L8: B-adrenergic blockers
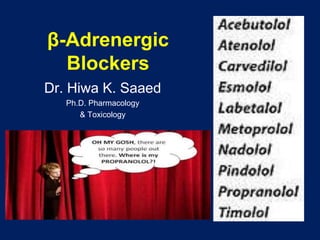
- 1. β-Adrenergic Blockers Dr. Hiwa K. Saaed Ph.D. Pharmacology & Toxicology
- 3. β-Adrenergic Blockers β-Blockers are effective in treating : • angina, • cardiac arrhythmias, • myocardial infarction, • congestive heart failure, • hyperthyroidism, • and glaucoma, • prophylaxis of migraine headaches. Note: The names of all β-blockers end in “olol” except for labetalol and carvedilol.
- 4. β-Blockers • All are competitive antagonists • Propranolol is prototype • Although all β-blockers lower blood pressure in hypertension, they do not induce postural hypotension, • because the α-adrenoceptors remain functional.
- 5. A. Classification and Mechanisms Selectivity (β1>β2) Partial agonist activity (Intrinsic Sympathomimetic Activity “ISA”) Lipid solubility (CNS effect) Membrane stabilizing activity (MSA) (local anesthetic action) Capacity to block alpha adrenoceptors. K+ channel blockade (sotalol)
- 6. A. Classification: Selectivity (β1>β2) • β1 selective (cardioselective) • Atenolol • Acebutolol • Bisoprolol • Esmolol (short t1/2) • Metoplrolol Advantage: HTN with asthma, peripheral vascular disease (coldness of extremities), NIDDM
- 7. A. Classification and Mechanisms Selective β2 • Butoxamine (experimental) Nonselective (β1 & β2) • Nadolol • Propranolol • Timolol
- 8. Combined (α & β): peripheral vasodilation • Labetalol • Carvedilol • Useful in Rx HTN patients for whom increased Peripheral resistance is undesirable (elderly or black) • Labetalol in Rx preeclampsia, pheochromocytoma • They do not alter serum lipid or blood glucose levels • Carvedilol also decreasees lipid peroxidation and vascular wall thickening (benefit in heart failure)
- 9. Partial agonist activity ISA • Pindolol • Acebutolol • Labetalol less bradycardia & diminished effect on COP, less disturbances of lipid and carbohydrate metabolism Advantages: • HTN with asthma, • HTN with moderate bradycardia • HTN+DM
- 10. A. Classification and Mechanisms 3. Local anesthetic activity (membrane-stabilizing activity): – Is a disadvantage when used topically in the eye because it decreases protective reflexes and increases the risk of corneal ulceration – Timolol, atenolol, carvedilol &nadolol: no Local anesthetic activity
- 11. 4. Lipid solubility – responsible for CNS adverse effects: propranolol Lipid soluble Pharmacokinetic properties Water soluble Pharmacokinetic properties Propranolol Highly metabolized Large Vd CNS penetration Shorter t1/2 Acebutolol Excreted unchanged by kidney Less 1st pass effect Small Vd Longer t1/2 except esmolol Timolol Atenolol Pindolol Esmolol Metoprolol Nadolol Labetalol
- 12. K+ channel blockade: sotalol • Sotalol is a nonselective β receptor antagonists, • that lack LA action • but has marked class III antiarrhythmia effect reflecting k+ channel blockade
- 13. B. Pharmacological Effects and Clinical Uses 1. CVS: A. Heart: both – decreased HR, force of contraction (–ve inotropic & chronotropic effect) – decreased A-V conduction, ↑PR interval – Decrease CO, work & O2 consumption Rx: Angina and Supraventricular tachycardia
- 14. Reflex peripheral vasoconstriction!? B. Vascular system: prevent β2 mediated vasodilation→ reduction in COP (because of cardiac effect) → decrease BP → reflex vasoconstriction. • On balance there is gradual reduction of both systolic and diastolic BP
- 15. 2. Respiratory: bronchoconstriction; contraindicated in asthma 3. Eye: reduce IOP especially in Glaucomatous eyes decrease aqueous humor production B. Pharmacological Effects and Clinical Uses
- 16. 4. metabolic and endocrine effects: A. Increased Na+ retention, how? – Reduced blood pressure causes a decrease in renal perfusion, resulting in an increase in Na+ retention and ↑plasma volume→ – In some cases, ↑blood pressure. – For these patients, β-blockers are often combined with a diuretic to prevent Na+ retention. – Also by inhibiting β receptors, renin production is also prevented, contributing to Na+ retention. B. Pharmacological Effects and Clinical Uses
- 17. B. inhibit lipolysis: ↑ plasma VLDL, ↓ HDL, ─LDL ↓ HDL/LDL ratio→ coronary heart disease C. partially inhibit glycogenolysis and decrease glucagon secretion • Great caution in IDDM (Type 1)? • Because pronounce hypoglycemia may occur after insulin injection, β blockers also attenuate the normal physiologic response to hypoglycemia, furthermore they mask signs of hypoglycemia; tremor, palpitation.. B. Pharmacological Effects and Clinical Uses
- 18. B. Clinical Uses Cardiovascular and ophthalmic applications are extremly important A. CVS: -angina pectoris ↓cardiac work & O2 demand, -Chronic hypertension, ↓CO, ↓ TPR, inhibition of renin release NB: β blockers are not used for acute or emergency Rx of HTN,? ma y increase diastolic pressure Labetalol is effective in emergency
- 19. -Arrhythmia (supraventricular tachycardias), -prophylaxis after MI: 1) early use within 6-12 hrs for 3-4 wks 2) Late use within 4 days- 4 wks after onset of infarction and continued for at least 2 years useful for secondary prevention from another MI - congestive heart failure* B. Clinical Uses
- 20. B. Eye: Glaucoma: reduce aqueous humor secretion (timolol) C. Endocrine use: Thyroid storm, thyrotoxicosis: propranolol D. CNS: propranolol 1. Anxiety with somatic symptoms 2. Migraine headache prophylaxis: 3. Famillial tremor, other types of tremor, “stage fright”: 4. Alcohol, opioids acute withdrawal symptoms B. Clinical Uses
- 21. C. Adverse effects • CVS: bradycardia, A-V blockade, CHF • Arrhythmias: never stop Rx with β blockers suddenly • Bronchoconstriction: Patients with airway disease: asthmatic attack • Sexual dysfunction?? Indep of β blockade • CNS effects: sedation, fatigue, sleep alterations
- 22. Thank You
