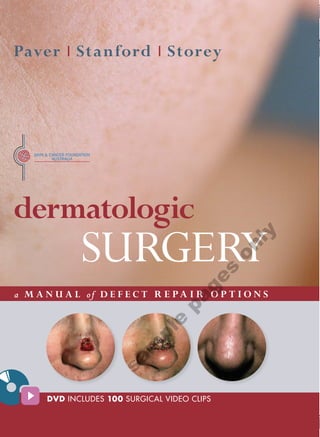
New Book: Dermatologic Surgery, Robert Paver, Duncan Stanford & Leslie Storey
- 1. 18mm 286mm Paver I Stanford I Storey dermatologic SURGERY ly on s ge a M A N U A L of D E F E C T R E PA I R O P T I O N S pa e pl m sa DVD INCLUDES 100 SURGICAL VIDEO CLIPS 18mm
- 2. dermatologic SURGERY ly on a M A N U A L of D E F E C T R E PA I R O P T I O N S s ge pa e pl m sa
- 3. Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The editors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the editors, nor the publisher, nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete. Readers are encouraged to confirm the information contained herein with other sources. For example, and in particular, readers are advised to check the product information sheet included in the package of each drug they plan to administer to be certain that the information contained in this book is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. First published 2011 Copyright © 2011 McGraw-Hill Australia Pty Limited Additional owners of copyright are acknowledged in on-page credits. Every effort has been made to trace and acknowledge copyrighted material. The authors and publishers tender their apologies should any infringement have occurred. Reproduction and communication for educational purposes The Australian Copyright Act 1968 (the Act) allows a maximum of one chapter or 10% of the pages of this work, whichever is the greater, to be reproduced and/or communicated by any educational institution for its educational purposes provided that the institution (or the body that administers it) has sent a Statutory Educational notice to Copyright Agency Limited (CAL) and been granted a licence. For details of statutory educational and other copyright licences contact: Copyright Agency Limited, Level 15, 233 Castlereagh Street, Sydney NSW 2000. Telephone: (02) 9394 7600. Website: www.copyright.com.au Reproduction and communication for other purposes Apart from any fair dealing for the purposes of study, research, criticism or review, as permitted under the Act, no part of this publication may be reproduced, distributed or transmitted in any form or by any means, or stored in a database or retrieval system, without the written permission of McGraw-Hill Australia including, but not limited to, any network or other electronic storage. Enquiries should be made to the publisher via www.mcgraw-hill.com.au or marked for the attention of the permissions editor at the address below. ly on National Library of Australia Cataloguing-in-Publication Data Author: Paver, Rob. Title: Dermatologic surgery: a manual of defect repair options / Rob Paver, Duncan Stanford, Leslie Storey. s ISBN: 9780070285392 (hbk.) ge Notes: Includes index. Bibliography. Subjects: skin-surgery, surgery, plastic flaps (surgery) Other Authors/Contributors: Stanford, Duncan, Storey, Leslie. Dewey Number: 617.477 pa Published in Australia by McGraw-Hill Australia Pty Ltd Level 2, 82 Waterloo Road, North Ryde NSW 2113 e Publisher: Elizabeth Walton pl Associate editor: Fiona Richardson Art director: Astred Hicks Cover design: Patricia McCallum m Internal design: Astred Hicks and Patricia McCallum Production editor: Michael McGrath sa Copy editor: Marcia Bascombe Illustrator: Chris Welch Proofreader: Terence Townsend Indexer: Shelley Barons CD-ROM preparation: CD-ROM cover and manual design: Typeset in … by Midland Typesetters Printed in China on 105 gsm by iBook Printing Ltd.
- 4. Robert Paver Duncan Stanford Leslie Storey dermatologic SURGERY ly on s ge a M A N U A L of D E F E C T R E PA I R O P T I O N S pa e pl m sa
- 5. sa m pl e pa ge s on ly
- 6. v FOREWORD Over recent decades, Dermatologic Surgery has every cosmetic unit is presented, thus avoiding needless witnessed tremendous growth and evolution. Expansion of repetition. both established procedures, as well as the development Dermatologic Surgery: a manual of defect repair options of new surgical techniques, has led to the division of represents tremendous innovation and a step forward in Dermatologic Surgery into two separate disciplines: Mohs surgical education. The videos show a time sequence Micrographic Surgery/Surgical Repair and Cosmetic dynamic that is difficult to achieve in any other format. Surgery. Certainly, videos of surgical procedures have been used as This text addresses the former; the repair of surgical teaching tools before. Their use, however, has been mostly defects created by the eradication of skin cancers. Every limited to individual case presentations at professional year thousands of Mohs procedures are performed across meetings or personal libraries available only to local the globe, producing their resultant defects. Dermatologic registrars. Now they are available to a more general Surgery: a manual of defect repair options is organized audience of students of all levels. Whether novice or into two complementary sections; a textbook format experienced practitioner, whether trained in dermatology, and corresponding videos. Numerous other texts have plastic surgery, or head and neck surgery, everyone will organized these topics in a similar manner to the written find something to add to their surgical armamentarium. text material presented here. What makes this project The accompanying text is organized in a template unique is supplementing the standard textbook format manner. Each cosmetic unit section is introduced with with an extensive, comprehensive collection of videos a description of the properties of the skin in that unit ly that correspond to the surgical procedures. Cutting-edge as well as the scope of repair options. Individual teaching methods have finally caught up with present-day repairs are illustrated by photographs, line drawings. technology. By being invited into the operating room, on The accompanying text describes the procedure, its advantages disadvantages and caveats, as well as students at all levels are treated to a stunning personal perspective. The experience is like having your own stressing the take-home main points. Another benefit is private expert mentor. that long-term outcomes conclude each picture series. The s The overriding concept here is to perform defect repairs reader will become comfortable with this repetitive format. ge employing principles developed for the cosmetic-subunit Cases with accompanying videos are clearly identified paradigm. These include: if possible, limiting repairs to with an appropriate symbol. one cosmetic unit; placing scar lines in junction lines Surgeons often become proficient with one or two flap pa dividing cosmetic units or the adjoining relaxed skin techniques and try to apply them to all defects. From tension lines and, if most of a cosmetic unit is missing, Dermatologic Surgery: a manual of defect repair options excising the remainder and repairing the whole unit. they will gain a different perspective that may better suit To actually see the application of these principles the defect and, in the long run, the patient. e unfold on screen is a true learning experience. The videos The authors should be congratulated for sharing their pl in particular reveal those aspects of the procedure not expertise. The forethought and time spent to tape and edit readily demonstrated with static two-dimensional pictures. this wide range of reconstructive procedures reveals the These include: flap design and execution, the tension heart of a true teacher/educator. Theirs is a contribution m vector of closure, the effect of the tension vector on free of significant importance. The initial and prime audience margins, how to hold instruments, how to handle tissue is noted to be registrars in training. There is not any sa gently, the extent and level of undermining, final trimming doubt that this will reach and benefit a wider audience. of tissue before closure and the utility of an assistant. The My advice; read the text and view the videos over and procedures range in difficulty from simple to complicated. over again. You will be treated to nuances you didn’t The videos are edited to show only the important stages appreciate before. of the repair and avoid time-consuming repetition. Each type of flap is covered, although not each flap within Stuart J Salasche, MD
- 7. sa m pl e pa ge s on ly
- 8. vii CONTENTS IN BRIEF Foreword v Preface xiv About the authors xvii Acknowledgments xviii SECTION 1 – NOSE 1 SECTION 5 – EARS 242 Chapter 1 Nasal Tip 2 Chapter 21 Upper-third of the Helical Rim 244 Chapter 2 Nasal Ala 28 Chapter 22 Middle-third of the Helical Rim 254 Chapter 3 Nasal Dorsum 56 Chapter 23 Conchal Bowl and External Chapter 4 Nasal Sidewall 70 Auditory Canal 264 Chapter 5 Nasal Root 82 Chapter 24 Anterior Ear 270 Chapter 25 Posterior Ear 282 SECTION 2 – FOREHEAD AND TEMPLE 90 Chapter 26 Ear Lobe 292 Chapter 6 Central Forehead 92 Chapter 7 Lateral Forehead 104 SECTION 6 – PERIOCCULAR 296 Chapter 8 Eyebrow and Suprabrow 116 Chapter 27 Lateral Canthus 299 ly Chapter 9 Temple 126 Chapter 28 Lower Eyelid 306 Chapter 29 on Medial Canthus 320 SECTION 3 – PERIORAL 140 Chapter 30 Upper Eyelid 332 Chapter 10 Lateral Upper Lip and Perialar Region 142 SECTION 7 – SCALP 340 s Chapter 11 Central Upper Lip 160 Chapter 31 Scalp 342 ge Chapter 12 Vermilion Upper Lip 172 Chapter 13 Lateral Lower Lip 178 SECTION 8 – NECK AND MASTOID 354 pa Chapter 14 Central Lower Lip 188 Chapter 32 Neck 356 Chapter 15 Vermilion Lower Lip 194 Chapter 33 Mastoid 364 Chapter 16 Chin 202 SECTION 9 – TRUNK AND LIMBS e 372 SECTION 4 – CHEEKS Chapter 34 Trunk and Limbs 374 pl 208 Chapter 17 Medial Cheek 211 m Chapter 18 Central Cheek 220 Index 388 Chapter 19 Preauricular 230 sa Chapter 20 Mandibular 238
- 9. viii CONTENTS IN FULL Foreword v Preface xiv About the authors xvii Acknowledgment s xviii SECTION 1 NOSE 1 • Composite graft 45 • Nasolabial turnover island pedicle flap (spear flap) 47 • Tunnelled (Kearney) variant of the nasolabial CHAPTER 1 NASAL TIP 2 turnover island pedicle flap 50 • Side-to-side closure 4 • Combined procedure—mucosa, cartilage, and skin 51 • Burow’s exchange advancement flap 6 • Mucosal layer 51 • Bilobed flap (Zitelli variation) 7 • Cartilage layer 52 • Dorsal nasal rotation flap 10 • Skin 55 • Myocutaneous flaps 12 • Unilateral pedicle technique 13 CHAPTER 3 NASAL DORSUM 56 • Horn variation 14 • Side-to-side closure 58 • Bilateral pedicle variation technique 15 • Perialar Burow’s exchange advancement flap 59 • Hunt variation 16 • Subcutaneous island pedicle flap 60 • Rhombic transposition flap 17 • Back-cut rotation flap 62 • Subcutaneous island pedicle flap 18 ly • Bilateral single-sided advancement (T-plasty or A-T) flap63 • Double-rotation flap (Peng variant) 19 • Double-rotation flap (Peng variant) 64 • Two-stage interpolation flap 20 • Rhombic transposition flap on 65 • Two-stage paramedian forehead interpolation flap 20 • Bilobed transposition flap 66 • Two-stage nasolabial interpolation flap 23 • Transposed island pedicle flap 67 s • Full-thickness skin graft 25 • Myocutaneous flap (refer to Chapter 1 Nasal tip) 68 ge • Full-thickness skin graft (refer to Chapter 1 Nasal tip) 69 CHAPTER 2 NASAL ALA 28 Nasal Ala Repairs for Partial Thickness Defects xx CHAPTER 4 NASAL SIDEWALL 70 pa • Side-to-side closure 29 • Side-to-side closure 72 • Bilobed transposition flap (medially or • Advancement flaps 73 laterally based) 30 • Perialar Burow’s exchange advancement flap 73 e • Nasolabial transposition flap (Zitelli variation) 32 • Nasolabial advancement flap 74 pl • Subcutaneous island pedicle flap 34 • Back-cut rotation flap 75 • Rhombic transposition flap 35 • Subcutaneous island pedicle flap 76 m • Myocutaneous island pedicle flap 36 • Transposition flaps 77 • Transposed island pedicle flap 37 sa • Bilobed transposition flap 77 • Shark island pedicle flap 38 • Nasolabial transposition flap 78 • Two-stage nasolabial interpolation flap 40 • Rhombic transposition flap 79 • Full-thickness skin graft 42 • Cheek advancement with Burow’s graft 80 • Second intention 44 • Full-thickness skin graft 81
- 10. Contents ix CHAPTER 5 NASAL ROOT 82 CHAPTER 7 LATERAL FOREHEAD 104 • Side-to-side closure 84 • Side-to-side closure 106 • Rhombic transposition flap 85 • Advancement flaps 107 • Back-cut rotation flap 86 • Unilateral single-sided advancement flap (O-to-L) • Subcutaneous island pedicle flap 87 and Burow’s exchange advancement 107 • Bilateral single-sided advancement • Procerus myocutaneous flap 88 flap (O-to-T) 108 • Side-to-side closure with a V-to-Y advancement from the glabella 89 • Bilateral two-sided advancement flap (O-to-H) 109 • Rotation flap 110 • Rhombic transposition flap 111 SECTION 2 FOREHEAD AND TEMPLE 90 • Skin grafts 112 • Full-thickness skin graft 112 CHAPTER 6 CENTRAL FOREHEAD 92 • Burow’s full-thickness skin graft 113 • Side-to-side (vertical) closure 94 • Split-thickness skin graft 114 ly • Advancement flaps 95 • Unilateral single-sided advancement flap (O-to-L) 95 CHAPTER 8 EYEBROW AND SUPRABROW 116 • Bilateral single-sided advancement flap (O-to-T) on • Side-to-side (horizontal or vertical) closure 118 T-plasty 96 • Advancement flaps 119 • Bilateral two-sided advancement flap (O-to-H) 97 • Unilateral single-sided advancement s • Rotation flap 98 flap (O-to-L) 119 ge • Subcutaneous island pedicle flap 99 • Bilateral single-sided advancement • Skin grafts 100 flap (O-to-T) 120 • Partial closure plus Burow’s graft 100 • Unilateral or bilateral two-sided advancement pa flap (O-to-U or O-to-H) 121 • Partial closure plus second intention 101 • Subcutaneous island pedicle flap 123 • Full-thickness skin graft for the suprabrow 124 e pl m sa Legend Preferred option when a standard side-to-side closure is not possible Sometimes a side-to-side closure can still be used for a medium to large defect
- 11. x DERM ATOLOGIC SU RGE RY A manual of defect repair options CONTENTS IN FULL CHAPTER 9 TEMPLE xx CHAPTER 11 CENTRAL UPPER LIP xx • Side-to-side closure 128 • Vertical Side-to-side closure 162 • Rhombic transposition flap 130 • Wedge excision 162 • Rotation flap 132 • Advancement flaps 163 • Advancement flaps 133 • Uuilateral, single-sided, (crescentic) • Burow’s exchange advancement flap 133 advancement flap 163 • Tripolar (Mercedes) advancement flap 134 • Bilateral, single-sided, advancement (T-plasty or O-T) flap 164 • Unilateral two-sided advancement flap (o-to-U flap) 135 • Bilateral, single-sided, advancement (T-plasty or O-T) flap with a full-thickness wedge 164 • Skin grafts 136 • Unilateral, two-sided advancement flap 165 • Partial closure plus Burow’s full-thickness skin graft 136 • Bilateral, two-sided advancement flap 166 • Full-thickness skin graft 137 • Philtral defects 167 • Split-thickness skin graft 137 • Side-to-side closure 167 • Second intention 138 • Advancement flap (T-plasty) 167 ly • Advancement flap (philtral two-sided) 168 SECTION 3 PERIORAL 140 on • Subcutaneous island pedicle flap 169 • Full-thickness skin graft 170 CHAPTER 10 LATERAL UPPER LIP AND CHAPTER 12 VERMILION UPPER LIP s PERIALAR REGION 142 172 ge • Side-to-side closure 144 • Wedge excision 174 • Wedge excision 146 • Mucosal advancement flap 175 • Rotation flap 148 • Bilateral vermilion rotation flap 176 pa • Advancement flaps 150 • Mucosal V-to-Y island pedicle flap 177 • Burow’s exchange advancement flap 150 • Double advancement (T-plasty or O-T) flap 151 CHAPTER 13 LATERAL LOWER LIP xx e • Crescentic advancement flaps 153 • Wedge excision 182 pl • Crescentic advancement with Burow’s triangle • Burow’s exchange advancement flap 185 in lip rhytides 153 • Rotation flap 186 m • Crescentic advancement with muscle and • Subcutaneous island pedicle flap 187 mucosal wedge 154 sa • Crescentic advancement utilizing a horizontal cut 155 CHAPTER 14 CENTRAL LOWER LIP 188 • along vermilion border 155 • Rotation flap combined with wedge excision 156 • Wedge excision 190 • Transposition flap 157 • Bilateral two-sided advancement flap 192 • Subcutaneous island pedicle flap 158
- 12. Contents xi CHAPTER 15 VERMILION LOWER LIP 194 CHAPTER 19 PREAURICULAR xx • Side-to-side closure 196 • Side-to-side closure 232 • Mucosal advancement flap (surgical vermilionectomy) • Burow’s exchange advancement flap 233 196 • Subcutaneous island pedicle flap 234 • Bilateral vermilion rotation flap 198 • Rhombic transposition flap 235 • Mucosal V-to-Y island pedicle flap 200 • Skin grafts 236 • Wedge excision 200 • Combined flap and Burow’s full-thickness skin graft 236 CHAPTER 16 CHIN 202 • Split-thickness skin graft 237 • Side-to-side closure 204 • Single- or double-rotation flaps 205 CHAPTER 20 MANDIBLE 238 • Rhombic transposition flap 207 • Side-to-side closure 240 • Rhombic transposition flap 241 SECTION 4 CHEEK 208 ly SECTION 5 EARS 242 CHAPTER 17 MEDIAL CHEEK 211 on • Side-to-side closure 212 CHAPTER 21 UPPER-THIRD OF THE HELICAL RIM 244 • Nasolabial advancement flap 213 s • Rotation flap 215 • Side-to-side closure 246 ge • Subcutaneous island pedicle flap 217 • Wedge excision 247 • ‘Banner’ Transposition flap 248 pa CHAPTER 18 CENTRAL CHEEK 220 • Superior helical rim advancement flap 250 • Bilobed transposition flap 251 • Side-to-side closure 222 • Helical crus rotation flap 252 • Advancement flap 223 e • Full-thickness skin graft 253 • Rotation flap 224 pl • Subcutaneous island pedicle 225 • Rotating Lenticular subcutaneous island m pedicle flap 226 • Rhombic transposition flap 228 sa
- 13. xii DER M ATOLOGIC SU RGE RY A manual of defect repair options CONTENTS IN FULL CHAPTER 22 MIDDLE-THIRD OF THE • Split-thickness skin graft 290 HELICAL RIM 254 • Second intention healing 291 • Side-to-side closure 256 • Wedge excision 256 CHAPTER 26 EAR LOBE 292 • Helical rim advancement flap 258 • Side-to-side closure 294 • Helical rim advancement flap • Wedge excision 294 (partial-thickness variant) 260 • Transposition flap—one or two stage 295 • Full-thickness skin graft 261 • Two-stage postauricular pedicle interpolation flap 262 SECTION 6 PERIOCULAR 296 CHAPTER 23 CONCHA BOWL AND EXTERNAL CHAPTER 27 LATERAL CANTHUS 300 AUDITORY CANAL 264 • Side-to-side closure 300 • Full-thickness skin fraft 266 • Rhombic transposition flap 301 ly • Pull-through flap 267 • Advancement flap 302 • Split-thickness skin graft 268 • Rotation flap on 302 • Second intention 269 • Bilobed flap 303 • Full-thickness skin graft 304 CHAPTER 24 ANTERIOR EAR 270 s • Side-to-side closure 272 CHAPTER 28 LOWER EYELID 306 ge • Rotation flap 274 • Side-to-side closure 308 • Full-thickness skin graft 276 • Wedge excision 309 pa • Pull-through flap 277 • Advancement flap 311 • Transposition flap 278 • Rotation flap 312 • Split-thickness skin graft 279 • ‘Banner’ Transposition flap from the upper eyelid 313 e • Second intention 280 • Rhombic transposition flap 314 pl • Subcutaneous island pedicle flap 316 CHAPTER 25 POSTERIOR EAR 282 • Full-thickness skin graft 317 m • Side-to-side closure 284 • Rotation flap 285 CHAPTER 29 MEDIAL CANTHUS 320 sa • Transposition flaps 286 • Side-to-side closure 322 • Rhombic transposition flap 286 • Transposition flap 323 • Bilobed flap 287 • Subcutaneous island pedicle flap 324 • Burow’s exchange advancement flap 288 • Procerus myocutaneous flap 325 • Full-thickness skin graft 289 • glabella back-cut rotation flap 326
- 14. Contents xiii • Full-thickness skin graft 327 SECTION 8 NECK AND MASTOID 354 • Split-thickness skin graft 328 • Second intention healing 330 CHAPTER 32 NECK xx • Z-Plasty repair 331 • Side-to-side closure 358 CHAPTER 30 UPPER EYELID 332 • Bilateral single-sided advancement (T-plasty or O-T) flap 360 • Side-to-side (horizontal) closure 334 • Transposition flaps 361 • Subcutaneous island pedicle flap 335 • Rhombic transposition flap 361 • Wedge excision 336 • Bilobed transposition flap 362 • Advancement flap 337 • skin grafts 362 • Rotation flap 337 • Full-thickness skin graft 338 CHAPTER 33 MASTOID 364 • Side-to-side closure 366 SECTION 7 SCALP 340 ly • Rotation flap 367 • Transposition flap 368 CHAPTER 31 SCALP 342 on • Unilateral or bilateral single-sided advancement flap (Burow’s exchange advancement flap and T-plasty) 369 • Side-to-side closure 344 • Full-thickness skin graft including Burow’s graft 370 • Single and double rotation flaps 346 s • Split-thickness skin graft 371 • Full-thickness skin graft 348 ge • Split-thickness skin graft 349 SECTION 9 TRUNK AND LIMBS 372 • Purse-string closure 350 pa • Variations of second intention healing 351 • Second intention healing 351 CHAPTER 34 TRUNK AND LIMBS 374 • Large flaps with split-thickness graft to the • Side-to-side closure 376 secondary defect 352 e • Tripolar (Mercedes) advancement flap 379 pl • Rotation flap 380 • Rhombic transposition flap 381 m • Subcutaneous island pedicle flap 382 • Keystone island pedicle flap 383 sa • Side-to-side OR FLAP closure with a Burow’s graft 385 • Split-thickness skin graft 386
- 15. xiv DERM ATOLOGIC SU RGE RY A manual of defect repair options PREFACE THE AIM This book is a practical, “how-to-do-it” manual of section. Many of the more difficult periocular defects are cutaneous defect repair options in dermatologic repaired by our visiting oculoplastic surgeons but we surgery. We have compiled all of the repairs that we have limited our discussion to repairs we consider within find useful and that lead to consistently good results, the skill of the typical dermatologic surgeon. and presented them in a logical, consistent format This manual assumes the reader already has basic supported by extensive use of diagrams and skills in cutaneous surgery. The book is not a complete photographs. This is supplemented by a DVD which guide to surgery, and basic aspects of surgery, such closely simulates looking over the shoulder of an as local anesthesia, instrumentation, suturing, skin experienced mentor, which we believe is one of the physiology, preoperative assessment, postoperative care, best ways to learn dermatologic surgery. and management of complications, are not included. While this manual is comprehensive in scope, it does not attempt to cover every repair possible at every site. Certain repairs have not been included as THE TARGET AUDIENCE they are either not performed by the authors or are The manual is primarily aimed at dermatologic surgeons thought to be inferior to the options we do provide. The with good surgical skills who wish to expand their repairs featured in the various sections of the manual knowledge of repair options to allow closure of more ly reflect the experiences of the surgeons at the Skin & difficult defects. However, it also, provides something for Cancer Foundation Australia (Westmead). The nose, for novices looking to extend their skills as well as for the example, is the most common site and one of the most expert preparing a teaching session. While the authors on challenging we operate on. As a result the nose has an are dermatologists, we hope that any practitioner treating extensive section in this manual, whereas the periocular skin cancer, as well as trainees wishing to learn, will find region is a less common site and has a much smaller the manual a useful resource. s ge NECK 1% pa TRUNK AND LIMBS 2% NOSE 41% BCC 92% SCALP 3% PERIORAL AREA 6% e RARER TUMORS 1% CHEEK 9% e.g. MAC, AFX etc. pl SCC 7% m EARS 10% FOREHEAD & sa PERIOCULAR AREA 13% TEMPLE 15% MOHS CASES AT THE SKIN & CANCER FOUNDATION MOHS CASES AT THE SKIN & CANCER FOUNDATION AUSTRALIA, 2007 BY ANATOMICAL SITE AUSTRALIA, 2007 BY HISTOLOGICAL TYPE
- 16. Preface xv THE SKIN & CANCER FOUNDATION THE MANUAL’S FORMAT AUSTRALIA (WESTMEAD) The manual is divided into nine sections representing The Skin & Cancer Foundation Australia (SCFA) is a the various body regions—eight for head and neck, and specialized medical organization dedicated to providing one for trunk and limbs. The head and neck sections are high-quality services in the areas of dermatology and further subdivided into chapters representing the cosmetic dermatopathology. The foundation was established in subunits within each region. Each chapter starts with 1978 in Sydney to provide expert dermatological services an overview and a list of the common repair options and to promote teaching, training, research, and education for that region or subunit. Next, each repair option is related to dermatology. discussed by listing the advantages and disadvantages, The foundation provides an extensive range of teaching to followed by a stepwise description of the technique medical students, nurses, visiting overseas doctors, residents for each procedure. Practical tips are highlighted and and registrars, Mohs Fellows and consultant dermatologists. risks and complications are mentioned where relevant. The Westmead facility was opened in 1994 and is Some repetition is deliberate so that the reader is not the oldest Mohs training unit in Australia. The day surgery constantly turning pages to previous sections. facility has eight operating theaters dedicated to cutaneous The book is extensively illustrated with photos and surgery, 13 dermatologic surgeons and five visiting diagrams, and the accompanying DVD includes over oculoplastic surgeons. Our surgeons perform more than 100 video demonstrations with commentary, providing a 2000 Mohs surgery procedures each year, representing ly “bird’s eye view” of the key points of the operation. These about a quarter of all Mohs cases performed in Australia. are clearly referenced in the text. The following data represents surgical statistics from the on Skin & Cancer Foundation Australia (Westmead) for 2007 A percentage of the proceeds of this book is being donated to the SCFA. s ge 6–10 cm 1% 5–5.9 cm 2% <1 cm 9% 4–4.9 cm 3% SECOND INTENTION 1% pa 3–3.9 cm 10% FLAP 47% OCULOPLASTICS OR PLASTICS 11% e 2–2.9 cm 25% 1–1.9 cm 52% pl GRAFT 14% m sa PRIMARY CLOSURE 27% MOHS CASES AT THE SKIN & CANCER FOUNDATION MOHS CASES AT THE SKIN & CANCER FOUNDATION AUSTRALIA, 2007 BY DEFECT SIZE AUSTRALIA, 2007 BY REPAIR OPTION USED
- 17. xvi DERM ATOLOGIC SU RGE RY A manual of defect repair options PREFACE HOW THE MANUAL CAME ABOUT The idea for this book grew out of the teaching activities initial videos were produced as a learning guide for the performed at the Skin and Cancer Foundation Australia dermatology trainees sitting their exams. (Westmead). While we use all the traditional teaching In 2007 a research fellow at the foundation cataloged methods, we have found that the best method is actually and photo-documented the repairs used to close all Mohs observing the surgery and then performing it with a surgery defects produced at the foundation over a twelve- mentor offering advice along the way. Of course, this is month period. This data was well received when it was not possible for many surgeons. In addition, the closures presented by Dr Leslie Storey at the annual meeting of the vary and a particular closure may not be performed Australasian College of Dermatologists in 2008. very frequently, therefore the visiting surgeon may never It seemed that these two learning experiences—lists see that closure. Consequently, we started videoing of repair options for varying defects in various sites procedures and editing them with a voiceover to produce and videos explaining how to perform each of the short and concise videos that demonstrate important procedures—would be a good combination for teaching aspects of each procedure. This has proven to be a purposes. Initially the thought was to produce a DVD only, valuable learning tool. but the idea grew in discussion between the authors. It The initial videos produced were of basic procedures seemed that a manual with a full description of all the in dermatology, and these have now been successfully options, including illustrations and images of repairs, ly incorporated into a national online teaching program for in combination with a collection of selected videos Australian general practitioners and medical students. This might offer a better all-round teaching aid for those led to the idea of a similar collection of teaching videos seeking information about repairs of cutaneous defects in on for people with more advanced surgical skills and the dermatologic surgery. s ge pa e pl m sa
- 18. xvii ABOUT THE AUTHORS DR ROBERT PAVER MB BS FACD FACMS Rob graduated in Dermatology in 1985 and completed a Mohs Surgery Fellowship in San Francisco in 1987. He established a Mohs Fellowship training program in Sydney in 1991 where he remains the Program Director. Rob is Convenor of the Australasian College of Dermatologists GP Training Task Force and Mohs Fellowship Training Program Task Force. Currently Rob is in private practice in Sydney, a consultant dermatologist at Westmead Hospital and Medical Director at the Skin and Cancer Foundation Australia (Westmead). DR DUNCAN STANFORD MB BS MSC (MED) FACD FACMS Duncan graduated in Dermatology in 2001 and completed his Mohs Surgery Fellowship in Sydney, in 2002. He is a Clinical Senior Lecturer at the University of Wollongong, an Assistant Editor of the Australasian Journal of Dermatology and a member of the Board of Censors for the Australasian College of Dermatologists. Duncan is in private practice on the South Coast of New South Wales, and performs Mohs surgery and laser procedures at the Skin and Cancer Foundation Australia (Westmead). ASSOCIATE PROFESSOR LESLIE STOREY MD FACMS ly Leslie graduated in Dermatology in 2005 and completed a Mohs Surgery Fellowship in Loma Linda, California, in 2006. After completing her Mohs Fellowship she spent two years in Sydney at the Skin and Cancer Foundation, working as a consultant dermatologist and Mohs Surgeon, during which time she set in motion the on process of creating this book. Leslie is currently an Assistant Clinical Professor of Dermatology at the University of California San Francisco in Fresno (UCSF Fresno), and heads its Division of Dermatologic Surgery. She teaches general and surgical dermatology to UCSF s Fresno medical students and UCSF Fresno primary care residents, both through lectures and in the clinic. ge pa e pl m sa
- 19. xviii DER M ATOLOGIC SU RGE RY A manual of defect repair options ACKNOWLEDGMENTS GENERAL ACKNOWLEDGMENT DR ROBERT PAVER The authors would like to acknowledge the tremendous Producing a textbook, and filming and editing videos, contribution the Skin & Cancer Foundation Australia are all very time-consuming processes which have a big (SCFA) has made to the development of dermatology and impact on the daily life, not only of the authors but also in particular, dermatologic surgery, in Australia. It has their families. In that regard I am very lucky to have such provided the facility to build our Mohs surgery unit and to a loving and supportive wife, Deirdre, and four wonderful run our Surgery and Laser Fellowship programs. Without children, all of whom I would like to thank for their this institution, Mohs surgery in Australia would not be as understanding and acceptance of my preoccupation with accessible to patients and trainees as it is today. this project over the past two years. Teaching young and motivated people is one of the My father, Dr Ken Paver, has been an inspirational most rewarding aspects of professional life. A wonderful figure and exceptional role model for me in dermatology thing about teaching is that you also learn from your and in life. He was the driving force behind the students. We would like to thank all the registrars, establishment of the Skin & Cancer Foundation Australia fellows, and consultants who have studied at the Skin & in Sydney. He also realised that Mohs surgery was a new Cancer Foundation Australia. Many of the things we have frontier for dermatology and, as a result, arranged for Prof included in this book have evolved through the process of Perry Robins in 1978 and Prof Ted Tromovitch in 1981 to teaching. visit Sydney as keynote speakers for foundation seminars, Working in a large facility with many other doctors to help establish Mohs surgery in Australia. ly provides a wonderful environment for the exchange As a result of their visits I was enthused by the concept of ideas and professional development. Many of the of Mohs surgery and applied for the Mohs surgery on consultants at the foundation have directly and indirectly fellowship with Drs Tromovitch, Stegman, and Glogau in contributed to this publication. We would like to thank San Francisco. They accepted my application and I am them all, but in particular, Dr Chris Kearney, Dr Shawn eternally grateful to them for their excellent teaching and s Richards, Dr Michelle Hunt, Dr Howard Studniberg, mentoring. Dr Rhonda Harvey, and Dr Paul Salmon from New Finally, and most importantly, the production of this ge Zealand, who have all contributed images for the book. book has been a joint effort of the three authors. I feel McGraw-Hill have been absolutely first class in the way blessed to have been able to work on this project with they have helped us as novice authors. We would like such wonderful people. Their enthusiasm and never pa to thank their whole team, but in particular, Lizzy Walton complaining attitude has made a large and complicated (Publisher—Medical Division), Fiona Richardson (Associate task so much easier. I have thoroughly enjoyed working editor), Michael McGrath (Senior production editor), and with them and I would to thank them for that privilege. e Astred Hicks (Art director), as well as Chris Welch, our brilliant illustrator. pl m sa
- 20. Acknowledgments xix DR DUNCAN STANFORD DR LESLIE STOREY I am truly a fortunate ‘child’ of the Skin & Cancer I owe a great deal to the Skin & Cancer Foundation Foundation Australia: initially as a dermatology trainee, Australia, and specifically to Rob Paver, for the then as a Mohs Fellow, and now as a consultant. I owe opportunity to work in Australia. I have learned an a great debt to the remarkable Rob Paver, as well as to immense amount directly from working with both Rob as Shawn Richards, Michelle Hunt, and Howard Studniberg. well as Duncan Stanford. All the surgeons at the Skin All of them have been so generous with their time and & Cancer Foundation have taught me some aspect of sage advice, and their superb work sets such a high dermatologic surgery. I would like to thank Dr Artemi, standard to aspire to. Dr Kearney, Dr Hunt, Dr Satchel, Dr See, Dr Kalouche, The lovely Leslie Storey was a bright light at the Dr Lee, Dr Studniberg, and Dr Richards. I would also like foundation for two years and she left such an impact that to thank Dr Abel Torres who was my first mentor. we still greatly miss her. I have a lot to thank her for but My experience overseas would not have been possible single out her quiet resolve to excel, which pushed us all without the loving support of my mother, father, brothers, to try new things (including writing a book). I, too, would husband, and three children. My husband, Wes, has like to thank Rob and Leslie for the honor of working on been my pillar of strength throughout our life together. this project with them. My mother and father taught me the importance of hard My wife, Lucie, and my two daughters, who I love work and the need to continually learn. They have been so dearly, have shown great tolerance and forbearance outstanding role models. ly as I’ve worked on this somewhat daunting project. As a medical educator, Lucie has also been able to give wise on counsel during the later stages of the book’s development. s ge pa e pl m sa
- 21. 126 sa m pl e pa ge s on ly
- 22. 127 CHAPTER TEMPLE 9 The temple is a common area for skin cancer. As discussed in the REPAIR OPTIONS: introduction to this section, the most important issues in this area are the danger zone for the temporal branch of the facial nerve TEMPLE and the superficial temporal artery. The temporal branch of the • Side-to-side closure facial nerve innovates to the frontalis muscle and gives rise to the • Rhombic transposition flap movements of facial expression for the eyebrows and forehead. • Rotation flap The area is composed of skin, subcutaneous fat, superficial • Advancement flaps temporal fascia (STF), deep temporal fascia (DTF), and temporalis muscle. The nerve lies immediately beneath the STF. The course • Burow’s exchange advancement flap of the nerve places it at risk of injury during surgery over the • Tripolar (Mercedes) advancement zygomatic arch and on the temple and lateral forehead. Its usual flap course is from a point 5 mm below the tragus to a point 15 mm • Unilateral two-sided advancement above the lateral extremity of the brow. Over the zygomatic arch, flap it is found about 2.5 cm lateral to the lateral canthus, placing it • Skin grafts about halfway between the lateral canthus and the superior helix ly • Partial closure plus Burow’s (see page 105 for a diagram of the facial nerve). full-thickness skin graft on There are several considerations when choosing a closure for • Full-thickness skin graft a temple defect. Any closure in this area can put tension on the • Split-thickness skin graft lateral canthus or the eyebrow. A small amount of distortion is s acceptable as it will settle after a few weeks. Extra tension can • Second intention ge leave the patient with a raised eyebrow or distortion of the lateral canthus and eyelids. pa Side-to-side closure is often possible due to the laxity in the preauricular region beneath the temple. Redundant skin from this area can also be advanced, transposed or rotated superiorly. If e none of these is an option, skin grafts may be used. If the defect pl is located in the concave area of the temple, second intention healing is also an option. m Preferred options when standard side-to-side closure sa is not possible
- 23. 128 DER M ATOLOGIC SU RGE RY A Manual of Defect Repair Options TEMPLE SIDE-TO-SIDE CLOSURE ADVANTAGES DISADVANTAGES • The closure stays within the surgical area • A long, straight line results from closure of larger • Scars can sit within, run parallel to, or are defects extensions of, the radial rhytides emanating from the lateral canthus (crow’s feet) • Suitable for closure of quite large defects A B ly C Figure 9.1 Horizontal side-to-side closure with M-plasty on at the medial end in the crow’s feet rhytides. An M-plasty at the lateral canthus is an excellent technique to shorten the length of an ellipse for closure of large defects on the temple. s ge pa e pl m sa
- 24. Temple C H A P TER 9 129 TECHNIQUE Using skin hooks, test for the best direction of closed horizontally or obliquely with a large 1 closure. Ellipses are often best oriented in a radial ellipse to prevent tension on the lateral eyelids. fashion as an extension of the creases radiating out from the lateral canthus in horizontal and Undermine in the subcutaneous plane avoiding 2 oblique directions. Rarely for small defects the nerves and vessels. oriented vertically, a vertical ellipse is required. After hemostasis is achieved, place a few Place the skin hooks on the medial and lateral 3 absorbable sutures to close the defect. borders and pull the defect closed to evaluate any tension on the eyebrow or eyelids. Sometimes Insert the superficial sutures. 4 these vertically shaped defects still need to be A B ly on s ge C Figure 9.2 Side-to-side closure oriented obliquely radiating out from the lateral canthus pa e pl m sa
- 25. 130 DER M ATOLOGIC SU RGE RY A Manual of Defect Repair Options RHOMBIC TRANSPOSITION FLAP SEE VIDEO 38 I TEMPLE RHOMBIC TRANSPOSITION FLAP ADVANTAGES DISADVANTAGES • Utilizes skin laxity from cheek and preauricular • For small to medium-sized defects only region • Pincushioning may occur • Good skin match • Care must be taken to avoid moving hair onto the temple A B ly on s ge C pa Figure 9.3 Rhombic transposition flap sourced from skin lateral and inferior to the defect e pl m sa
- 26. Temple C H A P TER 9 131 TECHNIQUE Refer to Figure 1.18 in Chapter 1 Nasal tip (page 17). plane around the defect and, in particular, the skin inferior to the flap where the skin laxity is Draw a line from the defect toward the area of found. 1 skin laxity medial or lateral to the defect and parallel to an imaginary extension of the crows After hemostasis is achieved, place the first 4 feet across the temple. subcutaneous suture to close the donor site, pulling the skin up from the cheek towards the Draw the second line from the end of the first, zygoma. 2 angling at 60 degrees away from the first line and down towards the cheek. It should be the same Trim the flap to fit the defect. Some surgeons 5 length as the first line. prefer to extend the defect into a geometric shape for the flap to sit in, believing that geometric Anesthetize the area and incise the flap. shapes leave less scarring. A few absorbable 3 Undermine the flap superficially in the sutures may then be inserted around the flap. subcutaneous plane avoiding the temporal branch of the facial nerve and the temporal artery if Insert the superficial sutures. 6 possible. Also undermine widely in the superficial A B ly on s ge C pa Figure 9.4 A transposition flap from skin medial and inferior to the defect can move a long way up onto the temple due to the laxity of the cheek, allowing substantial advancing movement of the flap up over e the zygoma as well as transposing into the defect. pl m sa
- 27. 132 DER M ATOLOGIC SU RGE RY A Manual of Defect Repair Options ROTATION FLAP SEE VIDEO 39 AND 40 I TEMPLE ROTATION FLAP AND TEMPLE ROTATION FLAP (LARGE) ADVANTAGES DISADVANTAGES • Suitable for closure of medium to large defects • Lateral eyebrow may be twisted upward a little • A curving variation of the Burow’s exchange • Care must be taken not to injure the nerve when advancement flap undermining and watch for the arteries • A portion of the scar will hide in the rhytides, along • Care must be taken to avoid moving hair onto the the hairline and in the hair itself temple • Scar may be visible where it runs obliquely across the temple TECHNIQUE Refer to the technique described for a rotation flap in arc needs to be approximately two to three times Chapter 7 Lateral forehead and Figure 7.4 (page 110). the size of the defect. Draw an arc from the superolateral aspect of the After anesthesia is obtained, incise the flap and 1 4 defect in or adjacent to the hairline, similar to undermine in the superficial plane (to avoid the single-sided advancement flap but curving injury to the facial nerve). Also undermine the laterally and inferiorly toward the preauricular skin inferior to the flap down onto the cheek to area. allow upward movement of the flap with suturing. The rotation pucker is then excised to produce an For defects not adjacent to the hair the arc will ly 2 oblique line across the temple. need to curve around beneath the hairline to avoid moving hair out onto the temple, while for defects adjacent to the hair the arc can run in the 5 on After hemostasis is achieved, place absorbable sutures to pull the flap across the defect. The hairline and down in front of the ear. remaining absorbable sutures are placed along the arc following the rule of halves principle. s Now draw the rotation pucker at the anterior 3 ge edge of the defect. The area of the flap within the Insert the superficial sutures. 6 pa A B C e pl m sa Figure 9.5 Rotate flap for a defect on the temple
- 28. Temple C H A P TER 9 133 ADVANCEMENT FLAPS BUROW’S EXCHANGE ADVANCEMENT FLAP SEE VIDEO 41 I TEMPLE BUROW’S EXCHANGE ADVANCEMENT FLAP ADVANTAGES DISADVANTAGES • Utilizes skin laxity from the temple and lateral • Possible eyebrow elevation cheek • Not as good for large, vertically oriented defects • Suitable for closure of medium to large defects • Can cause reorientation of the skin rhytides TECHNIQUE Outline the flap by drawing a line from the After hemostasis is achieved, place absorbable 1 4 inferolateral border of the defect down the sutures to advance the flap superiorly over the preauricular fold. The line may extend beyond the defect. insertion of the ear lobe for maximum mobility of Excise the standing cone deformity and the flap. Draw a triangle where the standing cone 5 approximate the edges with deep absorbable deformity will be located medial to the defect and sutures. oriented obliquely across the temple. If the line in the preauricular fold, or along the Alternatively draw a line from the inferolateral 6 2 orbital ring, can be closed by the rule of halves border of the defect, around the orbital rim to the principle, it should be. Sometimes for large crows feet at the lateral canthus. Draw a triangle defects a Burow’s triangle will need to be removed where the standing-cone deformity will be ly from beneath the ear lobe or in the crow’s feet. located, lateral to the defect and up into the hair line. on A few absorbable sutures may be placed along the 7 flap edges. Incise the flap and undermine in the 3 subcutaneous plane. Insert the superficial sutures. 8 s ge pa Courtesy of Dr Chris Kearney A B C e pl m sa Figure 9.6 A Burow’s exchange advancement flap around the orbital rim to the crow’s feet
- 29. 134 DER M AT OLOGIC SU RGE RY A Manual of Defect Repair Options ROATION FLAP continued TRIPOLAR (MERCEDES) ADVANCEMENT FLAP ADVANTAGES DISADVANTAGES • Suitable for closure of medium-sized defects • Possible eyebrow or eyelid distortion • A portion of the scar can hide within the horizontal • A portion of the scar is noticeable rhytides TECHNIQUE1 Undermine widely around the defect. triangles then confirm or remark the redundant 1 cones. Using skin hooks, pull defect edges together in 2 multiple directions to gauge the directions of Incise and remove these triangles. 4 greatest movement. Most laxity will always be found to be inferior to the defect. Use the skin After hemostasis is achieved, place several 5 marker to outline the potential triangular cones absorbable sutures with the first suture closing the of redundant skin. vertical line then other deep sutures to fully close the defect. Place a buried purse-string type suture connecting 3 Insert the superficial sutures. the center of all three sides of the outlined 6 ly on Figure 9.7 Tripolar advancement flap s ge A B pa e pl m sa Figure 9.8 Tripolar advancement flap
- 30. Temple C H A P TER 9 135 UNILATERAL TWO-SIDED ADVANCEMENT FLAP (O-TO-U FLAP) ADVANTAGES DISADVANTAGES • Utilizes skin laxity from beneath the defect • Anterior vertical line may be visible • Suitable for closure of medium to large defects which are more square in shape TECHNIQUE Outline the flap by drawing vertical lines down After hemostasis is achieved, place absorbable 1 3 from the inferolateral corner of the defect in sutures to advance the flap superiorly over the the hairline and from the inferomedial corner defect. down to the crow’s feet adjacent to the lateral canthus. Draw triangles where the standing cone Excise the standing cone deformities and 4 deformities will be located in the crow’s feet approximate the edges with deep absorbable medially and in the sideburn region laterally. sutures. The flap should be broader at its base than at the A few absorbable sutures may be placed along the leading edge. 5 flap edges. Incise the flap and undermine in the Insert the superficial sutures. 2 6 subcutaneous plane. A B ly on s ge pa e pl Figure 9.9 Design of the unilateral two-sided advancement flap for a square-shaped medium to large defect on the temple. This flap is not commonly used and is best considered when the medial vertical edge of the defect is too long m for an M-plasty or rotation-pucker repair as part of a unilateral advancement flap or rotation flap. sa
- 31. 136 DER M ATOLOGIC SU RGE RY A Manual of Defect Repair Options SKIN GRAFTS PARTIAL CLOSURE PLUS BUROW’S FULL-THICKNESS SKIN GRAFT As part of a combined repair, excised standing cones from a partial side-to-side closure or a flap repair, such as a tripolar advancement flap, may be used as full-thickness skin grafts to fill the residual defect. ADVANTAGES DISADVANTAGES • Closure of the donor site reduces the defect size • Grafts are more obvious scars than flaps but • No need for separate donor site repair smaller grafts are preferable to larger grafts • Good color, texture, and contour match. Some defatting of the grafts is still necessary and grafts are cut to fit, and sutured in position in the standard manner. A B ly on s C Figure 9.10 Side-to-side closure with M-plasty and ge Burow’s graft to the residual central defect pa e pl m sa
