Carbon monoxide poisoning by dr Yasser Diab
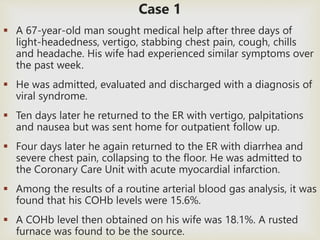
- 1. Case 1 A 67-year-old man sought medical help after three days of light-headedness, vertigo, stabbing chest pain, cough, chills and headache. His wife had experienced similar symptoms over the past week. He was admitted, evaluated and discharged with a diagnosis of viral syndrome. Ten days later he returned to the ER with vertigo, palpitations and nausea but was sent home for outpatient follow up. Four days later he again returned to the ER with diarrhea and severe chest pain, collapsing to the floor. He was admitted to the Coronary Care Unit with acute myocardial infarction. Among the results of a routine arterial blood gas analysis, it was found that his COHb levels were 15.6%. A COHb level then obtained on his wife was 18.1%. A rusted furnace was found to be the source.
- 2. Case 2 A 69-year-old man came to the ER after days of confusion, nausea, vomiting, intermittent syncope, hallucinations and shortness of breath. An arterial blood gas measurement found an oxygen saturation of 89%. He was admitted to the coronary care unit with a diagnosis of acute myocardial infarction. The next day a COHb level was measured and normal. While the patient was hospitalized he invited his sister and daughter-in- law to stay in his home. They both arrived at the ER the next morning with headaches, vomiting, and vertigo. Their COHb levels on initial observation were 28% and 32%. After investigation, the man’s gas water heater was faulty.
- 4. What Is Carbon Monoxide? Carbon monoxide is a colorless, odorless, tasteless, and initially non-irritating toxic gas, it is very difficult to be to detected. Carbon monoxide consists of one carbon atom and one oxygen atom, connected by a triple bond that consists of two covalent bonds as well as one dative covalent bond. Carbon monoxide is a product of incomplete combustion of organic matter due to insufficient oxygen supply to enable complete oxidation of carbon atom to form carbon dioxide (CO2).
- 6. Sources of carbon monoxide Endogenous a. Normal heme catabolism by heme oxygenase. b. Increased in hemolytic anemia, sepsis. Exogenous a. Incomplete combustion of carbonaceous fossil fuel b. House fires c. Automobile exhaust d. Propane-powered vehicles (forklifts, ice skating rink resurfacers) e. Gas-powered furnaces, ovens, fireplaces f. Heaters g. Indoor grills h. Camp stoves i. Boat exhaust j. Cigarette smoke k. Methylene chloride: a Solvent found primarily in paint remover Endogenously converted to carbon monoxide after inhalational exposure
- 7. Worldwide, the largest source of carbon monoxide is natural in origin, due to photochemical reactions in the troposphere that generate about 5×1012 kilograms per year.(Weinstock 1972) Other natural sources of CO include volcanoes, forest fires, and other forms of combustion.
- 8. Half-life: it is the time required for half the quantity of a drug or other substance to be metabolized or eliminated. CO half-life on 21% room air O2: 4-6 hours. CO half-life on 100% O2:80 minutes. CO half-life with hyperbaric O2: 22 minutes.
- 10. Who Is at Risk? EVERYONE, especially: People using alternate heat sources during power outages Elderly. Unborn babies, infants. People living in poorly vented crowded houses.
- 11. People with chronic heart disease, anemia, or respiratory problems. Personnel at fire scenes (fire-fighters/rescue workers) Individuals involved into camping activities (Kuwait and Gulf region). Industrial workers at pulp mills, steel foundries and plants producing formaldehyde and coke.
- 12. Incidence increase generaly in winter because: Insufficient ventilation Generators used inside during a power outage Gas or kerosene heater in room without proper ventilation Stoves or fireplaces that are improperly vented. Cars or trucks idling in a garage Improper use Using charcoal grills indoors Heating homes with gas ovens
- 13. Why carbon monoxide CO binds to: Hemoglobin Myoglobin Cytochrome oxidase Brain lipids is dangerous?
- 14. Hemoglobin: The affinity between hemoglobin and carbon monoxide is approximately 230 times stronger than the affinity between hemoglobin and oxygen so hemoglobin binds to carbon monoxide in preference to oxygen. Hemoglobin is a tetramer with four oxygen binding sites. The binding of carbon monoxide at one of these sites increases the oxygen affinity of the remaining three sites, which causes the hemoglobin molecule to retain oxygen that would otherwise be delivered to the tissue. This situation is described as carbon monoxide shifting the oxygen dissociation curve to the left.
- 16. Because of the increased affinity between hemoglobin and oxygen during carbon monoxide poisoning, little oxygen will actually be released in the tissues. This causes hypoxic tissue injury resulting in relative functional anemia. This decreases the amount of oxygen carried by the hemoglobin, and forming carboxyhemoglobin (COHb).
- 17.
- 18.
- 19. Cardiac myoglobin: Carbon monoxide also binds to the cardiac myoglobin. It has a high affinity for myoglobin, about 60 times greater than that of oxygen. Carbon monoxide bound to myoglobin may impair its ability to utilize oxygen.This causes reduced cardiac output and hypotension, which may result in brain ischemia. Carbon monoxide has double effect on the heart, hypoxia and direct toxicity.
- 20. Cytochrome oxidase: Carbon monoxide binds to mitochondrial cytochrome oxidase C and P450 with less affinity than oxygen, so it is possible that it requires significant intracellular hypoxia before binding. This binding interferes with aerobic metabolism and efficient adenosine triphosphate (ATP) synthesis. Cells respond by switching to anaerobic metabolism, causing anoxia, lactic acidosis, and eventual cell death. The rate of dissociation between carbon monoxide and cytochrome oxidase is slow, causing a relatively prolonged impairment of oxidative metabolism.
- 21. Brain lipid peroxidation: CO may cause leukocyte-mediated inflammatory changes in the brain, a process that may be inhibited by hyperbaric oxygen therapy. Following severe intoxication, patients may display central nervous system (CNS) pathology, including white matter demyelination. This leads to edema and focal areas of necrosis
- 22. Clinical picture Signs and symptoms usually vague and non-specific. You must ALWAYS maintain a high index of suspicion for CO poisoning!
- 23. Acute exposure Chronic exposure Delayed effect Headache: dull, frontal, and continuous (most common) (Hampson et al 2002) General: Malaise, flu-like symptoms, fatigue. Central: Drowsiness, weakness, agitation, confusion, Visual disturbance, syncope, seizures, Fecal and urinary incontinence, Memory and gait disturbances, coma Circulatory: Dyspnea on exertion, Chest pain, palpitations. Other: Nausea , vomiting , diarrhea, Abdominal pain Headache, dizziness, anorexia, apathy, insomnia, and personality disturbance Polycythemia and cardiomegaly, likely secondary to chronic hypoxia (Penney 1988) DNS or delayed neurological sequalae in the form of impairment of cognitive functions. Clinical picture of CO poisoning:
- 24. Giuseppe et al 2011
- 25. Clinical severity:(Ernst et al 2008) Mild < 15 - 20% Headache Nausea, Vomiting Dizziness, Blurred vision Moderate 21 - 40% Confusion, Syncope Chest pain, Dyspnea Weakness Tachycardia, Tachypnea Rhabdomyolysis Severe 41 - 59% Palpitations, Dysrhythmias Hypotension Myocardial ischemia, Cardiac arrest Respiratory arrest Noncardiogenic pulmonary edema Seizures, Coma FATAL >60% Death
- 27. Delayed Neurological Sequelae(DNS): The delayed neurological sequelae may occur in up to 50% of poisoned people after 2 to 40 days (Lewis et al 2002). It is difficult to predict who will develop delayed sequelae; however, advanced age, loss of consciousness while poisoned, and initial neurological abnormalities may increase the chance of developing delayed symptoms include difficulty with higher intellectual functions, short-term memory loss, dementia, amnesia, psychosis, irritability, a strange gait, speech disturbances, Parkinson's disease-like syndromes, cortical blindness, and a depressed mood. Depression may even occur in those who did not have pre-existing depression.(Roohi et al 2001)
- 28. Concentration Symptoms (Goldstein et al 2008) 35 ppm (0.0035%) Headache and dizziness within six to eight hours of constant exposure 100 ppm (0.01%) Slight headache in two to three hours 200 ppm (0.02%) Slight headache within two to three hours; loss of judgment 400 ppm (0.04%) Frontal headache within one to two hours 800 ppm (0.08%) Dizziness, nausea, and convulsions within 45 min; insensible within 2 hours 1,600 ppm (0.16%) Headache, tachycardia, dizziness, and nausea within 20 min; death in less than 2 hours 3,200 ppm (0.32%) Headache, dizziness and nausea in five to ten minutes. Death within 30 minutes. 6,400 ppm (0.64%) Headache and dizziness in one to two minutes. Convulsions, respiratory arrest, and death in less than 20 minutes. 12,800 ppm (1.28%) Unconsciousness after 2–3 breaths. Death in less than three minutes.
- 30. Historical hint: In addition to the Holocaust during World War II, German Nazis used gas vans to kill an estimated 700,000 prisoners by carbon monoxide poisoning. This method was also used in the gas chambers of several death camps.
- 31. Differential diagnosis Carbon monoxide has been called a "great mimicker" due to the presentation of poisoning being diverse and nonspecific. Headaches (migrain, cluster, tension.. Etc) Flu-like viral syndromes Depression Chronic fatigue syndrome Acute cronary syndrome Acute respiratory distress syndrome Altitude sickness, Lactic acidosis, Diabetic ketoacidosis, Meningitis or encephalities. Methemoglobinemia, Or opioid or toxic alcohol poisoning (Shochat et al 2009)
- 32. Management
- 33. Diagnosis • The diagnosis of CO poisoning is a clinical one, the common definition requires: (Neil B. Hampson 2012). History of recent CO exposure, The presence of symptoms consistent with CO poisoning, And demonstration of an elevated carboxyhemoglobin level • Laboratory testing requires a blood sample (arterial or venous) and laboratory analysis on a CO-Oximeter.
- 34.
- 35. Emergency Department Evaluation Patients with confirmed or strongly suspected CO poisoning may be triaged according to their clinical status with Special attention be paid to airway management. Attention should be paid for co morbidities (burns, trauma, other inhalational injuries…..) Intubation of the comatose patient or, if necessary, for airway protection (ie ..laryngeal edema) Vital signs and a directed neurologic examination should be done immediatly, and the patient should have continuous cardiac monitoring. An IV catheter should be inserted. Non-invasive co-oximetry may be useful at triage to rapidly identify patients with significant CO exposure.
- 36. ECG and cardiac monitoring because of the potential for myocardial ischemia or dysrhythmia. Ventricular dysrhythmias or ST-segment changes are sometimes seen. (Anderson et al 1967).
- 38. RAD-57 Finger tip carboxyhemo globin saturation monitor (SpCO%) (Masimo RAD-57 Portable CO oximeter)
- 40. Patient evaluation It is directed at making the diagnosis, estimating the severity of poisoning, and identifying end-organ damage. Questions to ask include: • Where was the patient found, and under what circumstances? • Was there clear evidence of CO exposure? • Was there loss of consciousness? • Was there evidence of trauma? • Was a fingerstick glucose determination performed? • Was noninvasive co-oximetry performed? • Was prehospital ECG performed? • Was there evidence of attempted self-harm or suicidal intent?
- 41. In addition to standard medical history, ask about symptoms consistent with end-organ dysfunction or damage. These include: Headaches Alterations in mentation Difficulty performing simple mathematical tasks Visual changes Syncope Other focal neurologic symptoms, or seizure. All patients, regardless of age or health status, should be asked about the presence of chest pain shortness of breath dyspnea on exertion, palpitations, or lightheadedness. Female patients should be asked about the possibility of pregnancy. All patients with CO poisoning should be questioned directly regarding suicidal intent.
- 42. Physical examination General: for burns and coexistent trauma, evaluation of the oropharynx for edema and soot, neck for stridor. Vital signs: for arrythmia, Hypotension that may indicate cardiogenic shock due to ischemia, or it may be related to acidosis or other Co-inhalants, such as cyanide. Skin: Classic cherry red skin is rare, usually detected postmortem (ie, "When you're cherry red, you're dead"); pallor is present more often. Pulmonary examination: for small airway obstruction as wheezing in patients who are exposed to smoke or have inhaled other irritants. Also “cardiac wheezing” or crackles signifying myocardial depression secondary to smoke inhalation.
- 43. Cardiac examination: new gallop may represent acute diastolic dysfunction. Neurological: Cranial nerves, motor, and sensory examination performed to detect any focal neurologic deficits. cerebellar function tests may also detect abnormalities not evident on gross examination. Gait testing is a must, because ataxia can be a presenting sign of neurotoxicity and may be missed if the patient is not observed while ambulating. Ophthalmologic Flame-shaped retinal hemorrhages Bright red retinal veins (a sensitive early sign) Papilledema Homonymous hemianopsia.
- 44. Diagnostic Studies Co-oximetry: SpCO measured with the RAD-57 was not a substitute for standard blood COHb measurement. However, noninvasive pulse CO-oximetry could be useful as a first-line screening test, enabling rapid detection and management of CO-poisoned patients in the emergency department. (Mustapha et al, RCj 2013) So,It cannot be considered the standard of care.
- 45. Carboxyhemoglobin level: Normal circulating levels in the blood are 0% to 3%, and are higher in smokers. Carbon monoxide levels cannot be assessed through a physical exam. (Roth and Herkner 2010). Done for all patient with known or suspected CO poisoning The relationship between COHb levels and poisoning severity is generally poor; accordingly, this should be obtained while initiating empiric treatment (Harper et al 2004). A COHb level greater than 3% in non-smokers or greater than 10% in smokers suggests an abnormal CO exposure.
- 46. ABG and serum lactate: Lactic acidosis due to increased anaerobic cellular metabolism in the setting of tissue hypoxia (Sokal et al 1985) Cardiac Biomarkers: if: (MMWR 2004) Patients have ECG changes suggestive of ischemia, Symptoms consistent with myocardial ischemia. History of coronary artery disease. Age greater than 65 years. Pregnancy testing: As elimination of CO from fetal hemoglobin takes over 3 times as long as it does for the mother. (Hill EP et al 1977)
- 47. Other tests: Creatinine kinase, urine myoglobin: Nontraumatic rhabdomyolysis Complete blood count: mild leukocytosis/ DIC-TTP Electrolytes and glucose level : Lactic acidosis, hypokalemia, and hyperglycemia with severe intoxication BUN and creatinine levels :Acute renal failure secondary to myoglobinuria Liver function tests : Mild elevation in fulminant hepatic failure Urinalysis : Positive for albumin and glucose in chronic intoxication Methemoglobin level : normal 0-12% ,Included in the differential diagnosis of cyanosis with low oxygen saturation but normal PaO2 Toxicology screen :volatile alcohols, salicylates, acetaminophen levels, if altered mental status or in patients who present after a suicide attempt. Ethanol level : A confounding factor of intentional and unintentional poisonings
- 48. Chest Radiography: pulmonary edema, aspiration pneumonitis, pneumothorax, or other underlying preexisting condition such as (COPD). Changes such as ground-glass appearance, perihilar haze, and intra-alveolar edema imply a worse prognosis than normal findings. CT scan: head and cervical spine if suspected trauma or altered mental status, For patients who will be undergoing HBO therapy for concealed hemorrhage.
- 51. Admission should be considered for patients : with symptoms of moderate or severe CO poisoning, such as altered mental status or persistent neurologic or cardiovascular dysfunction. (with or without COHb >20%). These patients may have comorbidities, such as concurrent cardiac ischemia, burns, or hemodynamic instability, each of which requires specialized care.
- 53. 1-Normobaric oxygen It is a 100% oxygen given at atmospheric pressure using non rebreather mask, It is the mainstay of treatment. It is continued until the patient is asymptomatic and HbCO levels are below 10%. In patients with cardiovascular or pulmonary compromise, lower thresholds of 2% have been suggested. Calculate a gross estimate of the necessary duration of therapy using the initial level and half-life of 30-90 minutes at 100% oxygen Carbon monoxide is competitively displaced from hemoglobin and eliminated from the body via the pulmonary circulation. CO half-life is inversely proportional to the fraction of inspired oxygen. The elimination half-life is approximately 300 minutes on room air, 90 minutes on reservoir “non-rebreather” facemask, and 30 minutes breathing HBO.(Ernst A et al 1998)
- 54. 2-Hyperbaric oxygen therapy (HBO): HBO is defined as 100% inspired oxygen delivered at greater than 1.4 atm of pressure in a special chamber. Treatment regimens usually involve 100% oxygen at 2.4-3 atm for 90-120 minutes. It is supposed that HBO is benificial o Increased elimination of HbCO o Remove CO from cytochrome oxidase, inhibit adherence of neutrophils on vascular endothelium, and prevent the downstream effects of lipid peroxidation (Thom et al 1993) o Certain studies proclaim major reductions in delayed neurologic sequelae, cerebral edema, pathologic central nervous system (CNS) changes, and reduced cytochrome oxidase impairment.
- 55. Indications for hyperbaric oxygen therapy in carbon monoxide poisoning: (Hampson 2001) Currently Accepted Indications 1) Neurologic findings a. Altered mental status b. Coma c. Focal neurologic deficits d. Seizures 2) Pregnancy with CO-Hgb levels > 15–20% 3) History of loss of consciousness Relatively Considered for: a. Cardiovascular compromise (ischemia, infarction,dysrhythmia) b. Metabolic acidosis c. Extremes of age d. Elevated CO-Hgb level (>25–40%) e. Abnormal neuropsychometric testing results f. Persistent symptoms despite normobaric oxygen
- 59. Controverse about HBO therapy: With: Hyperbaric oxygen should at least be considered in all cases of serious acute CO poisoning and normobaric 100% oxygen continued until the time of hyperbaric oxygen administration. (Weaver et al 2007). Daily 100-minute treatments with 100% oxygen in a hyperbaric chamber–60 minutes at 2.8 atmospheres for 3 days, extended to 6 days if there were neurological abnormalities. (Scheinkestel et al 1999). CO-poisoned patients who received three hyperbaric oxygen treatments within 24 hours of presentation manifest approximately one-half the rate of cognitive sequelae at 6 weeks, 6 months, and 12 months after treatment as those who were treated with normobaric oxygen. (Weaver et al 2007).
- 60. Aginst: The use of HBO therapy in CO poisoning remains controversial (Juurlink et al 2005) There is insufficient evidence to support the use of hyperbaric oxygen for treatment of patients with carbon monoxide poisoning (Buckley et al 2011).
- 62. The American College of Emergency Physicians (ACEP) clinical policy final recommendations are: 1. Hyperbaric oxygen therapy is a therapeutic option for CO-poisoned patients; however, its use cannot be mandated. 2. No clinical variables, including carboxyhemoglobin levels, identify a subgroup of CO poisoned patients for whom hyperbaric oxygen therapy is most likely to provide benefit or cause harm. (wolf et al 2008)
- 63. 3-Treatment of complications Arrythmias: managed according to ACLS protocol. Acidosis : it is not recommended to treat acidosis with a PH above 7.15 because it results in a rightward shift in the oxyhemoglobin dissociation curve, increasing tissue oxygen availability. Acidosis generally improves with oxygen therapy. Treatment of potentially coexistent inhalational cyanide toxicity using cyanide antidote kit and cyanocobalamine. Treatment of delayed neurological sequalae.
- 64. COPD patients: Patients with carbon monoxide poisoning and a significant smoking history – even if not formally diagnosed with COPD – have regular ABG analysis during treatment to ensure that they are not developing a dangerous respiratory acidosis. Carbon dioxide retention in such patients limits the use of uncontrolled high-flow oxygen, and thus in certain circumstances early intubation may need to be considered. The use of hyperbaric oxygen therapy in such patients should be considered only with extreme caution. (Tristan et al 2008)
- 65. Pregnancy Fetal hemoglobin has a 10 to 15% higher affinity for carbon monoxide than adult hemoglobin, causing more severe poisoning in the fetus than in the adult (omaye et al 2002) In utero fetus are more vulnerable to CO toxicity because of the natural leftward shift of the dissociation curve of fetal hemoglobin. Acute, severe CO poisoning is associated with high maternal and fetal mortality. Steady state levels of COHb in the fetus are higher than in maternal blood. It takes longer to reach steady-state, and fetal elimination of CO is also prolonged. For these reasons, many centers advocate hyperbaric treatment for pregnant females with a cohb level greater than 20% or signs of fetal distress (decreased or absent fetal movement or fetal bradycardia) . (elkharrat et al 1991)
- 66. Discharge: Patients who did not have: 1. loss of consciousness. 2. who have complete recovery from any symptoms, 3. whose COHb level has returned to normal (Asymptomatic patients with levels below 10% may be discharged). 4. and who have no evidence of end-organ damage (ECG changes, elevated cardiac biomarkers, neurological deficits) may be safely discharged to home. (Lavonas EJ et al 2007) An observation unit stay would be a useful option for stable patients requiring prolonged NBO therapy. Only those patients showing signs of significant end-organ toxicity will require hospitalization, with or without HBO therapy.
- 68. Key message (Neil et al 2011) I. Basic pathophysiology: Several mechanisms of CO toxicity exist, in addition to relative hypoxemia from carboxy hemoglobin (COHb) formation. II. Diagnosis a. Symptoms: Nonspecific. Most common are headache, dizziness, nausea/vomiting, confusion, fatigue, chest pain, shortness of breath, and loss of consciousness. b. Signs: Cherry red discoloration is rare. c. Role of carboxy hemoglobin level: Confirms clinical diagnosis. Correlates poorly with symptoms or prognosis d. Pre diagnosis management: Administer 100% oxygen while waiting for COHb level.
- 69. III. Management a. Normobaric oxygen therapy: If chosen for treatment, 100% oxygen by nonrebreather facemask or endotracheal tube until COHb normal (,3%) and patient asymptomatic (typically 6 h) b. Selection for hyperbaric oxygen (HBO) therapy: Currently not completely clarified. Poisoned patients with loss of consciousness, ischemic cardiac changes, neurological deficits, significant metabolic acidosis, or COHb.25% warrant HBO2. More mildly poisoned patients may be treated accordingly. c. Goals of HBO2therapy: Prevent neurocognitive sequelae d. Optimal HBO protocol: Unknown. Recommend retreatment of persistently symptomatic patients to a maximum of 3 treatments. e. Intentional poisonings: Coingestion of other toxins commons. Consider toxicological screening f. Concomitant cyanide poisoning: Suspect if CO source is house fire. Consider empiric treatment if pH 7.20 or plasma lactate.10 mmol/L.
- 70. IV. Patient follow-up a. Accidental poisoning: Follow-up in 4–6 wk to screen for cognitive sequelae b. Intentional poisoning: Psychiatric follow-up mandatory in light of high rate of subsequent completed suicide V. Prevention a. Public education: Educate about proper generator use and risk from combustion of fuels indoors b. CO alarms: Encourage minimum of 1 per home, located near sleeping area. Replace alarms every 5–7 yr, as per manufacturer’s instructions
- 71. Thank you
- 72. References Diagnosis And Management Of Carbon Monoxide Poisoning In The Emergency Department, February 2011 Volume 13, Number 2: Heikki Nikkanen, MD, FAAEM, FACMT Attending Physician, Brigham and Women’s Hospital, Department of Emergency Medicine, Boston, MA Aaron Skolnik, MD Chief Resident, Harvard Affiliated Emergency Medicine Residency, Brigham and Women’s Hospital Department of Emergency Medicine, Boston, MA
- 73. Goldstein M (December 2008). "Carbon monoxide poisoning". Journal of Emergency Nursing: JEN: Official Publication of the Emergency Department Nurses Association 34 (6): 538–542. doi:10.1016/j.jen.2007.11.014. PMID 19022078. Roohi F, Kula RW, Mehta N (July 2001). "Twenty-nine years after carbon monoxide intoxication". Clinical Neurology and Neurosurgery 103 (2): 92–95. doi:10.1016/S0303-8467(01)00119- 6. PMID 11516551 Hampson NB, Hampson LA (March 2002). "Characteristics of headache associated with acute carbon monoxide poisoning". Headache 42 (3): 220–223. doi:10.1046/j.1526-4610.2002.02055.x. PMID 11903546. Omaye ST (Nov 2002). "Metabolic modulation of carbon monoxide toxicity". Toxicology 180 (2): 139–50. doi:10.1016/S0300-483X(02)00387-6. PMID 12324190
- 74. Sokal JA, Kralkowska E. The relationship between exposure duration, carboxyhemoglobin, blood glucose, pyruvate, and lactate and the severity of intoxication in 39 cases of acute carbon monoxide poisoning in man. Arch Toxicol.1985;57:196- 199.(Prospective, descriptive study; 39 patients Ernst A, Zibrak JD. Carbon monoxide poisoning. N Engl J Med.1998;339:1603-1608. (Review article) Juurlink DN, Buckley NA, Stanbrook MB, et al. Hyperbaric oxygen for carbon monoxide poisoning. Cochrane Database Syst Rev.2005;(1):CD002041. (Meta-analysis)
- 75. Thom SR. Functional inhibition of leukocyte B2 integrins by hyperbaric oxygen in carbon monoxide-mediated brain injury in rats. Toxicol Appl Pharmacol.1993;123: 248-256. (Animal study) Elkharrat D, Raphael JC, Korach JM, et al. Acute carbon monoxide intoxication and hyperbaric oxygen in pregnancy. Intensive Care Med. 1991;17:289-292. (Prospective study; 44 patients) Lavonas EJ. Carbon monoxide poisoning. In: Shannon M, Borron S, Burns M, eds. Haddad and Winchester’s Clinical Management of Poisoning and Drug Overdose.Philadelphia, Pa: Elsevier; 2007:1297- 1307. (Textbook chapter) Diagnosis And Management Of Carbon Monoxide Poisoning In The Emergency Department
- 76. Wolf SJ, Lavonas EJ, Sloan EP, et al. Clinical policy: critical issues in the management of adult patients presenting to the emergency department with acute carbon monoxide poisoning. Ann Emerg Med.2008;51(2);138-152. (Clinical policy) Harper A, Croft-Baker J. Carbon monoxide poisoning: undetected by both patients and their doctors. Age Ageing.2004;33:105-109 Anderson EF, Allensworth DC, DeGroot WJ. Myocardial toxicity from carbon monoxide poisoning. Ann Internal Med.1967;67:1172-1182 Centers for Disease Control and Prevention. Carbon monoxide poisonings resulting from open-air exposures to operating motorboats - Lake Havasu City, Arizona, 2003. MMWR.2004;53(15);314- 318 Hill EP, Hill JR, Power GG, et al. Carbon monoxide exchanges between the human fetus and mother: a mathematical model. Am J Physiol.1977;232:H311-H323.
- 77. Carbon monoxide poisoning in a patient with carbon dioxide retention: a therapeutic challenge,Tristan RA Lane,corresponding author1 WilbyJ Williamson,1 and Joshua M Brostoff1,Cases J. 2008; 1: 102.Published online Aug 18, 2008. doi: 10.1186/1757-1626-1-102. Buckley NA, Juurlink DN, Isbister G, Bennett MH, Lavonas EJPublished Online:13 April 2011There is insufficient evidence to support the use of hyperbaric oxygen for treatment of patients with carbon monoxide poisoning. Buckley NA, Juurlink DN, Isbister G, Bennett MH, Lavonas EJ. Hyperbaric oxygen for carbon monoxide poisoning. Cochrane Database Syst Rev. Apr 13 2011;4:CD002041.
- 78. Hyperbaric Oxygen for Acute Carbon Monoxide Poisoning, Weaver et al 2002,N Engl J Med 2002; 347:1057-1067October 3, 2002DOI: 10.1056/NEJMoa013121. Hyperbaric oxygen for carbon monoxide poisoning Nick A Buckley1,*,David N Juurlink2,Geoff Isbister3,Michael H,Bennett4,Eric J Lavonas5 Editorial Group: Cochrane Injuries Group Published Online: 13 APR 2011,Assessed as up-to-date: 6 JUN 2010,DOI: 10.1002/14651858.CD002041.pub3 Practice Recommendations in the Diagnosis, Management, and Prevention of Carbon Monoxide Poisoning Neil B. Hampson1, Claude A. Piantadosi2, Stephen R. Thom3, and Lindell K. Weaver4,2012 the American Thoracic Society.
- 79. Penney DG. Hemodynamic response to carbon monoxide. Environ Health Perspec 1988;77:121–30.
