Haemolytic anaemia
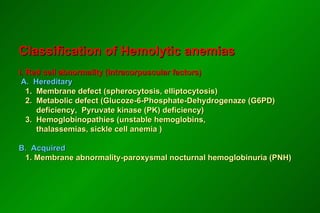
- 1. Classification of Hemolytic anemias I. Red cell abnormality (Intracorpuscular factors) A. Hereditary 1. Membrane defect (spherocytosis, elliptocytosis) 2. Metabolic defect (Glucoze-6-Phosphate-Dehydrogenaze (G6PD) deficiency, Pyruvate kinase (PK) deficiency) 3. Hemoglobinopathies (unstable hemoglobins, thalassemias, sickle cell anemia ) B. Acquired 1. Membrane abnormality-paroxysmal nocturnal hemoglobinuria (PNH)
- 2. HEMOLYTIC ANEMIAS Hemolytic anemias = reduced red-cell life span
- 3. II. Extracorpuscular factors A. Immune hemolytic anemias 1. Autoimmune hemolytic anemia - caused by warm-reactive antibodies - caused by cold-reactive antibodies 2. Transfusion of incompatible blood B. Nonimmune hemolytic anemias 1. Chemicals 2. Bacterial infections, parasitic infections (malaria), venons 3. Hemolysis due to physical trauma - hemolytic - uremic syndrome (HUS) - thrombotic thrombocytopenic purpura (TTP) - prosthetic heart valves 4. Hypersplenism
- 4. Mechanisms of hemolysis: - intravascular - extravascular
- 5. Inravascular hemolysis (1): - red cells destruction occurs in vascular space - clinical states associated with Intravascular hemolysis: acute hemolytic transfusion reactions severe and extensive burns paroxysmal nocturnal hemoglobinuria severe microangiopathic hemolysis physical trauma bacterial infections and parasitic infections (sepsis)
- 6. Inravascular hemolysis (2): - laboratory signs of intravascular hemolysis : indirect hyperbilirubinemia erythroid hyperplasia hemoglobinemia methemoalbuminemia hemoglobinuria absence or reduced of free serum haptoglobin hemosiderynuria
- 7. Extravascular hemolysis : - red cells destruction occurs in reticuloendothelial system - clinical states associated with extravascular hemolysis : autoimmune hemolysis delayed hemolytic transfusion reactions hemoglobinopathies hereditary spherocytosis hypersplenism hemolysis with liver disease - laboratory signs of extravascular hemolysis: indirect hyperbilirubinemia increased excretion of bilirubin by bile erythroid hyperplasia hemosiderosis
- 8. Hemolytic anemia - clinical features: - pallor - jaundice - splenomegaly
- 9. Laboratory features: 1. Laboratory features - normocytic/macrocytic, hyperchromic anemia - reticulocytosis - increased serum iron - antiglobulin Coombs’ test is positive 2. Blood smear - anisopoikilocytosis, spherocytes - erythroblasts - schistocytes 3. Bone marrow smear - erythroid hyperplasia
- 10. Diagnosis of hemolytic syndrome: 1. Anemia 2. Reticulocytosis 3. Indirect hyperbilirubinemia
- 11. Autoimmune hemolytic anemia caused by warm-reactive antibodies: I. Primary II. Secondary 1. acute - viral infections - drugs ( -Methyldopa, Penicillin, Quinine, Quinidine) 2. chronic - rheumatoid arthritis, systemic lupus erythematosus - lymphoproliferative disorders (chronic lymphocytic leukemia, lymphomas, Waldenstr Ö m’s macroglobulinemia) - miscellaneous (thyroid disease, malignancy )
- 12. Autoimmune hemolytic anemia caused by cold-reactive antibodies: I. Primary cold agglutinin disease II. Secondary hemolysis: - mycoplasma infections - viral infections - lymphoproliferative disorders III. Paroxysmal cold hemoglobinuria
- 13. Autoimmune hemolytic anemia - diagnosis - positive Coombs’ test Treatment: - steroids - splenectomy - immunosupressive agents - transfusion
- 14. Hereditary microspherocytosis 1. Pathophysiology - red cell membrane protein defects (spectrin deficiency) resulting cytoskeleton instability 2. Familly history 3. Clinical features - splenomegaly 4. Laboratory features - hemolytic anemia - blood smear-microspherocytes - abnormal osmotic fragility test - positive autohemolysis test - prevention of increased autohemolysis by including glucose in incubation medium 5. Treatment - splenectomy
- 15. Paroxysmal nocturnal hemoglobinuria 1. Pathogenesis - an acquired clonal disease, arising from a somatic mutation in a single abnormal stem cell - glycosyl-phosphatidyl- inositol (GPI) anchor abnormality - deficiency of the GPI anchored membrane proteins (decay-accelerating factor =CD55 and a membrane inhibitor of reactive lysis =CD59) - red cells are more sensitive to the lytic effect of complement - intravascular hemolysis 2. Symptoms - passage of dark brown urine in the morning
- 16. 3. PNH –laboratory features: - pancytopenia - chronic urinary iron loss - serum iron concentration decreased - hemoglobinuria - hemosiderinuria - positive Ham’s test (acid hemolysis test) - positive sugar-water test - specific immunophenotype of erytrocytes (CD59, CD55) 4. Treatment : - washed RBC transfusion - iron therapy - allogenic bone marrow transplantation
- 17. SICKLE CELL ANEMIA Definition: chronic hemolytic anemia occuring almost exclusively in blacks and characterized by sickle-shaped red cells(RBCs) caused by homozygous inheritance of Hemoglobin S