood supply, nasal airway problems and sinus problems*- no adverse consequences *-Bell, jos1975;33;412 * walker, turvey joms1988
- 5. Orthognathic surgery of the maxilla was first described in 1859 by von langenbeck for the removal of nasopharyngeal polyps. The first American report of a maxillary osteotomy was by David Cheever in 1867 for the treatment of complete nasal obstruction secondary to recurrent epistaxis for which a right hemi maxillary down fracture was used. Wasmund in 1927 introduced lefort I or total maxillary osteotomy technique for correction of skeletal open bite deformity. Axhausen in 1934 was the first to advance the maxilla at the Le Fort I level. Separation of the pterygomaxillary junction was advocated by Schuchardt in 1942 Moore and Ward in 1949 recommended horizontal transection of the pterygoid plates for the advancement. However, this technique was abandoned due to incidence of severe bleeding in most cases
- 6. • Hugo Obwegesser 1965 advocated complete mobilisation of maxilla so that maxilla could be repositioned without tension. • 1969-75 Bell, Lefort I downfracture & formed the BIOLOGICAL BASIS • Bennett & Wolford (1985) described cutts Parallel FH plane to prevent ramping effect. • The correct used of curved osteotome described by Turvey and Fonseca in 1980 • Precious et al described pterygomaxillary dysjunction without the use of osteotome (1991) • Use of Swan neck osteotome by cheng ( 1993) • Use of Saw by cheng (1993) • Use of Shark Fin osteotome by laster (2002) • Twist technique by fredricko (2012)
- 7. Protocol Design soft tissue to maintain adequate collateral blood supply to the ostetomised segment and to avoid injury to vital structures. Provide optimum exposure. Minimum periosteal stripping. Gentle soft tissue handling. Avoid injury to neurovascular bundle. Make osteotomy cuts under constant irrigation with normal saline. Plan interdental osteotomy cuts with out damaging periodontal status of adjoining teeth.
- 13. Biologic Basis
- 17. Studies by Bell and colleagues In the early 1970s, demonstrated that early osseous union with minimal osteonecrosis occurred following total maxillary osteotomy, indicating that the palatal soft tissue pedicle and the labial buccal gingival provide an adequate nutrient pedicle for single stage osteotomy. In 1975 provided evidence through micro angiographic studies that bilateral transection of the descending palatine vessels did not adversely affect the lefort I osteotomy procedure if basic surgical principles were followed. In 1995 continued to investigate the limits of this surgical technique by performing the lefort I osteotomy using a standard circum vestibular incision, segmentalizing the maxilla, stretching the palatal vascular pedicle and transecting the descending palatine arteries. The result was uncomplicated post operative healing, with only transient vascular ischemia.
- 18. Restoration of blood supply 1 week post operatively- Dodson -1994 JOMS 1 week –increase in periosteal-endosteal blood supply 2 weeks –vessels connecting segments 4 weeks restores blood circulation in segments Dodson in 1997 JOMS stated that no statistically significant differences in mean maxillary GBF between patients having the DPA ligated and those having the DPA preserved as measured using LDF during Le Fort I osteotomy in a study of 34 patients.
- 19. Indications of Le Fort I Osteotomy 1. Altering the vertical dimension of maxilla - Superior positioning in long face syndrome - Inferior positioning. 2. Anteroposterior movements of maxilla In cleft palate patients , congenitally deficient maxilla - Maxillary advancement - Maxillary set back in maxillary prognathism (only 3- 5mm is possible) 3. Levelling of occlusal plane. 4. Surgical expansion of maxilla 5. Narrowing of maxilla.
- 20. Outline of treatment Immediate presurgical planning • Surgical cephalometric prediction tracing. • Model surgery • Splint construction Orthognathic reconstructive surgery • Lefort I maxillary advancement or set back with expansion or superiorly or inferiorly placed. • Esthetic control of the upper lip & nose
- 23. Model surgery • Step 1. Models mounted. • Step 2. Models marked – Vertical reference – Facial midline – Horizontal reference – Palatal reference • Step 3. The following numerical measurements are made & recorded on the models: – Horizontal distance. – Distance from the max. mounting ring – Intercanine, interpremolar & molar distances.
- 26. • Step 4. The maxillary model is sectioned from its base at the level previously marked. • Step 5. Where midline split with widening is planned, the maxillary cast is separated in the midline by sawing downward . • step 6. Once maxilla is in the desired location, maxilla is secured to the base with heavy wax, the location of the maxillary incisor & 1st molar are rechecked for accuracy & skeletal movements are recoded. • Splint reconstruction
- 30. Midface Osteotomies Segmental maxillary osteotomy Single tooth Anterior segmental Posterior segmental Horseshoe Total maxillary osteotomy Lefort I SAME Classic Quadrangular Lefort II Anterior LF II Pyramidal LF II Quadrangular LF IILefort III Midface Zygomatic Malar - Maxillary
- 31. Instruments
- 32. Surgical technique 1. Positioning of the patient-10 degree head elevation 2. Hypotension GA (90mm/Hg systolic*) 3. Infiltration of the soft tissue with a vasoconstrictor 2% lidocaine (1;100000) *Anderson-delibrate hypotensive anesthesia for orthoganthic surgery.adult orthodontic orthognathic surgery 1986;1;133
- 34. V-Y closure of a lip incision. A skin hook is placed in the midline and tissue is gathered for approximately 1 cm with suture
- 35. Effect of the alar cinch technique of the width of the alar base. Note the difference after tying the suture.
- 36. Modifications
- 37. Segmentalization
- 38. Postsurgical management The surgical splint placed for 6 weeks. Elastics should be worn for at the time for 6 to 8 weeks. Non – exertional activity for 6 to 8 weeks. Nasal spray(oxymetazolin) Systemic decongestion Hierarchy of stability Maxillary advancement, posterior and superior movements are shown to be stable whereas inferior & transverse movements are unstable.
- 39. Quadrangular Le Fort I osteotomy • Hugo Obwegesser 1969 described a high Le fort I osteotomy for correction of midfacial hypoplasia in cleft lip and palate patients. This was named Quadrangular Le Fort I osteotomy by Keller & Sather 1989. Here the advancement of both the infra orbital rim and a portion of the zygomatic complex is done. Indications • This is mainly indicated in patients with maxillary-zygomatic horizontal deficiency, with class III skeletal malocclusion and normal nasal projection. This is ideal in management of midface hypoplasia with midline problems or transverse deficiency.
- 40. Procedure • The osteotomy cuts are placed on the lateral wall of maxilla from the pyriform aperture at the level of the infra orbital nerve. • The osteotomy is extended laterally below the level of the infra orbital nerve to the tuberosity and pterygoid plate region. • The maxilla is down fractured after detaching the nasal septum, pterygomaxillary disjunction and ostectomising the lateral nasal wall. • Bone grafts are used in the infra orbital region and also in the pterygomaxillary junction.
- 42. Surgical Assisted Maxillary Expansion (SAME) Brown first described SAME in 1938 - midpalatal split A LeFort I type of osteotomy with a segmental split of the maxilla and the placement of a triangular unicortical iliac graft for correction of maxillary constriction was presented by Steinhauser in 1972. Indications: Skeletal maxillomandibular transverse discrepancy greater than 5mm Significant TMD associated with a narrow maxilla and wide mandible Failed orthodontic expansion Necessity for a large amount more than 7mm of expansion Extremely thin and delicate gingival tissues with buccal gingival recession Significant nasal stenosis Widening of the arch following collapse associated with the cleft palate deformity
- 43. Technique
- 44. Anterior Segmental Osteotomy Cohn-Stock (1921) Wassmund (1935) Wunderer (1963) Cupar (1955) Epker and wolford (1980)
- 45. 1921 – Cohn Stock. Transverse palatal incision Wedge shaped osteotomy green stick fracture retracted the anterior segment Relapsed within 4 weeks Various incision designs for desired osseous movements . *Bell- overall procedure is predictable from standpoint of dental stability and soft tissue changes. * Stability and soft tissue changes in anterior part of jaw surgery A J ORDNTCS;1973
- 46. Indications : Correction of bimaxillary protrusion. Marked protrusion of the maxillary teeth (normal incisor axial inclination to alveolar bone) Anterior open bite To retract the anterior teeth when that cannot be accomplished by conventional orthodontic treatment.(pt non-complience) When orthodontic tooth movement is inadvisable.(ankylosis, root resorption) Improvement in appearance.
- 47. *Radioactive microsphere techq used assess the blood flow in AMO in macaque monkeys. Variation in flap design didn’t affect the postop blood supply to ant maxillary segment. This study gives scientific credence to different incisions for AMO Blood supply can be maintained by- labial-buccal & palatal tissues , labial –buccal tissues alone palatal tissues alone *Nelson –quantation of blood flow after AMO in three teq- JOS, 1978;36:108-112
- 48. • Preserves both buccal & palatal soft tissues. • Incision : vertical incision – planned extraction or interdental osteotomy. Anterior nasal spine incision. • Osteotomy : buccal horizontal osteotomy transpalatal osteotomy repositioning of entire segment. Wassmund technique : 1935
- 49. Wunderer technique : 1963 Similar to wassmund, except the palate is exposed by a transverse palatal incision with the margins away from the osteotomy site.
- 52. Downfracture Technique Technique : A buccal vestibular incision is created, allowing direct access to the anterior lateral maxillary walls, piriform aperture, nasal floor and septum. Most commonly used for AMO* Advantages : Direct access to the nasal structures Unhampered access – bone grafting Ability to remove bone under direct visualization Preservation of blood supply Ease of placement of rigid internal fixation.
- 54. Posterior Segmental Osteotomy Schuchardt (1959) Kufner (1971) - described a single buccal incision approach. Indications 1. Post maxillary alveolar hyperplasia 2. Total maxillary hyperplasia (when combined with AMO) 3. Distal repositioning of the post maxillary alveolar fragment to provide space for proper eruption of an impacted canine or bicuspid tooth 4. Spacing in the dentition that can be closed by ant repositioning of the posterior segment 5. Transverse excess or deficiency 6. Posterior open bite 7. Posterior cross bite
- 56. Combination Anterior & Posterior Maxillary Osteotomy Also called Horseshoe osteotomy A combined form of anterior and posterior subapical osteotomies "total subapical maxillary osteotomy" were reported by Paul 1969 for midface hypoplasia.. This technique was further described by West & Epker 1972, Hall & Roddy 1975, Wolford & Epker 1975. Indication Maxillary alveolar hyperplasia with or without an anterior open bite deformity Transverse hypolplasia without a vertical component This procedure creates a three piece maxilla, with the central nasal portion left undisturbed, through the use of palatal parasagittal osteotomies
- 57. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;97:683-92
- 58. Complications Intraoperative Postoperative Intraoperative 1. Incision design & closure 2. Unfavourable osteotomy - # at the junction of the horizontal process of the palatine bone with the palatal process of the maxilla - horizontal # of the pterygoid plates
- 59. 3. Bleeding PSA Artery Greater palatine artery Maxillary artery Pterygoid venous plexus ( Panula K, JOMS2001) Management Localized pressure packing directed at the bleeding point Cauterization with either chemical or with diathermy Ligation of the ECA Transantral ligation of maxillary artery Angiographic emoblization (IJOMS, 2005)
- 60. 4. Improper maxilary repositioning - failure to seat one or both of the mandibular condyles during maxillary repositioning will cause improper maxillary positioning & a malocclusion cause - insufficient bone removal
- 61. • 20 yrs period – 1000 Le Fort I osteotomies • Anatomical complication – 26 pt. – 16- deviation of nasal septum – 10 non union of osteotomy gap • Extensive bleeding – Require transfusion- 11 – Ligation of ECA – 1 • Significant infection – abscess & sinusitis-11 • Ischemic complication -10 • Aseptic necrosis – 2 • Insufficient fixation - 5
- 62. Postoperative Infections Sinusitis Occlusal derrangement Unaesthetic apperence Vascular compromise Haemotoma Devitalization of teeth Periodontal problems Oroantral communication Eur Rev Med Pharmacol Sci. 2013 Feb;17(3):379-84.
- 63. Infection • Behrman (1972) reported only 3 cases of infection out of 600 maxillary osteotomies. A double blind study of Eschelman 1986 showed a significant reduction of infection with antibiotic prophylaxis . They listed some of the indications for prophylactic antibiotics in orthognathic surgery. • - An intraoral surgical approach • - Previous irradiation of operative site • - Use of bone grafts • - Use of alloplastic implants • - Poor oral hygiene • - Patient prone to infection.
- 64. Aseptic necrosis • These complications are related to the degree of vascular compromise and occur in fewer than 1% of cases. Rupture of the descending palatine artery (DPA) during surgery, postoperative vascular thrombosis, perforation of palatal mucosa when splitting the maxilla into segments, or partial stripping of palatal soft tissues to increase maxillary expansion may impair blood supply to the maxillary segments. Sequellae of compromised vasculature include loss of tooth vitality, development of periodontal defects, tooth loss, or loss of major segments of alveolar bone or the entire maxilla. (Felipe Ladeira Pereira JOMS 2010) • The treatment of avascular necrosis of the maxilla is not easily attained. Although no treatment protocol has been established, aseptic necrosis of the maxilla should be treated by maintenance of optimal hygiene, antibiotic therapy to prevent secondary infection, heparinization, and hyperbaric oxygenation. A recent report described treatment of avascular necrosis of the maxilla related to a previously performed orthognathic surgery by hyperbaric oxygenation, bone grafting, and oral rehabilitation by an implant-supported fixed prostheses, with a successful outcome.( Singh J, BJOMS 2008)
- 65. Relapse • Maxillary advancement : 5-9% , mean 11%(FU- 15mons) • Maxillary superior repositioning – most stable – Anterior – 0-18% mean – 11% – Posterior – 7-24% mean – 3% • Maxillary inferior repositioning – Anterior – 9-54% mean -28% – Posterior – 21-167% mean – 70% • Maxillary expansion : 8-14% mean-11% (FU- 28mons)
- 66. Nerve injury • The incidence of infraorbital nerve neurosensory deficits at 12 months has been reported to be as high as 6% when tested objectively. • During Le Fort osteotomy it is recognized that the nasopalatine and posterior, middle, and anterior superior alveolar nerves are completely severed as an intrinsic part of the surgical procedure. Management of the descending palatine neurovascular bundle is controversial . • Despite ligation and division of the neurovascular bundle, sensory recovery does occur and is most likely to represent collateral axonal sprouting from adjacent nerves. (Gary F. Bouloux, Oral Maxillofacial Surg Clin N Am 2003)
- 67. References • Epker Stella Fish – Dentofacial Deformities (volume 2). • Fonseca othognathic surgey – (volume 2) • The quadrangular osteotomy revisited. Paul J W Stoleinga & John J A Brouns. Journal of Cranio Maxillofacial surgery. 2000 : 28 : 79 2013; 84. • Maxillary osteotomies. R. Gunaseelan. Indian journal of Oral & Maxillofacial surgery. 1998 : VIII : 9 -14. • Johan P. Reyneke, Oral Maxillofacial Surg Clin N Am 19 (2007) 321–338 • Brian A. Vandersea, Oral Maxillofacial Surg Clin N Am 19 (2007) 351–368
- 68. Thank U