Ped.case hx
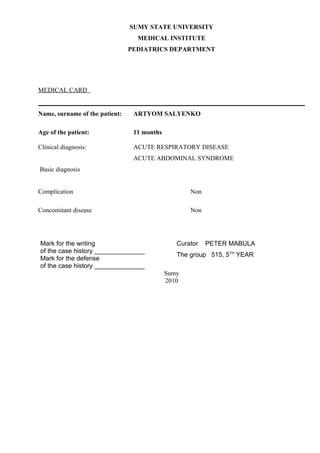
- 1. SUMY STATE UNIVERSITY MEDICAL INSTITUTE PEDIATRICS DEPARTMENT MEDICAL CARD Name, surname of the patient: ARTYOM SALYENKO Age of the patient: 11 months Clinical diagnosis: ACUTE RESPIRATORY DISEASE ACUTE ABDOMINAL SYNDROME Basic diagnosis Complication Non Concomitant disease Non Mark for the writing Curator PETER MABULA of the case history ______________ The group 515, 5TH YEAR Mark for the defense of the case history ______________ Sumy 2010
- 2. GENERAL PATIENT’S INFORMATION Name: ARTYOM Surname: SALYENKO Age: 11 Months Home address: TOKAL SUMY Date of admission to the hospital: 1 APRIL 2010 Pre-admission diagnosis: RESPIRATORY DISEASE, GIT SYNDROME ______________________________________________________________________ Patient’s department: INFECTIOUS (PEDIATRICS) I. COMPLAINTS Main: Fever, diarrhea and vomiting for 2 days. II. ANAMNESIS OF THE DISEASE The patient was apparently well until 2 days ago when he experienced an acute onset of fever which was shoerly followed by diarrhea and vomiting on the very day. His mother says he was previously given some food which she suspects to have caused the problem. The previous treatment: He has a history of the same disease atleast every 3 months of which 3 months ago he suffered the same problem where he was treated and apparently was cured. III. ANAMNESIS VITAE For children till 3 years The child was born from a health mother of which it was a SNVD at term and weighed 3.030kg. During pregnancay there were no pregnancy associated complications though was born at home and later was brought to the hospital for check up. Apgar’s score was not immediately checked since it was a home delivery. The child is breast fed and has received all necessary vaccinations. Dynamics of head circumference: 46.5cm Dynamics of chest circumference: 47.5cm The psychomotor development of the child: normal and satisfactory For all children irrespective of age The child had the same disease 3 months ago and it has been recurrent. Housing conditions of the child is satisfactory. Character of nutrition before present disease (character of meal, schedule of feeding) Normal and balanced diet. Allergological history
- 3. Presence of allergy symptoms: NO The intolerance of products: NO The intolerance of medicament (drug): NO No genetic illnesses No allergic reactions Epidemiological history The child didn’t contact with patients who suffered with inflectional diseases last 3 weeks. The symptoms of diarrhea were just 3 times a day and vomited once during last three days. Genetical history To make the pedigree of the patient, using common symbols: Healthy woman Healthy man Proband Sex unknown Dead Abortion Medical abortion Still-birth Marriage Consanguineous marriage Repeated marriage Unmarriage Sibling Monozygotic twins Dizygotic twins
- 4. No known pregnancy Sterility Known heterozygous person Carrier female Pregnancy in progress Affected person Objective examination of the child The patient’s general condition is moderately ill but satisfactorily responding to medication, The state of consciousness is clear, The mental state is (not) adequate Position of the child in bed is active, The patient is asthenic constitution. The child is of regular. Anthropometrical measurements Criterion In patient Weight, kg 9.5kg Height (stature), cm 75cm Head 46.5cm circumference, cm Chest circumference, cm 47.5cm The index by Erisman 10cm Summary: The child’s anthropometric measures are within normal ranges.
- 5. The skin and mucous membranes Colour of a skin - pink lip-nose triangle normal and no cyanoses. No skin rashes. Surface of a skin is smooth. The elasticity of the skin is kept within normal. Temperature of a skin is a bit febrile. Sensitivity of the skin: temperature 38celsius, Mucous membranes of a mouth reveals moist and smooth. Gums: pink in colour and moist Conjunctiva and sclera of eyes are a bit moist but no redness or discharge. The subcutaneous fat is distributed evenly. The skin fold thickness is 2 cm on abdomen, 1.5cm under the scapula, 1.5 cm on the shoulder, 2 cm on thigh. No oedema. The skin turgor is kept. Lymphatic system No palpable lymph nodes. The tonsils. Not inflammed. Muscular system The development of muscles is satisfactory, well-developed and symmetrical. Muscular tone within normal ranges. The range of motions is fully and no limitations The strength of muscles moderately strong. No pain during palpation of the muscles. Bone system Head circumference is 46.5сm, (normal) The head is mesocephalic. Anterior fontanel (presence,normal size and diamond shape, slight pulsation. Posterior fontanel fused Cardiovascular system Inspection: During inspection of the chest no bulging, no visible pulsation seen, no cyanosis, no odema, no jaundice. Palpation: The apical or cardiac trust (beat) is located on 5th intercostal space midclavicular line, No systolic or diastolic vibratory thrills palpable. Pulse (rate) is 134 beats per minute; rhythmic, synchronic, full but swift, Blood pressure of upper extremities 85/53 mm Hg. Border’s of hearts relative dullness
- 6. Border In patient Normal Right Right parasternal line Corresponding with the patients Upper 2nd rib parameters Left 2cm outer of left mid-clavicular line transversa 8cm 6-9cm l size Border’s of hearts absolute dullness Border In patient Normal Right Left sterna line Corresponding to patients parameters Upper 2nd intercostals space Left Mid-clavicular line (outer) transversa 2-3cm l size Auscultation: the heart sounds strong, rhythmical, 134 beats per min. S 1 is heard loudest at the apex of the heart, S2 is heard loudest at the right 2nd intercostal parasternal.no accent. No murmurs. Respiratory system No cyanosis of nasolabial triangle, per oral region, nails plates, acrocyanosis. Nasal breathing is free. Voice is normal. No cough present. No dyspnoea, Chest has normosthenic,. The intercostals spaces are normal. Movements of the chest - symmetrical, Type of breathing is combined (thoracic, abdominal). Dyspnea is absent. The respiration rate is 34 per minute (normal, tachypnea, bradypnea). The breathing is regular, Palpation: no pain on maxillary and frontal sinuses. Vocal fremitus is normal, No Pleural friction rubs or crepitations. In comparative percussion of the chest no abnormal or variational sounds heard. The width of Crenig’s areas 4cm Auscultation of the lungs: the breathing is vesicular and no presence of rales, rhonchi or crepitations. Digestive system Inspection: The colour of mucous membranes of oral cavity is moist, no incrustation (coating), no fissure or aphtha, colour of the tongue is pink, no inflammation of tonsils.
- 7. In vertical position the abdomen has normal shape, not distended, symmetrical abdominal circumference and moves with breathing, no visible peristalsis, the umbilicus is centrally located, is flatten. Also in horizontal position the abdomen has normal shape, moves with breathing, no distended veins of the anterior abdominal wall “caput Medusa”. In superficial palpation there is soft, the no present of tumour. Blumberg’ sign is negative; painless, McBurney’s point. Deep palpation according to Obraztsov-Strazhesko Sigmoid colon is localized in LIF, cylindrical in shape with soft consistance and mobile. Caecum is localized in RIF cylindrical shape, painfulness, movable, Colon transverses is localized in epigastric region with cylindrical shape, Colon ascenders: is localized in right part of the abdomen, cylindrical and normal consistance all painfulness. Colon descendent is localized in the left side of the abdomen with cyllindrical shape, soft and mobile. The liver not palpable, not tender,). Ortner’s symptom is negative, Ker’s symptom is negative, Murphy’s symptom is negative, Mussi-Georgievsky’s symptom is negative. The spleen not palpable, not tender. Meyo-Robson’s symptom is negative. The pancreas not palpable In auscultation intestinal peristalsis is not impaired. Stool is 3 times per day- liquid, without an admixing. Urinary system Inspection: No oedema on legs, face, sacral part, or on the lower part of abdomen. The No change of odour of urine though is said to be a bit concentrated. Examination of sacral area, lower abdominal part. No change of color of the skin no edema. Examination of the external sex organs: stage of development - no abnomarmality. symmetric development of the scrotum Testis present in the scrotum; no inflammation of penis or anomalies of penis development, phimosis, paraphimosis. Kidneys not palpable in vertical or horizontal position. Pasternatsky’s symptom is negative on right and on left side. Urinary frequency 3 times a day, Daily urine flow 60ml per urination, proportion between day and night diuresis2:1 Presence of uncontrolled urinations - no Endocrine system Examination: face expression - normal, no changes of anterior cervical surface. The level of development subcutaneous fat is within normal parameters. Thyroid gland not palpable. Nervous system The consciousness is kept. The mental development corresponds to the age of child.).
- 8. Nn nystagmus. Pupils are equal in size; no mydriasis or miosis. The light reflex is retained. The coordination of movement is kept. The pain sensitivity is kept. Tactile sensitivity is kept. Newborn reflexes (the necessary underline): Sucking - is normal, hypoactive, hyperactive; Rooting - is normal, hypoactive, hyperactive; Defence - is normal, hypoactive, hyperactive; Lip or trunk reflex - is normal, hypoactive, hyperactive; Grasp - is normal, hypoactive, hyperactive; Babinski's - is normal, hypoactive, hyperactive; Moro - is normal, hypoactive, hyperactive; Supporting - is normal, hypoactive, hyperactive; Dance or step - is normal, hypoactive, hyperactive; Perez - is normal, hypoactive, hyperactive; Crawling - is normal, hypoactive, hyperactive; Bauer's - is normal, hypoactive, hyperactive; Galant - is normal, hypoactive, hyperactive. Upper Brudzinski’s reflex - is normal, hypoactive, hyperactive; middle Brudzinski’s reflex - is normal, hypoactive, hyperactive; low Brudzinski’s reflex - is normal, hypoactive, hyperactive. Tendon reflexes brisk, (equally marked on both sides, Psycho-motor development of the child Gross motor development: Normal motor development Fine motor development: Normal Motor functions Sensory development : Normal sensory reflexes Vocalization development:Normal Socialization development: Child has no mental problems The plan of examination of the patient 1) History 2) Physical examination 3) Lab tests 4) Results of additional methods of examination Rooting blood analysis date Нb Eryth. CI Leuc Eos Bas juv. ban seg. lym mon ESR Blood clotting time х1012 х109 d 1.4 117 3.7 o.9 5.1 2 3 21 72 1 3 Urinal examination according to Nechepurenco NOT DONE Biochemical analysis of blood date protein glucose Bilirubin Creatinin urea ALT AST Amylase e
- 9. total total conjugated Urinal examination according to Zymnitzky: NOT DONE Portion 1 2 3 4 5 6 7 8 Quantities of urine specific gravity Analysis of feces on worm ova: Not done Test on enterobiosis: Not done Other methods of examination: Non Systemic examination done accordingly to discover or exclude other pathologies Clinical diagnosis:ACUTE RESPITORY DISEASE Basic diagnosis:Awaiting Lab results Complication: NON Concomitant disease:ACUTE ABDOMINAL SYNDROME Differential Diagnosis: 1) Enteral viral infection 2) Food poisoning (mild) 3) Acute Respiratory viral infection with secondary bacterial superinfection 4) The temperature list Data B P T M E M E M E M E M E M E M E M E M E M E M E M E M E M E P Epicrisis The patient: Artyom Salyenko Age,11months, Home address: Tokali Sumy Undergoing treatment at Sumy pediatrics Hospital from April 1, 2010 with a preliminary diagnosis of Acute Respiratory Disease and GIT Syndrome The general state and data of objective examination of the patient on admission (shortly)
- 10. The patient was admitted with c/o acute respiratory disease accompanied with diarrhea and vomiting plus high fever up to 38 celsius. The child is adynamic and weak. Has not been breastfeeding and eating since the beginning of the disease. Diarrhea 2 times and vomiting once a day. Prescribed treatment: 1) ORT 150ml/kg/1st 6hours then the same amount/day 2) Amoxycillin 100mg/kg qid for 7-10 days 3) Paracetamol 10mg/kg tid 3/7 4) Vitamins supprementations Recommendations: 1. Normal diet 2. Regimen : Bed rest Literature: Nelson text book of Pediatrics Case Hx by: Peter Mabula 5th Year Group 515