Case Study_Pharmacology
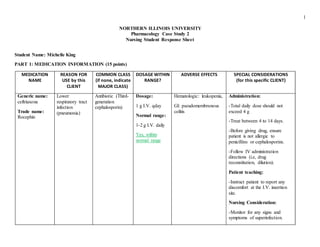
- 1. 1 NORTHERN ILLINOIS UNIVERSITY Pharmacology Case Study 2 Nursing Student Response Sheet Student Name: Michelle King PART 1: MEDICATION INFORMATION (15 points) MEDICATION NAME REASON FOR USE by this CLIENT COMMON CLASS (if none, indicate MAJOR CLASS) DOSAGE WITHIN RANGE? ADVERSE EFFECTS SPECIAL CONSIDERATIONS (for this specific CLIENT) Generic name: ceftriaxone Trade name: Rocephin Lower respiratory tract infection (pneumonia) Antibiotic (Third- generation cephalosporin) Dosage: 1 g I.V. qday Normal range: 1-2 g I.V. daily Yes, within normal range Hematologic: leukopenia, GI: pseudomembranous colitis Administration: -Total daily dose should not exceed 4 g -Treat between 4 to 14 days. -Before giving drug, ensure patient is not allergic to penicillins or cephalosporins. -Follow IV administration directions (i.e, drug reconstitution, dilution). Patient teaching: -Instruct patient to report any discomfort at the I.V. insertion site. Nursing Consideration: -Monitor for any signs and symptoms of superinfection.
- 2. 2 Generic name: ciprofloxacin Trade name: Cipro Respiratory tract infection Antibiotic (fluoroquinolones) Dosage: 500 mg, P.O. daily Normal range: 500 mg, P.O. every 12 hours No, not within normal range due to longer dosing interval. Rationale: “Start low and go slow” guidelines. Mr. MP is an elderly patient and age-related changes such as longer metabolism and excretion time is likely. Adverse Effects: Hematologic: thrombocytopenia Musculoskeletal: tendon rupture Skin: Stevens-Johnson syndrome Black Box Warning: -Drug associated with increased risk of tendinitis and tendon rupture, especially in patients older than age 60. (Mr. MP is 76) -Instruct patient to notify prescriber if he experiences pain or inflammation. Drug-Food interaction: Caffeine -Warn patient that caffeine’s effects will increase when taken with this drug. -Monitor patient closely, especially heart rate. Administration: -Before administering first dose, obtain specimen for culture and sensitivity tests. -Administer drug with fluids to reduce risk of urine crystals.
- 3. 3 Generic name: fluticasone propionate- salmeterol inhalation powder Trade name: Advair diskus Reasonfor use: To reduce exacerbations of COPD in patients with a history of exacerbations Common class: Corticosteroid (long-acting beta2-adrenergic agonist) Dosage: 250/50 – 2 puffs, Bid Normal Range: 1 inhalation of 250/50 only, b.i.d., about 12 hours apart. Yes, within normal range, however should specify instruction of 1 inhalation about 12 hours apart. Adverse Effects: Respiratory: lower respiratory tract infection, pneumonia Cardiovascular: palpitations Other: viral or bacterial infections Nursing consideration:. -If Mr. MP has taken this drug longer than 6 months, he should be evaluated to assess the therapy’s risks or benefits. Administration: -Remind patient to do 1 inhalation of the Advair Diskus 250/50 b.i.d, and about 12 hours apart. Patient Teaching: Instruct patient to report any symptoms of palpitations, chest pain, rapid heart rate, tremor or nervousness Albuterol inhaler Generic name: albuterol sulfate Trade name: AccuNeb, Proventil-HFA Reasonfor use: To prevent or treat bronchospasm in patients with reversible obstructive airway disease. Common class: Bronchodilator Dosage: 2 puffs q2hrs prn for wheezing (call if needed > twice in 8 hrs) Normal Range: 1-2 inhalations every 4 to 6 hours prn Not within normal range. Mr. MP’s dosage Adverse Effects: CV: tachycardia, hypertension Metabolic: hypokalemia Respiratory: bronchospasm Administration: -Shake inhaler before using. -Wait at least 2 minutes between inhalations. Patient Teaching: -Teach patient and have patient demonstrate back the correct use of albuterol inhaler. -Warn patient about risk for paradoxical bronchospasm and to stop drug immediately if it
- 4. 4 interval is shorter compared to the recommended. The rationale might be due to the severity or duration of having COPD. In addition, adjust-a-dose is stated for elderly patients to have 2 m.g. P.O. t.i.d or q.i.d. as oral tablets or syrup. occurs. Generic name: omeprazole Trade name: Prilosec Reasonfor use: Symptomatic gastroesophageal reflux disease (GERD) Common class: Proton pump inhibitor (PPI) Dosage: 20 mg capsule, P.O. daily Normal Range: 20 mg capsule , P.O. daily Yes, within range Adverse Effects: CNS: asthenia, dizziness Respiratory: upper respiratory tract infection Nursing considerations: -Chronic use of this drug may cause low magnesium levels. -Monitor patient for signs and symptoms of hypomagnesemia (i.e, abnormal heart rate or rhythm, muscle spasms) -Teach patient how to recognize these manifestations and report them to his health care provider.
- 5. 5 Administration: -Don’t crush tablets or capsules. -Give drug at least 1 hour before meals. Generic name: amlodipine and valsartan Trade name: Exforge Reasonfor use: Hypertension Common class: Amlodipine – Calcium channel blockers Valsartan – Angiotensin II receptor antagonist Dosage: Amlodipine 10 mg/ valsartan 160 mg 1 tablet P.O. every a.m. Normal Range: Amlodipine 5-10 mg / valsartan 160 – 320 mg P.O. once daily Yes, within normal range Adverse Effects: Amlodipine CNS: dizziness CV: palpitations Valsartan Respiratory: upper respiratory tract infection Amlodipine Nursing Considerations: Alert: Monitor patient carefully. Some patients have developed increased frequency, duration or severity of angina. Patient teaching: -Inform patient that S.L. nitroglycerin can be taken as needed when angina symptoms are acute. Valsartan Nursing Considerations: -Correct sodium and volume depletions before starting drug. -Monitor BUN and creatinine levels due to their chance of increasing with this drug.
- 6. 6 Generic name: theophylline Trade name: Theo-24 Reasonfor use: Chronic bronchospasm using extended- release preparations Common class: Bronchodilator (Xanthine derivatives) Dosage: 300 mg P.O. capsule, daily Normal Range: Maximum 400 mg P.O. daily in divided doses every 8 to 12 hours Yes, within normal range Adverse Effects: CV: sinus tachycardia, arrhythmias Respiratory: respiratory arrest Administration: -Give drug around-the-clock, using extended-release product at bedtime. Nursing Considerations: -Dosages may need to be increased in cigarette smokers because drug is metabolized faster. -If Mr. MP decides to quit, tell him to inform his prescriber. Dosage reduction may be needed to prevent toxicity. Caution: -Use cautiously in elderly patients and those with COPD, cardiac failure, hypertension angina and impaired circulatory function. Generic name: dabigatran etexilate mesylate Trade name: Pradaxa Reasonfor use: To reduce the risk of stroke and systemic embolism in patients with non-valvular atrial fibrillation. Common class: Anticoagulant Dosage: 150 mg P.O., twice daily Normal Range: 150 mg P.O., twice daily Yes, within normal range Adverse Effects: GI: hemorrhagic erosive gastritis, gastric and GI bleeding Hematologic: life- threatening bleeding Patient Teaching: -Instruct patient to report bleeding when brushing teeth or shaving; blood in vomit, urine or stool; nosebleeds. -Inform patient that regular blood tests will be required to monitor drug’s effects. -Inform patient to tell all of his health care providers he is taking
- 7. 7 this drug. Generic name: acetaminophen Trade name: Aspirin, Tylenol Reasonfor use: Mild pain Common class: Analgesic Dosage: 325 mg, 1 to 2 tablets every 4 hours prn for pain or fever Normal Range: 325 to 650 mg P.O., every 4-6 hours. Yes, within normal range Adverse Effects: CV: hypertension Respiratory: abnormal breath sounds Patient Teaching: -Inform patient that drinking alcohol while taking acetaminophen increases risk of liver damage. Alert: -Many OTC and prescription products have acetaminophen. When determining the total daily dose of acetaminophen, be alert of this. -Maximum daily dose is 4 g daily.
- 8. 8 PART 2: CLIENT PROBLEMS, ASSESSMENTS, and COLLABORATION (14 points) List 3 important problems/issues/concerns caused by Mr. MP’s medications and 1 intervention for each problem/issue/concern. Note: Identify 3 problems and 3 interventions total – not for each medication. Include the medication(s) that each problem is related to. List the 3 problems that you (the RN) are most concerned about. No more than 1 intervention can involve teaching the client. (6 points) 1. Risk for bleeding related to medication’s adverse effects of bleeding complications Nursing Intervention: For injections or venous punctures, the needle with the smallest gauge possible should be used to prevent bleeding. o In addition, after needle is removed, apply gentle and prolonged pressure to the area that was punctured. Patient teaching: o Inform patient to use caution in activities that may cause bleeding. Brushing teeth: patient should use soft bristles. Sneezing: avoid blowing nose forcefully Bowel movements: avoid straining Shaving: avoid using a straight-edge razor RelatedMedications: Dabigatran etexilate mesylate (Pradaxa): Adverse effects: Hemorrhagic erosive gastritis, gastric and GI bleeding, and life-threatening bleeding. Ciprofloxacin (Cipro) Adverse effect: Thrombocytopenia
- 9. 9 2. Risk for infection related to medication’s adverse effects of upper and lower respiratory infections, and leukopenia. Nursing Interventions: o Encourage patient to cough and deep breathe. o Wash hands before contact with patient and between procedures with patient. In addition, inform patient and visitors to wash hands as well. RelatedMedications: Fluticasone propionate salmeterol (Advair diskus) Adverse effects: Lower respiratory tract infection and pneumonia Omeprazole (Prilosec) Adverse effect: Upper respiratory tract infection Ceftriaxone (Rocephin) Adverse effect: Leukopenia Valsartan Adverse effect: Upper respiratory tract infection
- 10. 10 3. Risk for falls related to medication’s adverse effects of tendon rupture, dizziness and asthenia. Nursing Interventions: Implement measures and educate patient to prevent falls. Keep patient’s bed in lowest position. Instruct patient to rise from positions (i.e, sitting or supine) slowly. Instruct patient to wear non-slip socks or shoes when ambulating. RelatedMedications: Ciprofloxacin (Cipro) Adverse effect: Tendon rupture Omeprazole (Prilosec) Adverse effect: Asthenia and dizziness Amlodipine (Exforge) Adverse effect: Dizziness Valsarta Adverse effect: Dizziness, fatigue, orthostatic hypotension, syncope.
- 11. 11 List 3 important assessments you will perform to identify potential side effects/adverse effects from Mr. MP’s medications. Include the medication(s) that is related to each assessment. (3 points) 1. Respiratory assessment. -Assess breathing pattern (i.e., regular or irregular), breathing rate, and use of accessory muscles. -Auscultate lung sounds. -In addition, compare the new assessment findings to findings from patient’s history. RelatedMedications: Fluticasone propionate salmeterol (Advair diskus) Adverse effects: Lower respiratory tract infection and pneumonia Omeprazole (Prilosec) Adverse effect: Upper respiratory tract infection Acetaminophen Adverse effect: Abnormal breath sounds. Theophylline Adverse effect: Respiratory arrest. 2. Cardiovascular assessment. -Monitor patient’s blood pressure and heart rate. -Palpate Mr. MP’s peripheral pulse sites (i.e., carotid, radial, apical, pedal pulses) -Assess skin color and temperature. RelatedMedications: Acetaminophen
- 12. 12 Adverse effect: Hypertension Dabigatran (Pradaxa) Adverse effect: Gastric, GI bleeding, hemorrhagic erosive gastritis Theophylline Adverse effect: sinus tachycardia, arrhythmias 3. Musculoskeletal assessment. -Assess patient’s gait and balance. -Ask Mr. MP if he is experiencing any feelings of weakness when ambulating. RelatedMedications: Ciprofloxacin (Cipro) Adverse effect: Tendon rupture Omeprazole (Prilosec) Adverse effect: Asthenia and dizziness Amlodipine (Exforge) Adverse effect: Dizziness Valsartan Adverse effect: Orthostatic hypotension, dizziness, syncope, arthralgia
- 13. 13 Identify at least 5 of the healthcare providers that you will collaborate with in administering medications to Mr. MP. Describe in a minimum of 150 words what that collaboration will involve. (5 points – in order to maximize points earned, be sure to describe rather than to simply list the disciplines involved and be sure to focus on collaboration related to medications) Note: Only 1 of the 5 healthcare providers can be a physician, NP, or PA. Physician – It is important to have good collaboration with the physician regarding Mr. MP’s medications and whether he’s improving or not improving (i.e., blood pressure, respiratory function). In addition, if any new pertinent information arises. For example, if Mr. MP suddenly states he thinks he may have an allergic reaction to penicillin. I would hold his order of Rocephin due to its contraindication for penicillin allergies. Then, I would notify his physician about this newly found information, and he/she would determine what changes should be done regarding his Rocephin. Respiratory therapist - A collaboration with the respiratory therapist is crucial for Mr. MP’s care. If I found during my physical assessment of Mr. MP that his respiratory function has been worsening (i.e, abnormal breath sounds or shortness of breath), I would report this to his respiratory therapist. The deterioration of his respiratory function may be due to medications or the need for a higher dosage. Nevertheless, this is all vital information to provide to his respiratory therapist because he/she can do further re-evaluation and make adjustments to Mr. MP’s drug therapy and treatment. Pharmacist – If a situation arises where I am unsure of Mr. MP’s medications and their orders, I would contact the pharmacist. For instance, I was unsure of his prescription of the albuterol inhaler. When I looked into the drug book, Mr. MP’s dosage interval was shorter than the recommended. In addition, there was an adjust-a-dose statement for elderly patients to use the form of tablets or syrup. Therefore, I would contact the pharmacist of this concern.
- 14. 14 Physical therapist – The collaboration between the nurse and the physical therapist regarding medications can involve Mr. MP’s walking ability. I think this is an issue to address because it was reported that Mr. MP fell twice the last month due to ‘loss of balance’. If it appears to the nurse that the medications are putting him at risk for falling (i.e., experiencing dizziness, weakness), then, the nurse should communicate this with the physical therapist. That way the physical therapist can be aware of it and overcome it when working with the patient and planning their therapy. Occupational therapist – The collaboration with the occupational therapist may involve how Mr. MP can manage any adverse effects he’s experiencing from his medications and still perform the activities of daily living. For instance, it was reported in his history that he fell twice in the past month. In addition, some of his medications put him at risk for falling again in the future. The nurse can address this issue with the occupational therapist, so he/she can plan therapy for Mr. MP to prevent this from happening again. In addition, the fact that Mr. MP does not reportedly use a device to help him walk. The nurse can communicate this with the occupational therapist who may make suggestions to Mr. MP of the appropriate devices he can use.
- 15. 15 PART 3: ADDITIONAL QUESTIONS (10 points) Part 3: Additional Questions (10 points) 1. Mr. MP’s ceftriaxone (1 gram) is diluted in 50 mL of fluid. If it is to be infused over 30 minutes, what rate (in mL/hr) will be set on the pump? 50mL x 60 mins _____________ Hour x 30 mins Answer: 100 mL/hr 2. Mr. MP has a prn prescription for acetaminophen. How many tablets can he receive in one day without exceeding the maximum daily dosage for this drug? Prescription: 325 mg (1-2 tablets every 4 hours prn) Maximum daily dosage: 4,000 mg/day 4,000 mg / 325 mg = 12.3 Answer: Up to 12 tablets (3,900 mg total) Mr. MP can receive in one day without exceeding maximum daily dosage (4,000 mg)
- 16. 16 3. Mr. MP arrived from the ED without an infusion pump on his IV fluids (D5 .45NS with 20 mEq/L KCL). If the tubing pictured above is available, how many drops/minute will be required to maintain the infusion at the ordered rate? Round your answer to the nearest whole number. Gtt/min = (15 gtt/mL) (50mL/hr) (hr/60 mins) = Gtt/min = 750/60 = 12.5 Answer =13 gtt/min required to maintain the ordered infusion rate. 4. Mr. MP has medications that are controlled-release or sustained release preparations. Briefly describe the nursing implications for the administration of any controlled-release or sustained release medications. The nursing implications for controlled or sustained-release preparations are to not crush these tablets. The reason to not crush these medications is because their therapeutic effect will be lost if these are crushed. The purpose of these medications is to be dissolved over a period of time and maintain a constant drug concentration level within the patient.
- 17. 17 5. Mr. MP reports an allergy to morphine. What action(s) would you take if Mr. MP had a prescription for an opioid during this hospitalization? According to Fraser Health, if an allergy of morphine exists, there are other opioids available that will lower the chance of an allergic reaction re-occurring compared to the morphine. For instance, these other opioids can be semi-synthetic (i.e, oxycodone) or synthetic (i.e., fentanyl or methadone). However, caution should still be taken when administering these. The action I would take though is to look up this specific type of opioid in my drug book. I would check to see if there are any contraindications if patient is allergic to morphine. If I am still hesitant though, I would contact the physician and let him know my concerns of administering this drug. 6. Review Mr. MP’s theophylline level. What is the most likely cause of this level? What action(s) might be indicated? Mr. MP’s theophylline level and normal range: o Mr. MP’s theophylline level is 0.7, which is considered low. The normal range of theophylline is 10-20 mcg/mL. Causes: o The causes for low theophylline level are obesity, a diet high in carbohydrate and protein, cigarette smoking, and increased age. Most likely cause: o The most likely cause for Mr. MP’s low theophylline level is his chronic habit of smoking. Smoking quickens the excretion of theophylline. o Mr. MP did report that he has smoked 1 ½ packs of cigarettes/day x 60 years and has never successfully quit. Indicated actions: o Educate Mr. MP the factors that contribute to low theophylline level (i.e, obesity, diet high in carbohydrate and protein). Especially inform Mr. MP that smoking is a risk factor. Inform Mr. MP what foods are low in carbohydrate and protein. o Due to Mr. MP’s history of smoking, it should be strongly recommended for him to make plans of quitting.
- 18. 18 Inform him of helpful ways to quit and suggest local support groups available. o Ensure he is taking his theophylline medications as prescribed, and understands his dosage, why he is taking it, and the adverse effects. 7. Mr. MP is a long-time smoker. What intervention(s) would be appropriate for him during this hospitalization? Appropriate interventions would be to use therapeutic communication and educate him about the risks he’s taking by not quitting, and provide referrals for extra support. Therapeutic Communication o It’s important to use therapeutic communication in order to understand what has prevented him from successfully quitting in the past. Then once these barriers are identified, collaborate solutions and make a plan to overcome these barriers. o In addition, it is also important to provide support and encouragement for him to make plans of quitting. Questions should be asked to assess whether Mr. MP does have social support (i.e., friends and family) to help him quit. Patient Teaching o Not only informing him the risks of continuing to smoke, but also inform him the benefits (i.e, short-term and long-term) if he does. o Provide him an informational handout on discharge to remind him the reasons to quit and how he can quit. o Bring up the option of nicotine replacement therapy (i.e, nicotine gum, nicotine patch). Referrals o Provide Mr. MP with local support groups or programs specific to help those quit smoking.
- 19. 19 8. Nipride (50 mg in 250 mL of D5W) is prescribed at 3 mcg/kg/min for a client who weighs 82 kg. What is the infusion rate (in mL/hr)? Round to the nearest whole number. mL/hr = (250 mL) / (3 mcg / kg x min) (82 kg) (60 min/hr) (0.001 mg/mcg) (1/50mg) = 73.8 Answer= 74 mL/hr 9. Epinephrine (10 mg/500 mL) is prescribed at 0.3 mcg/kg/min for a client who weighs 15.5 kg. What is the infusion rate (in mL/hr)? Round to the nearest whole number. mL/hr = (500mL/10mg) (0.3 mcg / kg x min) (15.5 kg) (60 min/hr) (0.001 mg/ mcg) mL/hr = 13.95 Answer= 14 mL/hr 10. Norepinephrine (1 mg/250 mL) is prescribed at 3 mcg/min for a client who weighs 209 pounds. What is the infusion rate (in mL/hr)? Round to the nearest whole number. mL/hr = (250 mL/mg) (3 mcg/min) (60 min/hr) (0.001 mg/mcg) Answer = 45 mL/hr
- 20. 20 PART 4: REFLECTION (5 points) In 1 to 2 paragraphs (a minimum of 150 words), reflect on what you learned from this case study, as well as what you need to continue to work on. In this second case study I feel like I learned how to do each section more efficiently than last time. I feel like the first case study it took me a while to find everything I needed to find. This time it was a lot easier to find information and I had more confidence that it would be accurate. In the last case study I had some points taken off for not answering what the question was asking directly. For example, in the part that asks about the collaboration with other healthcare providers, I didn’t focus it on the patient’s medications. For this case study I made sure to not make the same mistake and focused it on the patient’s medications. Overall, I think I made an improvement compared to the first case study. I felt a little overwhelmed with the first case study, but I had more confidence and used my time more wisely for this one. For the future I think I will need to continue to work on managing my time with the case study. I did the majority of the case study after spring break, and it would have been better if I did it during spring break.
- 21. 21 LIST OF ALL REFERENCES USED Cengage Learning. (2010). Nursing considerations for nursing process: Implementation of the administration of medications by different routes. Retrieved from http://www.cengagesites.com/academic/assets/sites/5407/pdf/drug-admin/section5.pdf Elsevier. (2012). Nursing diagnosis. Retrieved from http://www1.us.elsevierhealth.com Fraser Health. (2006). Principles of opioid management. Retrieved from http://www.fraserhealth.ca/media/16FHSymptomGuidelinesOpioid.pdf National Institutes of Health. (1993). Nurses: Help your patients stop smoking. Retrieved from http://www.nhlbi.nih.gov/health/prof/lung/other/nurssmok.txt University of Cincinnati. (2000). Prescription medication in the elderly. Retrieved from http://www.netwellness.org/healthtopics/aging/faq16.cfm Vanderbilt University Medical Center (2014). Serum theophylline level. Retrieved from http://www.mc.vanderbilt.edu/diglib/consumerhealth/labs/49/150431.htm