Presentation1.pptx, f mri of brain neoplasm
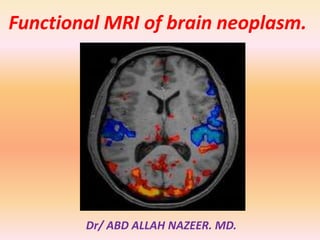
- 1. Functional MRI of brain neoplasm. Dr/ ABD ALLAH NAZEER. MD.
- 2. Functional magnetic resonance imaging (fMRI) is increasingly used in the work-up of patients at the preoperative stage to assess the relationship between the functionally eloquent cortex and brain pathology. Inter-individual normal variations of anatomy render such assessment unreliable based on structural imaging alone despite the definition of clear anatomical landmarks. This is even more of an issue when normal anatomy is obscured by a tumour mass effect or when functional anatomy is altered due to cortical plasticity. fMRI has seen a rapid evolution from its first human application in 1991 to an essential tool in the exploration of human brain function, most prominently in the scientific arena. In 2007, new Current Procedure Terminology (CPT) codes were developed for fMRI by the American Medical Association, signifying the transition of fMRI to a valuable tool in a clinical setting. Recent major advances in clinical fMRI make its acquisition, image processing, and even integration of its findings for neuronavigational purposes relatively easy. However, the technique is not without limitations and validation issues which are easily forgotten when color activation maps become readily available at the single click of a button. The theoretical background, the validity in brain tumour patients, and several considerations of fMRI are addressed.
- 3. fMRI Background: Blood Oxygenation Level-Dependent (BOLD) fMRI is the most commonly used functional MR neuroimaging technique. BOLD fMRI takes advantage of the tight link between local neuronal activity and blood flow, called neurovascular coupling due to neurovascular coupling, blood flow and volume increase locally with an increase of neuronal activity. This leads to an increase in oxygenated blood that is disproportionate to the increased need of oxygen for neuronal activity. As a result, there is a relative decrease of paramagnetic deoxygenated hemoglobin which in turn leads to an increase of MR signal in those areas of the brain that are active. Such signal changes are small and relative, which means that many measurements need to be made, typically during an alternation of active and baseline conditions in a task that aims to activate the functional brain region of interest. Furthermore, the signal changes occur at a delay after and are more prolonged than the neuronal activity, defined by the hemodynamic response function. A statistical model is created to assess the correlation of the measured signal changes with the task, taking the hemodynamic response function into account. The resulting statistical map is threshold at a certain p or T value and overlaid in color on a high-resolution anatomical image which is acquired separately. This is the typical color “activation” map produced by an fMRI image processing software, which is merely a combination of anatomical and statistical information very indirectly representing neuronal activation.
- 4. Task-Based fMRI For clinical application, almost exclusively task-based fMRI is used. During the performance of a task by the subject in the scanner, rapid imaging of the brain is performed. Typically, the entire brain is scanned at intervals of 3–5 s for a duration of about 5 min so that > 100 measurements are made per task. The task consists of active and baseline conditions, which commonly alternate in blocks of 20–40 s. Such so-called blocked paradigms are statistically robust, since a lot of signal is acquired for each condition, but they are restrained because they do not leave much room for unexpected or short stimuli. In an event-related task design, individual stimuli, each representing a specific condition, are presented in random order and rapid succession. Such a task design offers the possibility to present unexpected stimuli as well as many different condition. Rendering it very flexible, but statistically less robust since the signal acquired per condition is generally low. For clinical application, blocked designs are generally well-suited and preferable.
- 5. Clinical Pre-Surgical fMRI Studies: The aim of neurosurgery in brain tumour patients is maximum tumour resection, while at the same time minimizing the risk of new functional deficits post-operatively. For optimal results, the relationship between the tumour margins and eloquent brain regions needs to be established as accurately as possible. The gold standard for such assessment is intraoperative ECM, which has in fact been shown to significantly modify long-term survival in low-grade glioma patients. However, intraoperative ECM is invasive, requires experience and expertise of the neurosurgical team, increases surgery duration, and requires awake and active participation, collaboration, and motivation of the patient. Additionally, only a limited number of tasks can be tested. Functional MRI may be used to make a risk assessment preoperatively, which is of particular value in young low-grade glioma patients, to plan and guide the neurosurgical approach, shorten surgery duration, and obtain prognostic information prior to surgery. For fMRI to be used in such a setting, both high sensitivity and high specificity are required. High sensitivity for eloquent brain regions is needed to reduce the false negative rate so that no eloquent cortex is missed and no functional deficit is induced by surgery. At high specificity the false positive rate is low, which means that the visualized areas of activation relate to truly eloquent or critical brain regions. At low specificity non-critical brain regions are also visualized, inducing the risk that such areas are avoided at surgery and are subsequently exposed to a less extensive resection than would have been possible.
- 6. Motor Function: Motor cortex assessment has been validated in a multitude of studies that generally report a good correlation between fMRI and intraoperative ECM. Reported sensitivities for localization of the primary motor cortex range from 88–100 % . Specificities are also high, ranging from 87–100 % . Such high reliability may be contributed to by the robust activation that is seen with simple motor tasks that can be easily performed by the majority of patients. Also the functional anatomical stability of the sensorimotor area, at both the macroscopic and microscopic levels, probably contributes to the reliability of fMRI of motor function . Spatial accuracy of fMRI motor cortex localization is found to be within the range of 1–2 cm. Yetkin et al reported that all intraoperative ECM and fMRI sites of activation were within 2 cm, while 87 % were within 1 cm. Importantly though, reliability seems to be decreased with high tumour grades, as demonstrated by Bizzi et al. In benign and malignant brain mass lesions in or near the primary motor cortex, overall sensitivity was 88 %, but only 65 % in grade-IV gliomas.
- 7. Language Function: In contrast to the high validity shown for fMRI of motor function, results from language function validation studies are controversial, varying from 100 % sensitivity for fMRI to identify all critical language areas to as low as 22 %. Reported specificity is even more variable, ranging from 0– 100 %. Validation studies of fMRI of language function in brain tumour patients are relatively scarce, are generally performed in small patient populations, and suffer from differences in the validation methods used among the studies, disparities of brain lesions, and the variety of the language tasks performed preoperatively and during intraoperative ECM. The mapping of language function is also more complex than that of the sensorimotor cortex due to the lack of consistent surface landmarks and substantial inter-individual variability. The language cortical network seems to consist of critical regions, essential for language processing, and participating but non-critical areas, which may be resected without inducing a permanent language deficit. These areas cannot be reliably distinguished with fMRI, resulting in low specificity of fMRI compared with intraoperative ECM.
- 8. Other Functions: The visual cortex has been a frequent topic of study since the early days of fMRI, due to its relatively strong BOLD response and easy implementation of stimulus paradigms. Presurgical mapping of the primary visual cortex has been described and may be indicated when the normal anatomy is severely distorted by the tumour and/or when the brain structure of interest is located deep inside the brain and cannot be assessed by ECM. Commonly used stimulus paradigms are flashing lights presented with light-proof goggles and reversing black-and-white checkerboards . Another function that may be assessed with fMRI is visuospatial attention, failure of which results in spatial neglect. This condition arises with damage of the temporoparietal or frontal cortex, the thalamus or the basal ganglia, generally of the right hemisphere. It is an invalidating condition, in which patients behave as if the left part of the world does not exist. Functional localization may be assessed with fMRI using a line bisection task, in which patients are asked to bisect 20-cm horizontal lines, which has been used successfully during ECM.
- 9. Critical Issues: There are several limitations of fMRI that need to be considered when using the technique for pre-surgical assessment of brain tumour patients. These include issues that are inherent to the technique, such as spatial and geometric uncertainty, tumour effects on the BOLD signal, inter- and intra-individual variability, lack of discrimination between essential and modulating brain regions, and lack of information on the underlying white matter. The imaging sequence used for BOLD fMRI is particularly sensitive to postoperative effects, such as metallic implants and surgical staples, air underneath the skull flap, and blood products, as well. This means that additional care needs to be taken in patients who have had previous surgery, biopsy, or hemorrhage. Small regions of hemosiderin deposition may not be visible on conventional imaging, but will show large artifacts in the BOLD fMRI data. Such artifacts are obscured on the fMRI activation color maps, which would simply show decreased or no activation in the artefactual area. It is therefore crucial that the raw data are scrutinized for such artifacts in every patient. Other issues with pre-surgical fMRI, that may be resolved in the future, are the lack of standardization of tasks and image processing techniques.
- 10. Four resting state networks in a normal subject. Also shown are corresponding time courses of the independent component coefficients.(Colors quantify the z-value of correlation of the time series with the corresponding ICA coefficient. Either positive or negative z-values are shown.)
- 11. Activation patterns in response to visual stimuli. Note the lack of activation in the central visual cortex when using projection screen.
- 12. Visual area locations. A, Parasagittal anatomical image from one subject indicating the slice selection (perpendicular to the calcarine sulcus) for the retinotopy measurements and the control conditions. B–D, Visual areas V1, V2, V3, V3A, and V4v depicted on in-plane anatomies from a similar location (near the middle of the 8 in-planes) in three control subjects. E–G, Visual areas depicted on in-plane anatomies from a similar location in three dyslexic subjects.
- 13. Location of area MT1. A, Parasagittal anatomical image from one subject indicating the slice selection (parallel to the calcarine sulcus) for the moving dots and the test conditions. The blue lines were slices that contained the MT1 region of interest (ROI) in this subject. B– D, Brain activity in one slice containing the MT1 ROI from three control subjects. Reddish voxels show regions with greater response to moving versus stationary dot patterns. Images were chosen to optimally show MT1 in the right hemisphere (arrows), although activity from left hemisphere MT1 and V1 are also present in some cases. The image in B is from the same brain as the sagittal image in A and corresponds to the most inferior of the three blue slices. The MT1 ROI was defined by outlining (dotted line in B) the strongest area of activity that was approximately lateral to the junction between the calcarine sulcus and the parieto-occipital sulcus, and beyond the retinotopically organized visual areas. E–G, Slices with MT1 ROIs in three dyslexic subjects.
- 14. This image is in radiological format and shows an auditory language map averaged over 40 subjects. There is bilateral primary auditory cortex (yellow arrows), left Wernicke’s (green arrows) and Broca’s (red arrows), and SMA (orange arrows). In this auditory task, the subject hears phrases, such as “The funny guys at the circus” and thinks in his/her mind of a word that fits.
- 15. Typical pattern of language activation in Reverse Word Reading Task
- 16. Figure 4. Functional reorganization of motor area was observed in the patients with short term and long term spinal cord injury (sci). Figure 4a. Control. Figure 4b. Two years after sci. Figure 4c. More than 10 years after sci.
- 20. Localization of primary motor cortices in 28 years old patients with brain tumor: Note that the posterior and medial displacement of motor cortices by the mass lesion
- 21. Localization of language cortices in 28 years old patients with brain tumor: Note that the strong left lateralization of language activities.
- 23. Localization of primary motor cortices in 28 years old patients with brain tumor in 3 views
- 25. fMRI in preoperative planning. 3a. Preoperative planning for brain biopsy in a patient with a lesion (arrow) in the left frontal lobe (Broca’s area). Significant bilateral language activation was observed in this patient. 3b. fMRI was used to determine the language area and its relation to the tumor for a patient with glioblastoma (arrow).
- 32. Patient K, male, 37 years old, with glioblastoma in the left temporoparietal area,activation from visual task, R - right hemisphere; L - left hemisphere.
- 33. Patient P, male, 28 years old, with glioblastoma in the left temporal lobe, activation from visual and auditory tasks, R - right hemisphere; L - left hemisphere, WA – activation in Wernicke's area. Red - activation elicited by visual task, blue - activation elicited by auditory task, purple - activation that coincided in two tasks.
- 34. Patient KO, female, 53 years old, with glioblastoma in the left parietal area, activation from visual task (red), R - right hemisphere; L - left hemisphere.
- 35. Preoperative (A) activity showing the focus of activity in 4 patients obtained from the comparison of the visuomotor conditional blocks of trials with the motor control blocks of trials and postoperative (B) anatomical images. A: Functional MR images show the focus of activity within the rostral part of the premotor cortex in the lateral view (in all patients) and in the top view (in Case 2) of the cortical surface rendering in standard stereotactic space of the left hemisphere of each patient. The gray shaded area of the cortical surface shows the tumor location. Each blue cross indicates the location of the preoperative activity increase in the PMdr. The color scale indicates the t value range. B: Magnetic resonance images show the cortical surfaces as renderings (in standard stereotactic space) of the left hemisphere of each patient based on the postoperative MR image. The deformation of the cortical surface shows the extent of the tumor resection. The data demonstrate that, in each patient, the region involved in the visuomotor conditional function was not removed during the tumor resection.
- 36. Images showing the preoperative activity obtained from the comparison of the motor control with the visual control block of trials. The cortical surfaces are renderings (in standard stereotactic space) of the left hemisphere of each patient. The horizontal yellow line indicates the dorsoventral level of the horizontal sections illustrated in the images on the right. The increases in activity correspond to the location of the primary hand motor region in the precentral knob of each patient,
- 37. Tumor heterogeneity Recognition Evaluation on the High Grade Glioma of the BraTS dataset: Qualitative Example Case BRATS HG0001 a) Gadolinium T1 MRI Original Image b) FLAIR MRI Original Image c) Overlap between Gadolinium T1 MRI original image and the Ground Truth masks d) Overlap between Gadolinium T1 MRI original image and the automatic recognized masks.(Red points are Edema and Cyan point are the Active Tumor
- 38. Tumor heterogeneity Recognition Evaluation on the High Grade Glioma of the BraTS dataset: Qualitative Example Case BRATS HG0001 a) Gadolinium T1 MRI Original Image b) FLAIR MRI Original Image c) Overlap between Gadolinium T1 MRI original image and the Ground Truth masks d) Overlap between Gadolinium T1 MRI original image and the automatic recognized masks.(Red points are Edema and Cyan point are the Active Tumor)
- 41. 18-year old boy with a glioma grade 3 (arrows) near the left rolandic area, demonstrating the importance of fMRI in planning surgery and avoiding postoperative neurological deficits. fMRI using a visuomotor paradigm showed functional activation less than 2 cm posterior to the tumour and partial resection was proposed (A,B). Partial resection was performed using intra-operative cortical stimulation, and followed by application of gene therapy in the tumour remnant posteriorly. Postoperatively, no motor deficit was present.
- 42. 26-year old man with right frontal glioma demonstrating the role of fMRI in deciding on operability. This man was left-handed which increased chances that language areas are not confined solely to the left hemisphere. fMRI using a verb generation paradigm showed that the language areas Broca (B) and Wernicke (W) were strongly lateralized to the left hemisphere because no activation was seen in the right hemisphere. Complete resection of the right frontal glioma (T) was performed and the patient did not have any language deficit postoperatively.
- 43. 59-year old woman with arteriovenous malformation (AVM) in the right parieto-occipital region, demonstrating risk for postoperative deficit because activation areas are less than 2 cm of the lesion. fMRI using a visuomotor paradigm showed visual activation areas (green) medially and caudally relative to the AVM (circle), at less than 1 cm distance. After endovascular approach with partial embolisation, complete resection was performed surgically. Postoperatively, a left lower quadrant anopsy was present.
- 44. (Top row) Acquired axial CT and anatomical MRI slices from the AVM patient. (Bottom row left) fMRI activation map fused with the anatomical MRI data showing the Broadmann-17 functional structure and (lower right) corresponding color-coded (red = left-right; green= anterior-posterior; blue = superior-inferior). The FA map was used for calculating the tractography data.
- 45. Recurrent left parietal lobe anaplastic astrocytoma in 37- year-old right-handed woman. Surgery was not initially planned because of presumed involvement of receptive speech area. Left inferior and middle frontal gyral activation (yellow arrows) is consistent with dominant expressive speech area and is located at anterior border of more cephalad component of lesion. Left superior and middle temporal gyral activation (green arrows) is consistent with dominant receptive speech area and abuts inferior border of temporal component of lesion, with superior temporal gyral activation component lying anteroinferior to lesion.
- 46. Preoperative fMRI in patients during contralesional movements. Preoperative anatomic and functional MRI in Patients 1, 5, and 8 (left column) showed large tumoral infiltration of the supplementary motor area (SMA) (asterisk), associated with under activity in the SMA in the pathologic hemisphere, and over activity in the healthy SMA resulting in negative magnitude laterality indices (LI) (0.40, 0.12, 0.06). Recovery began within the first 3 days and lasted between 30 and 60 days. In Patients 6, 9, and 11 (right column), tumoral infiltration (asterisk) was lower, and LI remained positive (0.08, 0.19, 0.12). Arrows indicate predominant SMA activation. Recovery began after 7 to 21 days, and lasted between 90 and 120 days.
- 47. Postoperative fMRI. Anatomic and functional MRI in one representative control and in Patients 4, 6, and 12 during ipsilesional (IL) and contralesional (CL) movements after surgery. In controls and in patients during IL movements, supplementary motor area (SMA) (arrow) and premotor cortex (PMC) (arrowhead) activation predominated in the hemisphere contralateral to the moving hand. In patients during CL movements, SMA activation was located in the healthy hemisphere and PMC activation became more important in the ipsilateral healthy hemisphere. The resection cavity is indicated by the asterisk on axial planes.
- 48. Axial TIWI in neurologic format show left megalencephaly with an enlarged dysmorphic left cerebral hemisphere. There is poly microgyria as well as heterotopia. During this auditory task, there was only activation in the right primary auditory cortex (yellow arrow) rather the expected bilateral activation. (Color version of figure is available online.)
- 49. Conclusions. Functional MRI is a valuable tool in the pre-surgical assessment of brain tumour patients, but needs to be used with care. Interpretation of the results requires a lot of experience and may be difficult. Knowledge of functional brain anatomy is a first requirement for risk evaluation and to determine which fMRI tasks need to be performed. The shortcomings of fMRI in a clinical setting as described above need to explicitly be taken into account in every patient. In our institution, fMRI, combined with DTI tractography, is used to aid neurosurgical planning but intraoperative ECM is always used for confirmation when activation is shown in the proximity of the brain tumour or if activation is atypical. Most importantly, the absence of fMRI activation does not exclude the presence of functional neuronal tissue, not even within infiltrative tumours.
- 50. Thank You.
