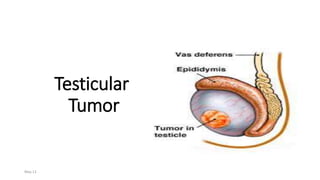
Testicular tumor
- 2. ANATOMY 2 Anatomy of the testis
- 3. Skin DARTOS Muscle External Spermatic Fascia Cremastric Muscle Internal Spermatic Fascia Tunica Vaginalis Tunica Albuginea Coverings of testis
- 4. Structure of testis • 200-300 lobules • Each lobule has 2-3 seminiferous tubules • Each seminiferous tubules lined by cell in different stages of spermatogenesis • Among the seminiferous tubules are Sertoli cells. • Between the loops of the seminiferous tubules are interstitial cells, produce testosterone.
- 5. BLOOD SUPPLY VENOUS DRAINAGE 5 Fig 6. Blood supply of testis
- 6. Lymphatic Drainage Drain into the retroperitoneal lymph glands between the levels of T11 and L4, but they are concentrated at the level of the L1 and L3 vertebrae
- 7. Testicular Tumor INTRODUCTION Testicular cancer forms about 1 -1.5% of all malignancies in males Incidence – 0.6 per 100000 Mortality – 0.3 per 100000 Cure rate increased with introduction of platinum based chemotherapy from 10 to 80%
- 8. EPIDEMOLOGY OF TESTICULAR CANCER • Age: for GCT: median age at diagnosis is 34 years. • Age - 3 peaks 2 – 4 yrs 20 – 40 yrs above 50 yrs In a man age: 50 years or older solid testicular mass is usually lymphoma • Race: more common in young white men ,less in African .
- 9. Testicular Descent December 16 9Recent advances in the management of Testicular tumor
- 10. Predisposing Factors 1. Cryptorchidism 2. Klinefelter syndrome 3. Positive family history 4. Contralateral germ cell tumor 5. Trauma 6. Viral infection 7. Hormonal factors 8. Exposure to environmental oestrogen
- 11. Predisposing Factors 1. Cryptorchidism • This risk is further increased if the testis is intra-abdominal. • Abdominal testis is more likely to be seminoma, testis brought to scrotum by orchiopexy is more likely to be NSGCT. • There is still an increased risk of developing a tumour in the contralateral normally descended testicle in pt. with cryptorchidism • Prepubertal orchidopexy fails to prevent the subsequent development of malignancy
- 12. KLINEFELTER SYNDROME • Characterised by: • testicular atrophy • absence of spermatogenesis • gynecomastia Karyotype: 47XXY
- 13. Pathological classification 2:Interstitial cell tumor of Testis 2-3% Leydig cell tumor Sertoli cell tumor 1:GERM CELL TUMORS 95% Seminoma 40% Non seminomatous germ-cell tumors 60% Embryonal carcinoma 20-25% Teratoma 25-35% Yolk sac (endodermal sinus) tumor Choriocarcinoma 1% Mixed germ-cell tumor 4: others 5% lymphoma
- 14. Seminoma The commonest variety of testicular tumour Adults are the usual target (4th and 5th decade); never seen in infancy Starts in the mediastinum: compresses the surrounding structure. Patients present with painless testicular mass 30 % have metastases at presentation, but only 3% have symptoms related to metastases
- 15. Seminoma • Serum alpha fetoprotein is normal • Beta HCG is elevated in 30% of patients with Seminoma • Classification a) classical b) Anaplastic c) Spermatocytic
- 16. Gross appearance of seminoma. The tumor in A is very small, whereas that in B has replaced most of the testis
- 17. Embryonal Carcinoma 2nd most common germ cell tumor 90% of NSGCT Most men present in their 20s to 30s with a testicular mass Highly malignant tumours; may invade the cord stuctures.epidydymis High degree of metastasis Serum AFP is positive in 33%, & beta HCG is elevated in 20% of cases
- 18. EMBRYONAL CARCINOMA • MACROSCOPIC : 1. Fleshy gray white tumor with prominent necrosis & hemorrhage
- 19. Yolk Sac Tumour Most common germ cell tumor ( & most common testicular tumor ) in children, • 60% of GCT in children. First 2 years of life. • #<2% of testicular tumors in adults • Elevated serum levels of alpha-fetoprotein. • Microscopically, Schiller-Duval bodies are a characteristic feature Testicular mass the most usual presentation.
- 20. YOLK SAC TUMOR • MACROSCOPIC : white to tan masses, with myxoid & cystic changes
- 21. pediatric yolk sac tumor appears as a solid, yellow, myxoid nodule
- 22. The cut surface of this adult yolk sac tumor shows areas of hemorrhage and cystic change.
- 23. Choriocarcinoma A rare and aggressive tumour (5yrs survival is 5%) Typically elevated hCG Primary is very small and often exhibit NO TESTICULAR ENLARGEMENT Small palpable nodule may be present Presents with disseminated disease. Prone to hemorrhage.
- 24. Choriocarcinoma
- 25. Teratoma Teratoma in greek means “monster tumor” Contain all three germ layers with varying degree of diffrentiation Occurs in its pure form in pediatric age group. In adults, occur as a component of mixed germ cell tumor. Normal serum marker ◦ Mildly elevated AFP levels
- 26. Interstitial cell tumors 1. Leydig cell tumors Presents with painless testicular mass A masculinising tumor, produces androgens Precocious puberty Prominent external genitalia Deep masculinised voice Pubic hair Gynacomastia and decreased libodo due to oestrogen production by increased peripheral conversion
- 27. LEYDIG CELL TUMOR • MACROSCOPIC : 1. Leydig cells impart a golden brown colour. tumor is solid & lobulated 2. Necrosis can be seen in malignant tumors
- 28. Interstitial cell tumors 2. Sertoli Cell Tumor can occur in any age group including infants It is a faminising tumor Excess estrogen production Gynacomastia in 1/3rd of cases 10 % are malignant
- 29. Interstitial cell tumors 3. Gonadoblastoma Mixed germ cell. Composed of seminoma like germ cells and Sertoli cells. Exclusively in patients with dysgenic gonads and intersex syndromes 80% are phenotype females with primary amenorrhoea 20% are males with crytochordism and dysgenic gonads and hypospadias Bilateral orchidectomy because of risk of bilateral tumours.
- 30. LYMPHOMA • CLINICAL : 1. Lymphoma most often result of secondary spread; occasionally , primary lymphoma may occur 2. Most men are in their 60s 3. Involvement is bilateral in 20 % of all cases
- 31. LYMPHOMA MACROSCOPIC : white to tan fleshy tumor
- 32. Spread 1. Direct spread 2. Lymphatic spread They drain primarily to para-aortic lymph nodes No inguinal nodes until scrotal skin involvement Seminoma metastasize exclusively through lymphatics 3. Blood Spread NSGCT spread through blood route Lungs, liver, bones and brain are the usual sites usually involved
- 33. CLINICAL FEATURES Painless Swelling of Testes Dull Ache or Heaviness in Lower Abdomen 10% - Acute Scrotal Pain 10% - Present with Metatstasis • - Neck Mass / Cough / Anorexia / Vomiting / Back Ache/ Lower limb swelling 5% - Gynecomastia Rarely - Infertility December 16 33Recent advances in the management of Testicular tumor
- 34. Clinical Features 2. Due to metastasis Abdominal or lumbar pain (lymphatic spread) Dyspnoea, hemoptysis and chest pain with lung mets Jaundice with liver mets Hydronephrosis by para-aortic lymph nodes enlargement Pedal oedema by IVC obstruction
- 35. Clinical Features 3. Clinical examination: a) Enlarged testis (except choriocarcinoma) b) Nodular testis c) Firm to hard in consistency d) Loss of testicular sensation e) Secondary hydrocele
- 36. INVESTIGATIONS 1. Scrotal Ultrasound 2. CT Scan Abdomen & Pelvis 3. CT Thorax / Chest X-Ray - PA and lateral views 4. Tumour Markers - AFP - HCG 5. MRI/PET Scan December 16 36Recent advances in the management of Testicular tumor
- 37. Human Chorionic Gonadotropin NORMAL VALUE: < 1 ng / ml HALF LIFE of HCG: 24 to 36 hours RAISED HCG - 100 % - Choriocarcinoma 60% - Embryonal carcinoma 55% - Teratocarcinoma 25% - Yolk Cell Tumour 7% - Seminomas normal value: below 16 ngm / ml half life of AFP – 5 and 7 days Raised AFP : Pure embryonal carcinoma Teratocarcinoma Yolk sac Tumor Combined tumors, AFP not raised in pure choriocarcinoma & in pure seminoma AFP –Alfa feto protein
- 38. ROLE OF TUMOUR MARKERS • Helps in Diagnosis - 80 to 85% of Testicular Tumors have Positive Markers • Most of Non-Seminomas have raised markers. • Degree of Marker Elevation Appears to be Directly Proportional to Tumor Burden • Normalization of tumor marker after high inguinal orchidectomy does not ensure complete disease removal however after Orchidectomy if Markers Elevated means Residual Disease • Negative Tumor Markers becoming positive on follow up usually indicates - Recurrence of Tumor • Markers become Positive earlier than radiological studies
- 39. T3
- 41. SURGICAL TREATMENT Scrotal Exploration and orchidectomy for suspected testicular tumor • Radical orchiectomy • Diagnostic and Therapeutic treatment of choice. • Complete removal of ipsilateral epididymis and spermatic cord to the level of the internal inguinal ring. • Partial orchiectomy • Considered in patient with polar tumor measuring 2 cm or less. • Adjuvant radiotherapy is given postoperatively. 41
- 42. CHEMOTHERAPY • Indications • As an alternative to adjuvant RT for stages I–II seminoma • Adjuvant therapy for stages II–IV seminoma • Regimens • Regimens including BEP, EP, PVB, and VIP for stages II–IV diseases Drug/ combination Dose and schedule Bleomycin 30 IU IV bolus on days 2,9,16 Etoposide 100 mg/m2 IV over 30 mins on days 1-5 Cisplatin 20 mg/m2 IV over 15-30 mins on days 1-5 Repeat cycle every 21 days for 3 or 4 cycles December 16 42Recent advances in the management of Testicular tumor
- 43. RETROPERITONEAL LYMPH NODE DISSECTION • The rationale for primary RPLND is that, in contrast to most malignancies, testicular GCT is surgically curable in most patients with low volume regional metastases. 43
- 44. Fig. 8 Laparoscopic RPLND Port Placement December 16 44Recent advances in the management of Testicular tumor
- 45. Fig. 9 Robotic assisted RPLND Port Placement December 16 45Recent advances in the management of Testicular tumor
- 46. RADIATION THERAPY • Seminoma is extremely radiosensitive. Radiation therapy is often used for adjuvant therapy for early-stage seminoma, and its use in non-seminoma germ cell tumors (GCT) is limited. December 16 46Recent advances in the management of Testicular tumor
- 47. • Fig. 10 Paraaortic and ipsilateral inguinal field for stage II left testicular seminoms, with inclusion of the renal hilus. December 16 47Recent advances in the management of Testicular tumor
- 48. Thank you
Hinweis der Redaktion
- 1. Changes start to develop at the age of 2 yrs
- Embryonal carcinoma showing solid nodular cut surface with numerous areas of necrosis and hemorrhage.
- Gross appearance of pure choriocarcinoma. The strikingly hemorrhagic appearance is characteristic of this tumor type.
- Gross appearance of Leydig cell tumor. A, The tumor, which has replaced most of the testis, has a granular yellowish appearance.
- Gross appearance of malignant lymphoma of large cell type, which completely replaces the testis.
