Echocardiography in TAVI patients 2014
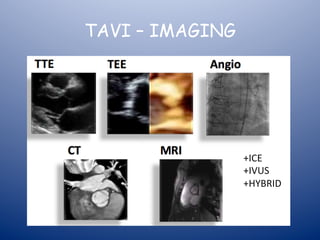
- 1. TAVI – IMAGING +ICE +IVUS +HYBRID
- 2. Use of Imaging for TAVI § Assessment pre TAVI § TTE, MSCT, 3DE, coronary angiography § Assessment during TAVI § TOE/TTE, Fluroscopy § Assessment post TAVI § TTE, MSCT
- 3. Assessment pre TAVI • TTE – Diagnosis: severe AS, morphology – Aortic regurgitation – LVOT/subaortic stenosis – Mitral & tricuspid valves – LV & RV function – Pericardial effusion – LV hypertrophy – LV/LA thrombus • MSCT/3DE – Annulus size – Prosthesis type and size – Coronary height – Sinus of valsalva diameter – Femoral access • Coronary angiography – Proximal CAD – PCI • CMR – LGE – interstitial fibrosis • Dobutamine stress ECHO SCREENING
- 5. Is it severe AS? • “Flow dependent” parameters • Post-VPC accentuation of gradient • Atrial fibrillation • Aortic regurgitation • “Classical” LG LF severe AS reduced LVEF (DSE) • “Paradoxical” LG LF severe AS normal LVEF • NF, LG, N LVEF severe AS
- 7. (SV = TVI LVOT x CSA LVOT) or SVI
- 9. Dobutamine stress ECHO in paFent with LGSAS Baseline CW tracing: Peak velocity 3.2 m/s Mean grad 25 mmHg AVA 0.45 cm2 CW 10ug/kg/min dobutamine Peak velocity 4.1 m/s Mean grad 39 mmHg AVA 0.5 cm2
- 10. DSE in a patient with Pseudo-severe AS Baseline 5 ug/kg/min Peak velocity stable, AVA increased, contracFle reserve +, absence of severe AS 10 ug/kg/min 20 ug/kg/miin
- 11. NFHG N EF LFLG N EF NFLG N EF LFLG Low EF Algorithm for classificaFon of paFents with LGSAS MSCT – extent of AV calcium
- 12. Imaging for aortic annulus sizing prosthesis type/sizing TTE/TOE MSCT 3D-‐ECHO
- 13. Circ Cardiovasc Interv: 2008 Piazza et al
- 14. Understanding Annulus Anatomy VIRTUAL ANNULUS Most basal point of aortic leaflet attachment Measured during systole, ensure alignment, Circ Cardiovasc Interv: 2008 Piazza et al trailing edge to leading edge – PLAX TTE/TOE
- 15. MSCT ECHO 3D 2D AorFc annulus is oval In shape in majority of PaFents RaFo of longD/shortD 1.28
- 17. Basal SAX view of Aortic Valve RC LC NC Circ Cardiovasc Interv: 2008 Piazza et al
- 18. AORTIC ANNULUS SIZING -‐ 2D vs 3D
- 19. Histology of Aortic Valvar Complex Circ Cardiovasc Interv: 2008 Piazza et al
- 21. ECHO vs Surgical Assessment Annulus Diameter
- 22. 2-D TOE Underestimate 35% Correct 55% Overestimate 10% 3-D TOE Mylofe et al, JACC CV Intervent 2014
- 23. INCORRECT SIZING • WRONG VALVE USED IN 50 % OR CASES
- 24. Aortic annulus – diameter variation during cardiac cycle Aortic annulus: 4-5% larger in systole vs diastole
- 25. Which MSCT Measurement to use…… • Short diameter • Long diameter • Mean diameter: SAPIEN • Area-‐derived diameter • Perimeter-‐derived diameter • Area: SAPIEN • Perimeter: CoreValve
- 26. Oversizing – does it mafer? • 10-‐20% oversizing recommended • Area/perimeter/mean diameter • TransiFon zone – Annulus falls between two valve sizes • Presences of LVOT calcium – Important: • balloon-‐expandable valves: root rupture • Self-‐expanding valves: para-‐valvular leak • Any post-‐TAVI BAV: root rupture/valvular AR
- 28. CONSEQUENCES OF INACCURATE AORTIC ANNULUS SIZING • ANNULUS RUPTURE – BALLOON EXPANDABLE – SELF-‐EXPANDING • PARAVALVULAR AORTIC REGURGITATION – LINKED TO PROGNOSIS • VALVULAR AORTIC REGURGITATION • PROSTHESIS EMBOLISATION • PPM REQUIREMENT POST TAVI • POST-‐TAVI BAV – ASSOCIATED WITH INCREASED RISK OF CVA
- 31. 3D ANALYSIS OF 3-‐DIMENSIONAL STRUCTURE
- 34. AORTIC ANNULUS – INACCURATE SIZING
- 35. Imaging for aortic annulus sizing prosthesis type/sizing TTE/TOE MSCT 3D-‐ECHO
- 41. GA required for 3D TOE
- 44. When should 3DE be a surrogate, alternative or preferred for TAVI sizing • When MSCT cannot be obtained but 3D available – No local expertise with MSCT • When MSCT is contraindicated/risky – Severe renal impairment • When there is doubt regarding the quality of the MSCT – Motion artifact/difficult to repeat
- 45. MSCT for assessment of peripheral access
- 46. 3-‐MENSIO VALVES (MSCT BASED FEM ART ACCESS ANALYSIS)
- 47. MSCT GOLD STANDARD FOR AORTIC ANNULUS SIZING 2D TEE AND TTE UNDERESTIMATES AORTIC ANNULUS DIMENSIONS AORTIC ANNULUS DIMENSIONS IMPORTANT FOR ACCURATE PROSTHESIS SIZING
- 48. OR SLIDE FROM JAMES’ TAVI Talk on peripheral access
- 49. Assessment during TAVI PROCEDURE
- 50. TAVI -‐ PROCEDURAL STEPS • Baseline ECHO • Peripheral access • Identify ideal projection • Cross valve • BAV • TAVI valve positioning • TAVI valve deployment • Post deployment final assessment – Haemodynamic – Aortography – TOE/TTE • Real-time monitoring for complications during procedure
- 51. Baseline TOE/TTE at start of procedure • Confirm gradients • Baseline aortic regurgitation • Baseline mitral valve assessment • LVOT • Baseline LV/RV wall motion • Baseline pericardial effusion • Online monitoring of valve procedure/complications • Repeat all at end of procedure + check for complications
- 53. M85, CKD, COPD, PAF, T2D Class IV NYHA, no significant CAD
- 61. SUPPORTIVE HYBRID REAL-‐TIME GUIDANCE Overlay of 3D MSCT images from pre-‐procedure Screening on top of live X-‐Ray fluoroscopy
- 64. PSAX TTE Day 1 Post TAVI CDF
- 67. Procedural Findings Assessment of Post-‐Procedural AR: Requires agreement of three assessment tools Echocardiography Hemodynamics Aortography PVAR vs VAR Severity ComplicaFons AR Valve posiFon Gradient/AVI Coronary perfusion TCT 2013 Procedural Outcomes Extreme Risk Study | Iliofemoral Pivotal 67
- 68. Cath Lab Assessment Immediate Post Deployment • Haemodynamic – AV index: Ao diastolic pressure-‐LVEDP (<25 = significant AR) – Peak to Peak gradient + mean gradient (PT Ao-‐LVPT) • Aortography – PVAR/VAR – use enough contrast/RAO projecFon – Coronary artery perfusion – Competence of aorFc root • ECHO: TOE/TTE – AorFc paravalvular and valvular leak – Systolic valve funcFon: PG, MG, AVA – LV/RV systolic funcFon – Pericardial effusion – compare with baseline – Mitral valve funcFon – mitral regurgitaFon, AML hinge point – Tricuspid valve/pulmonary pressure
- 69. ComplicaFons & Management AorFc RegurgitaFon • Typically paravalvular mild or mild-moderate severity • Most of AR disappears or reduces at 1 yr follow-up [13% absent, 80% mild AR] Cardiol Clin 29 (2011) 211–222 J. Am. Coll. Cardiol. 2012;59;1200-‐1254
- 72. Annular and leaflet calcification may limit prosthesis expansion – cause of PVAR
- 73. Paravalvular/valvular aorFc regurgitaFon post TAVI • AeFology (paravalvular) – MalposiFon • Supra-‐annular • Infra-‐annular – Underexpansion • Focal/widspread calcificaFon – Prosthesis mismatch • Undersizing – Horizontal aorta: • AeFology (valvular) significant VAR uncommon – Incorrect prosthesis size • Oversizing – Valve damage during procedure – Underexpanded valve – calcium – Overexpansion of valve – post TAVI BAV
- 78. Assessment of para-‐valvular aorFc regurgitaFon post TAVI ** Not well-‐validated and may overesFmate the severity compared with the quanFtaFve doppler PVAR assessment cont’d…….. TOE: Deep transgastric permits best axial alignment for the quanFtaFve doppler measurement of regurgitant pressure half-‐Ame. PLAX and PSAX ME: indenFficaFon of site, number and extent of PVAR jets. Vena contracta diameter and area can be assessed using 2D and 3D colour doppler but may not be a reliable measure of PVAR post TAVI (mulFple, small, irregular shape, eccentric jets)
- 79. Para-‐valvular AR post TAVI ME PSAX ME PLAX
- 82. Native aortic valve regurgitation post balloon aortic valvuloplasty
- 83. Deep Transgastric view – PHT
- 84. US Pivotal Extreme Risk Study Surgical AVR paravalvular leak: 2-‐4%
- 85. US Pivotal Extreme Risk Study
- 86. Malposition – infra-annular SAPIEN Balloon-‐expandable
- 87. Malposition – infra-annular Different Mechanism: CoreValve self-expanding
- 90. Annular Rupture, Aortic Dissection…
- 91. TAVI IMAGING at follow-up • Imaging modalities – TTE –valve function – MSCT – valve deformity – CMR – LV/RV assessment FOLLOW-‐UP
- 92. Suggested time for routine ECHO follow up post TAVI § 24-48 hrs, pre-discharge § 30 days § 6 month § 12 months § Then yearly thereafter
- 93. Routine ECHO assessment of TAVI valve • Valve position • Valve morphology • Valve function – Systolic – Diastolic • LV size and systolic function +RV • Mitral + tricuspid • Pulmonary pressure • Pericardial effusion
- 94. How is TAVI different from SAVR • TAVI (vs SAVR) – No sewing ring – Much longer prosthesis (up to 55 mm) • Flow acceleration • LVOT diameter • Valve type • PVAR – Native valve in situ • Calcium, leaflets, prosthesis type, size, expansion – LBBB more common
- 95. Definition of new valve dysfunction at follow-up • Suspected structural TAVI failure: compare to patient’s baseline ECHO eg TTE post-procedure (Day 1) • Significant changes: – An increase in the mean gradient >10 mmHg – A decrease in the AVA >0.3-0.4 cm2 – A reduction in the DVI >0.10-0.13 • Exclude measurement error – – Baseline (Day 1) LVOT diameter – Depends on valve depth in LVOT and valve type – LVOT diameter and LVOT velocity for AVA should be measured in same location outside the stent frame – LVOT non-circular – Flow acceleration inside stent frame prox to valve cusps with elevated velocity • Note changes in LV function and allow for effect on gradient
- 96. Definition of new valve dysfunction at follow-up • Suspected structural TAVI failure: compare to patient’s baseline ECHO eg TTE post-procedure (Day 1) • Significant changes: – An increase in the mean gradient >10 mmHg – A decrease in the AVA >0.3-0.4 cm2 – A reduction in the DVI >0.10-0.13
- 98. Post-implantation follow up of TAVI patients • Similar to follow up of surgically implanted prostheses but two important differences – Calculation of EOA as an index of valve opening: • Founded in ratio of post- to pre-valvular velocities • Flow acceleration within transcatheter valve proximal to the valve cusps • Pre-valvular velocity should be recorded proximal to the stent (PW doppler with sample situated where LVOT diameter measured) and the post-valvular velocity recorded with CW doppler reflects that distal to the stented valve • If the LVOT velocity used in the calculations is erroneously recorded inside the stent but proximal to the cusps the result will be an increased velocity with an overestimation of the valve area and DVI
- 99. Prosthetic Aortic Stenosis • Limitation of flow independent parameters – The absolute EOA does not account for the cardiac output requirements in relation to the patients body size – The indexed EOA may overestimate the haemodynamic burden in obesity; hence lower criteria may be more appropriate in patients with a BMI>30kg/m2 – DVI severity criteria are dependent on LVOT size ie a lower threshold may be more appropriate if LVOT>25mm – The LVOT should be measured just beneath the ventricular margin of the valve stent/skirt – Unlike the surgically implanted valve, the transcatheter prosthetic valve EOA is defined not only by the size of the valve but also by the patient’s aortic valve/annular anatomy and procedural variables. Thus, well-established normal trans- catheter valve gradients and EOAs based on preimplant aortic annular dimensions do not currently exist.
- 101. • In condiFons of normal or near normal SV
- 102. DSE
- 105. Assessment of para-‐valvular and valvular prostheFc AR post TAVI ** Not well-validated, assumes continuity of flow and may overestimate the severity compared with the quantitative doppler PLAX and PSAX TTE: Number/distribution and extent of PVAR jets. A3C and A5C for further assessment of jets: PHT.
- 106. MSCT post TAVI Coronal Oblique View 3D volume rendered view Medtronic CoreValve 2 weeks post TAVI -‐Adequate deployment -‐No instent restenosis -‐Patent coronary art -‐Good valve posiFon -‐Integrity of stent struts -‐thrombus/vegetaFon visible on leaflets -‐Assymmetric expansion
- 108. Edwards Sapien XT/3
- 109. TTE PRE TAVI PLAX: CDF VAR/MR & A5C: CDF VAR
- 111. PORTICO TAVI post-‐implantaFon: LVOT measurement
- 112. A5C TTE Day 1 Post TAVI VTI LVOT
- 113. A5C TTE Day 1 Post TAVI CW AorFc Valve
- 114. PORTICO TAVI D1 LVOT measurement
- 115. A5C TTE Day 2 Post TAVI PW LVOT outside valve and inside valve
- 116. A5C TTE Day 2 Post TAVI CW AorFc Valve
- 117. SECOND GENERATION TAVI DEVICES
- 118. PORTICO Day 1 – Post TAVI Baseline TTE Day 1 post TAVI
- 119. TTE PRE TAVI PLAX: CDF VAR/MR & A5C: CDF VAR
- 120. PORTICO Day 1 – Post TAVI Baseline TTE Day 1 post TAVI
- 121. A4C TTE Day 2 Post TAVI Simpsons Biplane for LVEF
- 122. PLAX TTE Day 1 Post TAVI
- 123. PSAX TTE Day 1 Post TAVI CDF
- 124. PSAX 2D TTE Day 1 Post TAVI
- 125. A5C TTE Day 1 Post TAVI
- 126. A5C TTE Day 1 Post TAVI PVAR PHT
- 127. PSAX TTE Day 1 Post TAVI Mitral Valve CDF
- 128. PSAX TTE Day 1 Post TAVI CDF RVOT/PV/TV/AV
- 129. Pre TAVI
- 132. A5C TTE Day 2 Post TAVI CDF PVAR and PHT PVAR
- 151. The color Doppler jet of a paravalvular leak is ouen best appreciated from the deep transgastric TEE view (Figure 19). This view usually permits the best axial alignment for the quanFtaFve Doppler measure of regurgitant pressure half-‐Fme. The midesophageal views provide the cross-‐ secFonal and long-‐ axis views to facilitate idenFficaFon of the site and extent of paravalvular leak. The vena contracta diameter and area can be assessed using 2D and 3D color Doppler applicaFon, respecFvely (Figure 20).
- 152. Valve funcFon • Valve Academic Research ConsorFum-‐2 maintains the original recommendaFons to use echocardiography as the primary imaging modality for the assessment of prostheFc valve funcFon.39 This should include the valve posiFon, morphology, funcFon, and evaluaFon of the leu ventricle (LV) and right ventricle (RV) size and funcFon. The sug-‐ gested Fme points for rouFne follow-‐up transthoracic echo-‐ cardiography (TTE) following valve implantaFon are:immediately (before discharge) following the implantaFon for transarterial approaches or within 30 days for transapi-‐ cal or transaorFc approaches, 6 months following implantaFon, 1 year following implantaFon, and yearly thereauer. At these endpoints, prostheFc aorFc valve steno-‐ sis and regurgitaFon should be reported.
- 153. Diagnosis of aorFc stenosis • Establishing diagnosis of severe AS – AVA <0.8-‐1.0 or AVAI <0.6cm/m2 – MG >40 mmHg – Peak velocity >4.0 m/s • Pixalls in ECHO diagnosis – Gradient post-‐ectopic – Hyperdynamic states eg anaemia – AorFc regurgitaFon – Doppler beam not parallel to valve being assessed – Low LVEF “classical” LF LG severe AS (DSE of use): severe vs pseudosevere AS and contracFle reserve – Normal LVEF “paradoxical” LF LG severe AS: hypertrophied low volume LV, low SV
- 154. • TTE (pre-‐TAVI planning) – Annular dimension for accurate valve sizing • LimitaFons of TTE and TOE • TAVI CT method of choice • Undersizing may cause PVL, valve migraFon • Oversizing may cause root rupture and incomplete expansion of valve leaflets with valvular AR, reducFon in valve durability • Annular diameter measure in systole (annulus is bigger in systole), in PSLAX, at point of inserFon of aorFc cusps (virtual annulus), from Fssue blood interface to Fssue blood interface: trailing edge to leading edge • TTE underesFmates the annulus in most cases (not measuring true diameter, annulus no circular but oval in most cases) • TOE 2D sFll underesFmates annulus in 30% of cases, but overesFmates annulus in 10-‐20% of cases making valve sizing difficult • TOE 3D is more accurate and correlates well with TAVI CT measurements but resoluFon much lower and equipment and experience required to be useful
- 155. • TTE (pre-‐TAVI planning) – Bicuspid vs tricuspid valve – LV and RV dimensions and funcFon – AorFc regurgitaFon – Structure and funcFon of other valves – LVOT obstrucFon – Basal septal hypertrophy – LV thrombus – Pre-‐exisFng echolucent pericardial space eg fluid or fat and calcificaFon (trans-‐apical)
- 156. • TOE (pre-‐TAVI planning) – Not rouFnely done pre-‐procedure since rouFne TAVI CT performed – used in our insFtuFon intra-‐procedurally (annulus measurements confirmed) – If doubt re: aorFc root, annular size, bicuspid vs tricuspid, LVOT calc – TOE assumes annular circularity – almost never the case – Annulus to RCA osFum can be measured but not the annulus to LCA osFum (requires 3D-‐TOE or MSCT) – AorFc arch atheroma – important to know but MSCT also good and devices smaller more stearable with less risk of embolisaFon
- 157. • Role of 2D-‐ECHO limited during TAVI – Immediate detecFon of complicaFons at any stage – Eg causes for hypotension: • Tamponade, severe PVL, root rupture, new LV dysfuncFon (coronary obstrucFon) – Assessment of valve funcFon auer deployment • Mechanism of AR • PVL • Valvular regurgitaFon • Systolic valve funcFon: eg remaining gradient/area, need for further postdilataFon – Deep TG view: CW, PW, CF • Prosthesis impingement of the AML if prosthesis extends past the AML hinge point • Complemented by haemodynamic assessment and aortography
- 158. • Role of 3D-‐TEE during TAVI – Annulus dimension confirmaFon if doubt – important for accurate prosthesis sizing – Assessment of severity of PVL post TAVI deployment • Planimetry of regurgitant orifice (eg DTG, Mid-‐oesophageal) • Planimetry of vena contracta – Other imaging modaliFes: • Intracardiac ECHO (ICE) • Trans-‐nasal TOE
- 160. Follow up assessment • The follow-‐up assessment should also begin with valve imaging and documentaFon of changes in morphology. When determining whether a paFent has developed haemodynamically significant structural valve failure, the paFent’s own baseline echocardiographic parameters should be used as a reference. • An increase in the mean gradient >10 mm Hg, a decrease in the EOA>0.3-‐0.4 cm2, or a reducFon in the DVI>0.1-‐0.13 probably indicates a change in valve funcFon and should trigger a comprehensive haemody-‐ namic evaluaFon • Whenever valve dysfuncFon is suspected, the careful evaluaFon of valve morphology should confirm a structurally abnormal valve. In addiFon, measurement error must be excluded; the use of a consistent LVOT diameter for more accurate follow-‐up study comparisons is recommended. • Finally, changes in ventricular morphology would be expected in the se}ng of long-‐standing significant valvular dysfuncFon and this parameter may support the clinical assessment of severity.
- 162. TAVI -‐ PROCEDURAL GUIDANCE
- 164. TAVI – IMAGING MODALITIES • ECHO • MSCT • FLUORO • CMR • HYBRID – MSCT+FLUORO • OTHERS – IVUS, ICE
- 165. ICE for TAVI
- 166. IVUS FOR TAVI VOLCANO CorporaFon -‐ 9F -‐ 60 mm field of depth IVUS MSCT
- 167. 3MENSIO
- 168. PHILIPS – MSCT (NAVIGATOR)
- 169. TAVI
- 173. Key TAVI Exclusion Criteria by ECHO • Bicuspid or unicuspid valve • Severe valvular regurgitation (any) • Pre-existing prosthetic heart valve • Moderate/severe MS • Hypertrophic obstructive cardiomyopathy • Severe basal septal hypertrophy with LVOT gradient • Aortic annulus<20 or >29 mm • Asc aorta diameter >43 mm (>40 for small annulus)
- 178. PLAX of typical severe AS with gradients and AVA on side
- 179. PLAX Mr Neville Pseudosevere AS or Mr Ferris (gradient and AVA)
- 180. DSE Features to look for to disFnguish between true severe and pseudo severe AS
- 181. Paradoxical LF LG N LVEF
- 183. Circ Cardiovasc Interv: 2008 Piazza et al
- 185. • The immediate post-‐TAVI evaluaFon documents iniFal valve appearance (posiFon and circularity of the stent, and leaflet morphology and moFon) and a comprehensive haemodynamic evaluaFon. Valve Academic Research ConsorFum-‐2 advocates using the integraFve approach • Using 1 flow dependent (eg, mean gradient) and 1 flow independent criterion (eg, EOA) for the iniFal haemodynamic evaluaFon • If there is discordance between these measurements, then the DVI should be calculated. An abnormal DVI indicates possible prostheFc valve dysfuncFon • A normal DVI indicates intrinsically normal prostheFc valve funcFon, and the indexed EOA can then be used to determine the reason for the iniFal measurement discordance. When the indexed EOA is low in the se}ng of a normal DVI, the paFent probably has a prosthesis–paFent mismatch (PPM), an indicator of the intrinsic relaFonship of the implanted valve to the cardiac output requirements of the paFent • Prosthesis–paFent mismatch occurs in the se}ng of a morphologically normal valve and is considered to be haemodynamically insignificant if the indexed EOA is >0.85 cm2/m2, moderate if between • 0.65 and 0.85 cm2/m2, and severe if<0.65 cm2/m2. However, for obese paFents (body mass index >30 kg/ m2) lower criteria may be more appropriate
- 186. • There is growing evidence suggesFng a significant associaFon of post-‐ procedural paravalvular aorFc regurgitaFon (AR) with short-‐ and long-‐ term mortality. • As the number of implanted transcatheter heart valves increases, valve durability and dysfuncFon become more crucial issues. • EvaluaFng the presence and severity of regurgitaFon should include an assessment of both central and para-‐valvular components, with a combined measurement of ‘‘total’’ aorFc regurgitaFon (AR) reflecFng the total volume load imposed on the LV • The quanFtaFve and semi-‐quanFtaFve haemodynamic assessment of AR severity should be performed with Doppler echocardiography according to the guidelines • Color Doppler evaluaFon should be performed just below the valve stent for para-‐valvular jets, and at the co-‐aptaFon point of the leaflets for central regurgitaFon
- 187. • Although all imaging windows should be used, the parasternal short-‐axis view is criFcal in assessing the number and severity of paravalvular jets • Whenever possible, the quanFficaFon of the prostheFc regurgitant volume, effecFve regurgitant orifice area, and regurgitant fracFon (Table 10) should be performed • The regurgitant volume may be calculated as the difference between the stroke volume across any non-‐regurgitant orifice (RVOT or mitral valve) and the stroke volume across the LVOT • It is important to realize that at this Fme the body of evidence supporFng the numerical criteria used in Table 10 as well as Figure 4 may be limited. These criteria should be used as guidelines for clinical decision-‐making and require further validaFon as our experience conFnues to expand
- 188. – Accurate quanFficaFon of AR post TAVI • May consist of valvular and para-‐valvular AR (usually just PVR) • Valvular AR: CF doppler, – length of jet unreliable indicator of severity, – proximal jet width or cross-‐secFonal area preferred, – following criteria: <25% mild, 26-‐64% moderate, >65% severe, limited to valvular AR as PVR ouen mulFple jets, irregular shaped jets and eccentric jets • Valvular AR: Vena Contracta – VC esFmate of EROA – AcousFc shadowing from stent/sewing ring may interfere with measurements – VC measured at the level of the cusps of the bioprostheFc valve • QuanFtaFve measurements – Total SV-‐non-‐regurgitant valve SV=RV – EROA: SV/VTI – Based on several measurements with potenFal for errors significant
- 189. • Para-‐valvular AR: • ASE/EAE guidelines • Vena Contracta – Measured at the prox end of the stent skirt – No validaFon for adding the vena contracta of mulFple jets • ProporFon of the circumference of the sewing ring/proximal stent skirt occupied by the jet gives a semi-‐quanFtaFve guide to severity: – <10% mild – 10-‐20% moderate – >20% severe – Assumes conFnuity of the jet which may not be the case for transcatheter valves and thus may overesFmate the severity of PVAR in the se}ng of mulFple small jets – This approach does not consider the that the radial extent of PV jets may vary (eg surgical PVL) and in the case of transcatheter valves may be very small ie not a big problem – AfempFng to add the degrees of involvement when the jets are small is challenging • QuanFtaFve methods for assessment of severity of PVAR post TAVI – RV: – comparison of SV across AV (forward+regurg vol) LVOT and a non-‐regurgitant valve eg mitral or tricuspid (RV ouxlow), can be used for prostheFc valves and for TAVI – Total stroke volume also measured by: subtracFng LVESV (forward) from LVEDV(forward+regurgitant), not accurate with 2D, 3D may be the method of choice, growing evidence for 3D evaluaFon of RV by this method for naFve AR – EROA: – Shore pressure half Fme of CW doppler signal of AR: problem: mulFple jets, eccentric, irregular shape, – Density of spectral display: best if one single jet – Diastolic flow reversal in the desc aorta: PW doppler from the suprasternal notch/abdominal aorta from subcostal view • CombinaFon of above, iniFal haemodynamic assessment and aortography is ouen required as well as clinical parameters during follow up • CMR auer 7 weeks in experienced centres with the right magnet is the most accurate and limited evidence suggests that the echo assessment underesFmates the degree of severity of PVR post TAVI
