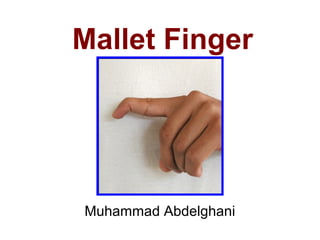
Mallet finger
- 1. Mallet Finger Muhammad Abdelghani
- 2. Finger extensor mechanism anatomy Lateral view Dorsal view DIP = distal interphalangeal joint MCP = metacarpophalangeal joint ORL = oblique retinacular ligament PIP = proximal interphalangeal joint TRL = transverse retinacular ligament.
- 3. Anatomy • The extrinsic extensor tendon: – Originates in the forearm. – Courses over the MCP joint. – Has an indirect attachment to the proximal phalanx. • The primary extensor force across the MCP joint is transmitted through the sagittal band connections to the volar plate. – The tendon trifurcates over the proximal phalanx.
- 4. Anatomy • Central slip: – The central continuation of the extensor tendon. – Attaches to the dorsal base of middle phalanx. – Exerts an extensor force across the PIP joint.
- 5. Anatomy • Interossei and lumbricals: – Provide the intrinsic contribution to extensor mechanism. – Form a lateral band on each side of the digit, passing volar to the MCP joint. – The lateral bands join with the lateral slips of the extrinsic extensor tendon at the level of PIP joint to form the conjoined lateral bands. – The two conjoined lateral bands then converge dorsally and insert at the base of the distal phalanx as the terminal extensor tendon.
- 6. Anatomy • The other components of the extensor apparatus stabilize the extensor hood and coordinate joint movement.
- 7. Anatomy • Triangular Ligament: – A thin tissue connecting the conjoined lateral bands over the middle phalanx. – Prevents separation and volar migration of the lateral bands when the PIP joint is flexed.
- 8. Anatomy • Transverse Retinacular Ligaments: – Originate from each side of the PIP joint volar plate. – Insert dorsally into the adjacent conjoined lateral band. – Stabilize and limit dorsal migration of the lateral bands during PIP joint extension.
- 9. Anatomy • Oblique Retinacular Ligaments: – Arise from the flexor tendon sheath and volar aspect of the proximal phalanx. – Course distally to insert onto the dorsal base of the distal phalanx with the terminal extensor tendon, thus linking and coordinating PIP and DIP joint motion.
- 10. Mallet Finger • An injury that involves disruption of the extensor mechanism at the level of the distal interphalangeal (DIP) joint.
- 11. Alternative Names • Baseball finger • Drop finger
- 12. Epidemiology • Usually occurs in work environment or during sports participation. • Most frequently involved digits: long, ring, and small fingers of the dominant hand. • Age and Sex: – Often seen in young to middle-aged males. – Women with this injury tend to be older.
- 13. Genetic Predisposition • Most mallet fingers are caused by a traumatic event. • However, Jones and Peterson found an unusually high incidence in a three-generation family, with 85% of the lesions developing spontaneously or after minimal trauma. • The authors proposed a possible genetic predisposition toward mallet finger deformity in certain individuals.
- 15. Mechanism of Injury • Most common mechanism: – Sudden forced flexion of the extended fingertip. – This results in either: • stretching or tearing of extensor tendon substance or • avulsion of tendon insertion from the dorsum of distal phalanx, with or without a fragment of bone.
- 16. Mechanism of Injury • Less frequent mechanism: – Forced hyperextension of the DIP joint. – This causes fracture at the dorsal base of the distal phalanx. • Open injuries are caused by a laceration, crush, or deep abrasion.
- 17. Pathoanatomy • A well-balanced system exists between intrinsic and extrinsic tendons, and between flexion and extension forces across each finger interphalangeal (IP) joint.
- 18. Pathoanatomy • Any injury causing a flexion or extension deformity in one IP joint can lead to tendon imbalance, creating an opposite deformity in the adjacent IP joint. – At DIP joint: FDP flexion force is counterbalanced by the terminal extensor tendon. – At PIP joint: flexion forces of the FDP and FDS tendons are counterbalanced by the extension forces of the conjoined lateral bands and the central slip of extensor apparatus.
- 19. Balance between flexion and extension forces at the finger joints The single dots represent the axes of flexion-extension at each joint. The double dots represent the areas of action of the corresponding tendons at each joint.
- 20. Pathoanatomy • With a mallet injury, the delicate balance between flexion and extension forces is disrupted. • The following sequence of events occurs: – Discontinuity of the terminal extensor tendon – Migration of extensor apparatus proximally – Increased extensor tone at PIP relative to DIP joint. – Early or late swan neck deformity (hyperextension of PIP joint with concomitant flexion of DIP joint) can occur.
- 21. Classification Acute vs. Chronic • Acute mallet deformities = those occurring within 4 weeks of injury. • Chronic deformities = those presenting later than 4 weeks from injury.
- 23. Classification Doyle Classification • Type I: Closed injury, with or without a small avulsion fracture at the dorsal base of distal phalanx. • Type II: open tendon injuries caused by laceration at or around the DIP joint. • Type III: also open injuries; they occur from a deep soft-tissue abrasion with loss of skin and tendon substance. • Type IV: mallet fractures
- 24. Classification Subclassifications of Type IV Injuries • Damron & Engber: – IVA: Distal phalanx physeal injuries in children. – IVB: Distal phalanx fractures in adults involving 20%- 50% of the joint surface. – IVC: • Hyperextension injuries, resulting in a fracture fragment >50% of the distal phalanx articular surface. • Associated with DIP joint volar subluxation. • Wehbé & Schneider: – Subclassification based on fracture size and presence or absence of DIP joint subluxation.
- 25. Clinical Evaluation • Recognition and diagnosis of a mallet finger are relatively straightforward. • Patients present with pain, deformity, and/or difficulty using the affected finger.
- 26. Clinical Evaluation • Inspection: – Soft tissues – Deformity: • Most patients develop an extensor lag at the DIP joint immediately after injury. • The deformity may be delayed by a few hours or even days. • Concurrent hyperextension of the PIP joint (ie, swan neck posture) may be noted with active finger extension.
- 27. Clinical Evaluation • Palpation: – Tenderness can be elicited in acute injuries with palpation over the dorsal margin of DIP joint. • ROM: – Measure finger MCP and PIP joint motion.
- 28. Radiographic Evaluation • Posteroanterior, oblique, and lateral radiographs of the digit are recommended to assess for bone injury and joint alignment.
- 29. Neglected Injuries • Neglecting mallet injury often results in permanent stiffness and deformity at the DIP joint level.
- 30. Treatment Options • Non-surgical: –Successful in most mallet injuries. • Surgical: –Treatment of either an acute or a chronic mallet finger –Salvage of failed prior treatment
- 31. Treatment Options • Many splint configurations and surgical techniques have been described over the last century. • However, the optimal treatment of each type of mallet finger injury remains controversial.
- 32. Definition of satisfactory outcome (Geyman et al.) • DIP joint exhibits a residual extensor lag ≤20° • DIP flexion arc is ≥50° • Patient reports minimal or no pain.
- 33. Management of Acute Mallet Finger Injuries Nonsurgical • Indications: –Type I mallet injuries – Closed mallet fractures involving less than one third of the articular surface with no associated DIP joint subluxation.
- 34. Management of Acute Mallet Finger Injuries Nonsurgical • Outcome: – About 80% of closed injuries will heal with 6 (tendinous)—8 (bony) weeks of splintage with a further 2 weeks at night. – If the tendon does not heal within this period of time further splintage can be successful. – If this fails, open repair may be considered. – Controversy exist regarding: • style of splint • duration of immobilization necessary for acceptable outcome
- 35. Management of Acute Mallet Finger Injuries Nonsurgical • Immobilization of both PIP and DIP joints was previously thought to be necessary to relax the extensor hood and intrinsic musculature during terminal extensor tendon healing. • However, Katzman et al demonstrated that only the DIP joint need be immobilized in extension to allow healing of the mallet injury.
- 36. Management of Acute Mallet Finger Injuries Nonsurgical • Most authors currently advocate immobilization of the DIP joint alone. • In the presence of a swan neck deformity, however, temporary inclusion of the PIP joint in flexion has been suggested. • Combined PIP and DIP joint splinting has not been conclusively proved to restore tendon balance in a swan neck deformity.
- 37. Management of Acute Mallet Finger Injuries Nonsurgical Splinting • Numerous splints have been devised for managing mallet finger injuries. • Common examples: – The stack splint – The perforated thermoplastic splint – The aluminum foam splint
- 39. Three different mallet finger splints A, Stack splint (Stax Finger Splint, Sammons Preston Rolyan, Bolingbrook, IL) B, Perforated thermoplastic splint (Aquaplast Splinting Material, Sammons Preston Rolyan) C, Aluminum foam splint
- 40. Management of Acute Mallet Finger Injuries Nonsurgical Splinting • ‘Mexican hat’ splint: – Incorporates a “buckle” over the DIP joint to alleviate undue pressure on the healing terminal extensor tendon. • A sterilized aluminum splint secured with sterile tape strips has been proposed to treat mallet injuries in operating room personnel.
- 41. Management of Acute Mallet Finger Injuries Nonsurgical Splinting • Many splints, same treatment principles: – The digit is immobilized in full extension or slight hyperextension across the DIP joint. – Avoid excessive extension because dorsal skin vascular compromise can occur when the joint is immobilized in > 50% of the normal range for passive DIP joint hyperextension.
- 42. Management of Acute Mallet Finger Injuries Nonsurgical Splinting • Instruct the patient on how to change the splint for periodic cleaning and examination of the skin without allowing the DIP joint to flex. – Continuous immobilization: 6-8 weeks. – Nighttime splinting: 2 weeks. • A new full-length course of immobilization is recommended when the DIP joint is inadvertently flexed during treatment.
- 43. Management of Acute Mallet Finger Injuries Nonsurgical Splinting • Requirements for successful splinting: – Frequent physician assessment (check films in the splint over the first 2 weeks) – Patient compliance
- 44. Management of Acute Mallet Finger Injuries Nonsurgical Splinting • A small residual extensor lag and radiographic evidence of DIP joint osteoarthritis do not preclude a successful treatment result.
- 45. Management of Acute Mallet Finger Injuries Nonsurgical Casting • Infrequently used technique. • May be beneficial in: – Children – patients deemed noncompliant with splint treatment • Described by Smillie (1937) for acute mallet finger injuries. • Both IP joints are casted: – PIP joint in 60° of flexion – DIP joint in slight hyperextension • Inclusion of PIP joint in flexion prevents a tubular cast from inadvertently falling off the finger.
- 46. Management of Acute Mallet Finger Injuries Surgical Type I Injury • Splinting is the treatment of choice. • Surgical indications: – Individuals unable to comply with a splinting regimen – Patients who would have difficulty performing their jobs with an external splint (eg, surgeons, dentists, musicians).
- 47. Management of Acute Mallet Finger Injuries Surgical Type I Injury • To immobilize the DIP joint in extension, a transarticular K-wire is driven longitudinally or obliquely across the DIP joint. – The tip of the wire is buried in the middle phalanx. – The distal end is either capped or cut beneath the skin surface. • Post-Operatively: – K-wire is removed after 6-8 weeks. – This is followed by 2 weeks of nighttime extension splinting.
- 48. Management of Acute Mallet Finger Injuries Surgical Open Injuries (Types II and III) • Open mallet injuries require surgical repair. • Various surgical methods have been described.
- 49. Management of Acute Mallet Finger Injuries Surgical Open Injuries (Types II and III) • The tendon can be repaired separately from the skin. • However, as there is little subcutaneous tissue: – The repair material may be superficial – Successful results have been achieved with a mass repair of tendon and skin. • A K-wire through the DIP joint is useful to stabilise the repair while the tendon heals. • If the tendon ends are damaged a turndown of one lateral band can be used to strengthen the repair. – This method may also be useful for chronic mallet injuries.
- 50. Management of Acute Mallet Finger Injuries Surgical Open Injuries (Types II and III) • Doyle: – A combination of surgical repair and splinting for acute tendon lacerations overlying the DIP joint. – A running suture is used to reapproximate both skin and tendon, followed by application of an extension splint. – The suture is removed after 10-12 days. – Splinting is continued for 6 weeks.
- 51. Management of Acute Mallet Finger Injuries Surgical Open Injuries (Types II and III) • Type III mallet deformities: – Involve loss of skin, subcutaneous tissues, and tendon substance. – Caused by deep abrasions, crush injuries, and degloving accidents. – Often difficult to treat because of exposure of both bone and articular cartilage. – Staged reconstructive surgery may be considered: • Early skin coverage is followed by restoration of extensor tendon function with insertion of a free tendon graft. – In severe cases, DIP arthrodesis with bone shortening or fingertip amputation may be more appropriate.
- 52. Management of Acute Mallet Finger Injuries Surgical Mallet Fracture (Type IV) • Management strategies for the different subtypes of mallet fractures remain controversial. • Treatment alternatives: – Observation with reassurance – Extension splinting – Closed and open reduction with internal fixation – DIP joint arthrodesis.
- 53. Management of Acute Mallet Finger Injuries Surgical Mallet Fracture (Type IV) • A true lateral radiograph of the injured digit is valuable for determining: – size and displacement of fracture fragment – presence or absence of volar subluxation of the distal phalanx. • Closed mallet fracture injuries involving less than one third of the articular surface and without DIP joint subluxation can be reliably treated with extension splinting alone. • Wehbé & Schneider and Schneider advocated nonsurgical management of nearly all mallet fractures, regardless of the size or displacement of the fracture fragment or the presence of volar subluxation of the distal phalanx.
- 54. Calculations for determining fracture fragment size, fragment displacement, and distal interphalangeal joint subluxation. A and B = the length of the involved bone segments at the articular surface of the distal phalanx, C = the amount of fracture fragment displacement, D = the distance between the midaxial lines of the middle and distal phalanges.
- 55. Management of Acute Mallet Finger Injuries Surgical Mallet Fracture (Type IV) • Disadvantages of surgical treatment of mallet fractures: – Technically demanding – Higher complication rate than nonsurgical management • A dorsal prominence overlying the DIP joint may follow nonsurgical treatment. – This same deformity is seen in the surgically treated patients.
- 56. Lateral radiograph of a remodeled mallet fracture The arrows indicate the old fracture line. The distal interphalangeal joint remains congruent.
- 57. Management of Acute Mallet Finger Injuries Surgical Mallet Fracture (Type IV) • Indications for surgical intervention: –Mallet fractures involving more than one third of articular surface – Fractures with associated DIP joint subluxation
- 58. Management of Acute Mallet Finger Injuries Surgical Mallet Fracture (Type IV) • Techniques: – Transarticular pinning of DIP joint ± fracture fragment fixation – Tension band constructs – Compression pinning – Extension block pinning • All of these techniques involve placement of at least one K-wire to immobilize the DIP joint in extension.
- 59. Extension block pinning technique A, With the distal phalanx extended, a K-wire is inserted proximal to the fractured fragment. B, The fracture is reduced manually by directing the exposed end of the K-wire distally. C, The wire is drilled into the head of the middle phalanx, and a second wire is passed retrograde across the distal interphalangeal joint.
- 60. Management of Acute Mallet Finger Injuries Surgical Mallet Fracture (Type IV) • Open vs. Closed Reduction: – Proponents of open reduction think that associated complications can be minimized by using meticulous surgical technique. – Closed reduction with percutaneous pinning has been advocated by surgeons who are concerned about complications with open management. – They cite problems related to reducing the small articular fragment, the inability to accurately assess DIP joint congruency, and the potential for injury to the tenuous soft-tissue envelope.
- 61. Management of Chronic Mallet Finger Injuries • Patients who present for treatment > 4 weeks after injury typically report pain, dissatisfaction with the appearance of the digit, and interference with use of the finger for normal work and recreational activities. • As with acute mallet injuries, both nonsurgical and surgical treatment measures have been advocated.
- 62. Management of Chronic Mallet Finger Injuries Nonsurgical • Continuous extension splinting (10 weeks) should be considered as an alternative to surgery for a chronic mallet finger deformity (Patel et al., 1986).
- 63. Management of Chronic Mallet Finger Injuries Nonsurgical • Garberman et al found no differences in outcome between patients splinted early (<2 weeks after injury) and late (>4 weeks after injury). • They recommended DIP joint extension splinting for closed mallet injuries regardless of chronicity, including fractures involving less than one third of the joint surface. • Brzezienski and Schneider advocated splinting for all chronic mallet deformities resulting from either neglect or previous failed treatment.
- 64. Management of Chronic Mallet Finger Injuries Surgical • Rationale of surgery: – Chronic mallet finger may develop pathologic features that interfere with treatment results. – A static contracture of the extensor mechanism can develop over time, making it difficult to achieve apposition of the tendon ends with simple extension splinting.
- 65. Management of Chronic Mallet Finger Injuries Surgical Surgical procedures for chronic mallet finger: • Aims: – to stabilize the DIP joint – to improve active DIP joint extension. • Examples: – Terminal extensor tendon shortening – Tenodermodesis – Oblique retinacular ligament reconstruction – Fowler’s central slip tenotomy
- 66. Management of Chronic Mallet Finger Injuries Surgical • The abbreviato operation (Lind & Hansen, 1989): – The extensor tendon is transected near the DIP joint and repaired directly, without overlapping and without excision of damaged tendon tissue. – Scar contraction at the repair site is thought to correct the flexion deformity. – A transarticular pin is used to immobilize the DIP joint in extension for 6 weeks. – Timing: • The authors recommended performing the procedure within 3 months of injury in patients with marked ligamentous laxity to avoid progression to a swan neck deformity. • However, the procedure is not recommended before 6 months to allow potential spontaneous correction of the extensor lag.
- 67. Management of Chronic Mallet Finger Injuries Surgical • Tenodermodesis: – Originally described by Iselin et al. – Used to manage chronic mallet finger deformities in both adults and children. – Technique: • An elliptical wedge of skin, tendon, and scar tissue is resected. • The skin and tendon are reapproximated as a single unit with sutures. • Similar to the abbreviato operation, a temporary K-wire is used to maintain the DIP joint in full extension during the healing process.
- 68. Tenodermodesis Procedure In the tenodermodesis procedure, a 3- to 4- mm elliptical wedge of skin, subcutaneous tissue, and tendon/scar is resected. A, The full-thickness defect is repaired with nonabsorbable sutures. B, Before securing the sutures, the distal interphalangeal joint is immobilized in extension with a Kirschner wire.
- 69. Management of Chronic Mallet Finger Injuries Surgical • Spiral Oblique Retinacular Ligament Reconstruction: – Originally reported by Thompson et al; later modified by Kleinman and Petersen. – Addresses the imbalance of flexion and extension forces contributing to a chronic mallet deformity. – Restores the dynamic tenodesis effect of the oblique retinacular ligaments in coordinating PIP and DIP joint extension. – A free tendon graft is harvested and secured distally to the dorsal base of distal phalanx. – The graft is passed volarward in a spiral fashion around the radial aspect of the middle phalanx and is secured proximally to the ulnar side of the flexor tendon sheath at the level of the proximal phalanx or directly to bone. – The PIP and DIP joints are temporarily immobilized with K-wires before initiating finger motion exercises.
- 70. Spiral oblique retinacular ligament reconstruction A, Lateral view. The tendon graft is secured to the dorsum of the distal phalanx with a pullout suture or wire. The graft is passed along the radial border of the middle phalanx, deep to the neurovascular bundle and volar to the flexor tendon sheath. B, Volar view. The graft is then sutured to the ulnar edge of the flexor tendon sheath at the level of the proximal phalanx.
- 71. Management of Chronic Mallet Finger Injuries Surgical • Fowler’s Central Slip Tenotomy: – Aim: To correct for increased extensor tone at the PIP joint resulting from retraction of the extensor apparatus. – Timing: • The operation should be delayed until at least 3 months after injury to allow restoration of terminal extensor tendon continuity by scar tissue (Houpt et al, 1993). – To prevent boutonnière deformity, the triangular ligament bridging the two conjoined lateral bands must be preserved when cutting the extensor mechanism. – Unlike the other corrective procedures, active finger motion is permitted immediately after surgery.
- 72. Dorsal (A) and lateral (B) views of Fowler’s central slip tenotomy. The central slip is transected immediately proximal to its insertion on the base of the middle phalanx. The lateral bands and triangular ligament are preserved.
- 73. Management of Chronic Mallet Finger Injuries Surgical • DIP Joint Arthrodesis: – Indications: Salvage procedure for patients with painful mallet finger injuries secondary to arthritis, deformity, infection, and/or failed prior surgery. – Can be effectively performed with K-wires, tension band wiring, or IM screw fixation. – Position of fusion: between neutral and 10° of flexion. – Advantages of arthrodesis: • Reliable pain relief • Early PIP joint finger motion
- 74. Posteroanterior (A) and lateral (B) radiographs of a DIP joint arthrodesis. Fixation was achieved with a headless differential-pitch compression screw.
- 75. Complications • Complication rates: – In digits treated with extension splinting: 45% – In digits treated surgically: 53%.
- 76. Complications • Complications associated with splinting: – Most are transient. – Most resolve with adjustment of the splint or after completion of treatment. – Complications include: • Skin maceration and ulceration • Tape allergy • Transverse nail plate grooves • Splint-related pain
- 77. Complications • Complications associated with surgical treatment: – 76% are long-term complications. – Reported problems include: • Infection • Nail plate deformity • Joint incongruity • Hardware failure • DIP joint prominence • DIP joint deformity
- 78. Mallet Thumb • Unlike mallet finger, avulsion of the extensor pollicis longus (EPL) tendon at its distal insertion (mallet thumb) is rare. • Although the recommended treatment for closed mallet finger is conservative, some authors proposed operative treatment for mallet thumb.
- 79. References • Bendre AA, Hartigan BJ, Kalainov DM: Mallet Finger. J Am Acad Orthop Surg 2005;13:336- 344 • Dean BJF, Little C: Fractures of the metacarpals and phalanges. Orthopaedics & Trauma 2011; 25(1):43-56 • De Smet L, van Ransbeeck H: Mallet Thumb. Acta Orthopædica Belgica 2003; 69(1): 77-78 • Rust PA, Eckersley R: Twenty questions on tendon injuries in the hand. Current Orthopaedics (2008) 22, 17–24
Hinweis der Redaktion
- Lateral radiographs of the middle finger showing mallet fracture with dorsally displaced intra-articular fracture fragment from the base of the distal phalanx involving about 50 % of the articular surface without comminution and volar subluxation of the distal phalanx. Lateral radiograph demonstrating a bony mallet injury, note the extensor lag of the distal interphalangeal joint.
- A thermoplastic mallet splint (Stack)
- Lateral radiograph of a bony mallet injury treated with a mallet splint, this radiograph confirms a satisfactory reduction with a fully extended joint.
- Patel MR, Desai SS, Bassini-Lipson L: Conservative management of chronic mallet finger. J Hand Surg [Am] 1986; 11:570-573.
