Minerals all
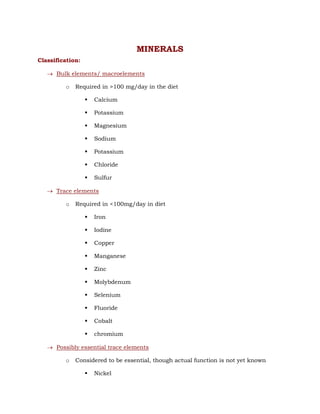
- 1. MINERALS Classification: Bulk elements/ macroelements o Required in >100 mg/day in the diet Calcium Potassium Magnesium Sodium Potassium Chloride Sulfur Trace elements o Required in <100mg/day in diet Iron Iodine Copper Manganese Zinc Molybdenum Selenium Fluoride Cobalt chromium Possibly essential trace elements o Considered to be essential, though actual function is not yet known Nickel
- 2. Tin bromine Lithium barium Unessential but found in diet Rubidium Silver Gold Bismuth Toxic minerals o Found in food but toxic Lead Aluminium Mercury Arsenic cadmium CALCIUM Sources: Milk and milk products Egg, fish and meat Vegetables, cereals, pulses, nuts Recommended dietary allowance (RDA): ADULT: 500 mg/day Children: 1200 mg/day Pregnant and lactating: 1500 mg/day Aged : 1500mg/day; vit D - 20µg/day to facilitate Calcium absorption
- 3. Functions: All functions are by the ionic form- Ca 2+ Constituent of bones and teeth o Present as calcium hydroxy apatite crystals o Provides strength and hardness o Storehouse of calcium (i.e., if serum calcium level decreases, it can be supplied by the bones) Blood coagulation o Factor IV o Activation of other clotting factors- VIII, IX, X and prothrombin. Enzyme action o Activates enzymes via calmodulin Eg: adenylate cyclase, phosphorylase kinase, pyruvate carboxylase, pyruvate dehydrogenase, glycogen synthase etc. Role in muscle contraction Role in nerve conduction Neuromuscular excitability o Decreases neuromuscular excitability o Counteracts the excitatory effects of Na+ and K+ o Decreases serum Ca2+ - spasms – hypocalcemic tetany In myocardium, it prolongs systole; if calcium level is very high, cardiac arrest is caused in systole. Release of stored hormones- insulin, PTH, calcitonin, ADH Second messenger in hormonal action o G proteins & inositol triphosphate Secreted in milk Absorption:
- 4. In first and second part of duodenum Active process- against concentration gradient Factors favouring absorption: Vit D- active form- calcitriol- i.e., 1, 25-dihydroxy cholecalciferol o Increases synthesis of carrier protein CALBINDIN o Action of Vit D is similar to that of steroid hormones; hence it itself is considered as a hormone. Parathormone (PTH) o Increases calcium absorption by activating Vit D through 1αhydroxylase Acidity if increased in intestine favours calcium absorption The amino acids lysine and arginine also favour absorption. Factors decreasing absorption: Phytates like inositol hexaphosphate Oxalates precipitate calcium as calcium oxalate Malabsorption syndromes The change in Ca : P ratio from the normal range of (2:1 to 1:2) decreases absorption Serum calcium: Normal : 9-11 mg/dL Torniquet should not be tied while testing Ca2+ levels as it will give wrong higher values. Calcium exists in three forms in serum o Ionic calcium (Ca2+) – 50% o Anions (phosphate/ citrate/ oxalate/ complexes) < 1 mg o Bound to albumin (protein bound calcium)- 4mg/dL o First two are called diffusible calcium Regulation:
- 5. 1. Effect of Vit D On intestine: increase synthesis of calbindin thus increasing calcium absorption On bone: calcification (deposition of calcium & phosphate in bone mineralisation) and also increase osteoblast activity thus decreasing serum calcium level On kidney: decreases excretion/ increases reabsorption of calcium thus increasing serum calcium levels. Overall : hypercalcemic effect 2. Effect of PTH On bone: causes resorption/ demineralisation by stimulating osteoclasts On kidney: increases reabsorption of calcium; excretion of phosphorus (phosphaturic effect) On intestine: increases absorption of calcium Overall: hypercalcemic effect 3. Effect of calcitonin Secreted by parafollicular cells of thyroid 32 amino acids On bone: deposition of calcium & phosphorus (mineralisation) On intestine: decreases absorption but not prominent On kidney: not much action, probably increases excretion of calcium Overall: hypocalcemic effect In medullary carcinoma of thyroid, calcitonin concentration increases; hence is used as tumour marker. 4. Phosphorus level inversely affects calcium level. i.e,. Ca × P = 40, a constant (higher in children) 5. Serum protein levels 1 g decrease in serum albumin leads to 0.8 mg decrease in serum calcium
- 6. 6. pH of plasma Alkalosis – makes ionic Ca bind with protein – ionic Ca decreases – causes tetany 7. In children, serum Ca level is closer to the upper limit 8. Renal threshold – 10 mg/dL Hypercalcemia: Effects: Deposition in kidneys along with phosphorus – tubular damage and renal calculi Deposition in extra osseous tissues Decrease in neuromuscular excitability characterised by constipation, abdominal pain, muscular hypotonia In heart if the level goes beyond 15 mg/dL, cardiac arrest is caused. Causes: Hyperparathyroidism Excess intake/ increased absorption of Vit D/ calcium/ both. Sarcoidosis – increased sensitivity to Vit D – increased Ca absorption Secondary malignancies (carcinoma) in bone Leukemias Paget’s disease Osteoporosis Thyrotoxicosis Drugs like thiazides (diuretic) Hypocalcemia: Effects: Tetany (only when IONIC calcium decreases) – tested using CHVOSTEK’S SIGN & TROUSSEAU SIGN
- 7. Usually asymptomatic Carpopedal spasm (affects hands, feet, face & larynx) Causes: Chronic renal failure Defecient intake/ dietary defeciency/ decreased absorption of Ca and Vit D Diseases of pancreas, biliary tract and intestine Hypoparathyroidism – acquired/ idiopathic Neonatal hypocalcemia due to maternal hyperparathyroidism Hypoproteinemia Acute pancreatitis Renal tubular defects PHOSPHORUS Sources: milk, meat, fish, eggs, vegetables RDA: 500 mg/day in adults; >1 g in children Absorption: in mid jejunum as inorganic phosphorus (mechanism not clearly understood) Factors affecting absorption: Ca : P ratio of 2:1 to 1:2 has best absorption Vit D increases phosphorus absorption PTH increases P absorption Calcitonin decreases P absorption Iron and phytic acid decrease absorption by binding with P and forming complexes Functions: Component of bones and teeth Totally, 1 kg of phosphorus is found in body,
- 8. o 80% in bones and teeth o 10% in muscles o 10% in cells As components of high energy compounds like ATP, GTP, CTP, carbamoyl phosphate, creatine phosphate, PEP etc. Intermediates in carbohydrate metabolism are phosphate derivatives. In lipid metabolism, o Intermediates of TAG synthesis are phosphate derivatives o As components of membranes (phospholipids) Phosphoproteins In the nucleotides and nucleic acids, backbone has phosphate In acid base balance, as phosphate buffer system Component of coenzymes like TPP, PLP, NAD+, NADP+, FMN, FAD, CoA etc. Regulation of enzyme activity by phosphorylation and dephosphorylation. eg., glycogen synthase and glycogen phosphorylase Serum phosphorus: Normal: 2.5 – 4.5 mg/dL in adults; 4 – 6 mg/dL in children To estimate serum P level, hemolysis of collected blood must be avoided. Regulation of serum P level: PTH In intestine: increases absorption In bone: bone resorption These increase serum P level In kidneys: phosphaturic effect This decreases serum P level, which is more pronounced. Therefore, overall effect if decrease in serum P level Calcitonin
- 9. In bone: decreases resorption In intestine: decreases absorption In kidneys: increases phosphaturia Overall effect is decrease in serum P level Calcitriol/ vit D In intestine: increases absorption In kidneys: increases reabsorption These increase serum P level In bones: increases mineralization This decreases serum P level. Overall effect is increase in serum P level. Hyperphosphatemia: no definite symptoms seen Causes: Excess Vit D Renal failure Hypoparathyroidism and pseudohypoparathyroidism Diabetic ketosis Healing fractures Acromegaly Hypophosphatemia: anorexia, bone pain, muscular weakness, dizziness Causes: Hyperparathyroidism Rickets and osteomalacia Hyperinsulinism Steatorrhea – decreases fat absorption – decreases Vit D absorption Fanconis syndrome
- 10. IRON Sources: green leafy vegetables, cereals, pulses, jaggery, fish, meat, liver. Milk is a very poor source. RDA: males: 20 mg, females: 30 mg, pregnant: 40 mg per day. Functions: totally, 3 to 5 g of iron is found in body. Part of proteins. They are of two types: o Heme proteins Hb, Mb Enzymes like cytochromes, tryptophan pyrrolase, catalase, peroxidase o Non heme iron proteins Fe-S centres Aconitase – activated by iron Ferritin Transferrin o 75% in Hb; 5% in Mb; 20% in other proteins. Absorption: only 10% of iron intake is absorbed from upper duodenum Factors affecting absorption: Gastric HCl liberates Fe3+ from food, favouring absorption G-SH, Vit C, ferrireductase, -SH of cysteine help to convert Fe3+ to Fe2+ Vit C and amino acids form soluble chelates (iron ascorbate and iron aminoacid) favouring absorption.
- 12. Transport: In blood, through transferrin Each transferrin has 2 binding sites for iron 300 mg of transferrin present in 100 mL of blood can bind with 400 μg of Fe3+ (range 250 to 400 μg) – Total Iron Binding Capacity (TIBC) But, only one third of the sites are used in normal individual. Therefore, total serum iron is 100 to 150 μg/dL In liver diseases, TIBC decreases In iron deficiency anemia, TIBC increases. Uptake of iron: By reticulocytes in bone marrow By receptor mediated process in reticulocyte membrane. Receptor + transferrin Receptor-transferrin complex Internalized Iron liberated Receptor-apotransferrin complex Goes back to its membrane site Receptor remains; apotransferrin returns to blood Storage : in ferritin Has 24 subunits
- 13. Can bind to 4000 atoms of Fe3+, but in normal, only 2000 Fe3+ are bound to one ferritin molecule. 20% of iron is in this form. Hemosiderin: Insoluble, amorphous form of iron 37% of iron is in this form Ferritin in centre, with aggregates of iron on it Formed only during iron overload. Excretion: 1 to 1.5 mg/day through faeces Unabsorbed iron and iron from the desquamated mucosal cells. Disorders: Iron deficiency anemia Most common nutritional deficiency disorder 30% of world’s population is anemic In India, it is 70%; in pregnants, 80% are anemic Microcytic, hypochromic type. Causes: Lack of nutrition o The food may not contain iron o Phytates and oxalates in food bind to iron and prevent its absorption Hookworm infection (one worm – 0.3 mL blood/day) Repeated pregnancies (1 g iron lost per pregnancy) Chronic blood loss o Haemorrhoids/piles o Peptic ulcers
- 14. o Menorrhagia Nephrosis o Loss of haptoglobin (binds Hb), haemopexin (binds heme) and transferrin Lead poisoning (it inhibits ALA dehydratase – decreased Hb synthesis) Lack of absorption after gastrectomy Hypoclorrhydria Clinical manifestations: Person becomes uninterested – apathetic – due to decreased O2 Decreased ATP synthesis as iron is a component of cytochromes Atrophy of gastric epithelium Dysphagia – Plummer Wilson syndrome – precancerous condition Impaired attention, irritability, poor memory – decreased scholastic performance Person becomes less efficient. Lab findings: Hb < 12 g/dL Serum iron < 100 μg/dL Increased TIBC Treatment: Treating the underlying cause than the symptoms. Iron and folic acid - 100 mg & 500 μg in pregnants; 20 mg & 100 μg in children Iron toxicity: Hemosiderosis: Golden brown granules of hemosiderin accumulate in liver and spleen Seen in patients receiving repeated blood transfusion as in thalassemia, hemophilia etc.
- 15. Hemochromatosis/Bronze diabetes: Total body iron > 30 g (normal 4 to 5 g) Hemosiderin in large quantity, in liver – liver cirrhosis; in pancreas – diabetes; in skin – brown appearance Bantu siderosis: Found in African Bantu tribe Due to cooking in iron vessels MAGNESIUM Sources: all green vegetables (chlorophyll has Mg) RDA: 350 mg/day Total body Mg content: 25 g Functions: 60% of body’s Mg is found in bones and teeth Cofactor for enzymes utilizing ATP, like kinases (PFK, alkaline phosphatase, hexokinase, cAMP dependent kinases. In body, Mg-ATP complex is found. Mg-ATP is substrate for adenylate cyclase to form cAMP Activation of myosin ATPase Nucleic acid and protein biosynthesis need Mg as cofactor – polymerases, aminoacyl tRNA synthetase Reduces neuromuscular excitability Mg deficiency – hypomagnesemic tetany Serum levels: 1.8 to 2.2 mg/dL
- 16. Hypomagnesemia: Causes: Severe, prolonged diarrhea Malabsorption Protein Calorie Malnutrition (PCM) Alcoholism and malnutrition Hypermagnesemia: CNS depression Lousiness, lethargia Causes: Increased use of Mg containing laxatives and antacids Renal failure COPPER RDA: 2 – 3 mg/day Total body copper content: 100 mg Serum concentration: 70 to 140 μg/dL Transport: bound to albumin Functions: Role in iron metabolism (component of ceroluplasmin/ferroxidase) Deficient ceruloplasmin – iron deficiency anemia – CANNOT be treated by oral iron therapy (normal blood concentration of ceruloplasmin (an acute phase protein) is 25 to 50 mg/dL Component of the enzyme superoxide dismutase. This enzyme is of two types: o Cytosolic – has 2 Zn2+ and 2 Cu2+ per molecule o Mitochondrial – has 2 Zn2+ and 2 Mn2+ per molecule For cross linking of collagen, enzyme lysyl oxidase has Cu.
- 17. Tyrosinase needs copper. Other enzymes requiring copper are cytochrome oxidase, tryptophan pyrrolase, dopamine β hydroxylase, monoamine oxidase, δ ALA synthase. Copper increases HDL concentration. Disorders: Wilson’s disease (hepato-lenticular degeneration): Decrease in plasma ceruloplasmin Due to defect in gene coding for Cu containing ATPase Liver cirrhosis due to Cu deposition In lentiform nucleus of brain, Cu is deposited, leading to Parkinson’s disease like symptoms Damage to kidney tubules – aminoaciduria Deposition in pancreas – diabetes Deposition in edges of cornea – in Descemet’s membrane, forming golden brown/blue/green ring (Kayser-Fleischer ring) Penicillamine – chelating agent Menke’s kinky/steely hair disease: Deficient Cu binding ATPase. ZINC RDA: 10 to 15 mg/day Total body zinc content: 2 to 3 g Functions: Component of enzymes o More than 300 enzymes need Zn2+ as cofactor. o Eg., superoxide dismutase, carbonic anhydrase, alcohol dehydrogenase, LDH, glutamate dehydrogenase, retinine reductase, RNA polymerase. Vit A metabolism
- 18. o Stimulates Vit A from liver o Increases plasma Vit A level and its utilization in Rhodopsin cycle Role in taste o Protein gusten in saliva needs Zn For growth and reproduction Role in insulin action o For storage and release of insulin Promotes wound healing, mechanism not known Defeciency manifestations: Loss of appetite, poor growth, dermatitis, impaired wound healing, decreased taste sensation (hypogeusia), loss of hair (alopesia), fetal malformations. Disorder: Acrodermatitis enteropathica Disorder of Zn absorption Characterized by acrodermatitis Skin lesion around mouth, teeth, fingers Diarrhea IODINE Source: commercial salt RDA: 150 to 200 μg/day Total body iodine content: 25 to 30 mg; 80% of it is in thyroid gland Function: component of thyroxin hormones – T3 and T4 Deficiency: Second major micronutrient deficiency in India (first place for iron, third place for Vit A) Goitre Goitrous belt – areas rich in goitre patients; along the Himalayas
- 19. Goitrogens o Present in food o Decrease iodine utilization o Present in cassava tubers, bamboo, sweet potato o Cabbage and tapioca have thiocyanate which inhibits iodine uptake by thyroid gland o Mustard seeds have thiourea inhibits iodination of tyrosine in thyroglobulin. FLUORINE Source: Drinking water is the main source Other sources are sea fish, tea, cheese, jowar, toothpaste RDA: 2 to 4 mg/day Functions: Present as fluoride ion. In places where water has fluoride >1 ppm (0.1 mg/dL), people are resistant to dental caries o Mode of action: fluoride gets incorporated to enamel of teeth and makes it resistant to organic acids of bacteria Makes bone resistant to osteoporosis Inhibits enolase, thus stops glycolysis. Fluorosis: Excess of fluoride (>3 to 5 ppm, also goes as high as 20 ppm) in drinking water Mottling of teeth Chalky appearance of teeth, brown pigmentation Pitting of teeth – pieces of teeth may be lost Alternate areas of osteosclerosis and osteoporosis.
- 20. MANGANESE Component of enzymes o Superoxide dismutase – mitochondrial component o Arginase o Isocitrate dehydrogenase o Cholinesterase o Enolase Many kinases, hydrolases, decarboxylases need Mn Activation of glycosyl transferases, to synthesize oligosaccharides, proteoglycans and glycoproteins In animals, for normal reproduction and bone formation. SELENIUM Functions: Component of glutathione peroxidase, hence acts as antioxidant It has sparing effect on Vit E and vice versa Part of 5-deiodinase needed to convert T4 to T3 Component of thioredoxin reductase Amino acid selenocysteine (SeCys/SeC) is the 21st amino acid o It has –SeH group instead of –SH group o It is incorporated into proteins; coded by stop codon UGA Deficiency: Liver necrosis and cirrhosis Cardiomyopathy, muscular dystrophy Keschan cardiomyopathy: Seen in Keschan province in China Soil contains less Se causing deficiency
- 21. Cardiac necrosis, arrhythmia MOLYBDENUM Component of molybdoflavo enzymes xanthine oxidase and aldehyde oxidase Also found in sulfite oxidase and nitrite reductase COBALT Component of cobalamin Stimulates formation of erythropoietin Activates glycyl glycine dipeptidase CHROMIUM Role in glucose metabolism – increases glucose tolerance of an individual.
