The role of innovation in augmenting healthcare - the ColaLife Story
- 1. The role of innovation in augmenting Healthcare – the ColaLife Story Simon Berry Co-founder & CEO, ColaLife simon@colalife.org
- 2. What is ColaLife? ColaLife is a charity registered in the UK Charity number: 1142516 ─ Two full-time workers and one part-time ─ Six voluntary trustees on our board ─ Focus on saving children’s lives ─ Independent ─ Our fieldwork was carried out in Zambia but we are now working to have a global impact We have no commercial interest in the products described in this presentation
- 3. Rohit Ramchandani Jane Berry Simon Berry The Team.
- 4. What do we mean by innovation? Innovation is: Something new or different that delivers value to the world, with the key criteria that you’re not innovating if you’re not improving people’s lives. So: it is not about technology (but it might be). it is more than just a clever idea.
- 5. Why do we need innovation? The Past The Future
- 6. Why do we need innovation? The Past The Future
- 7. Why do we need innovation? The Past The Future
- 8. Why do we need innovation? The Past The Future
- 9. Why do we need innovation? The Past The Future
- 10. Why do we need innovation? The Past The Future Innovation
- 11. the problem
- 13. Diarrhoea 8%of deaths Malaria 5%of deaths AIDS 1% Source: UNICEF (2017) Levels and trends in child mortality. Estimates developed by the UN Inter-agency Group for Child Mortality Estimation. Measles 1% The second biggest infectious killer is diarrhoea.
- 15. The 15-year-old recommended treatment that only 7% of children get. ORS and Zinc
- 18. Remote rural retail shop, Kalomo District, Zambia Drug store room, Tiriri Health Centre, Katine, Uganda Medicines don’t
- 20. What we learnt Litre ORS sachets are too big Measuring water was an issue Willingness to pay Preferred branding Finding out what people want.
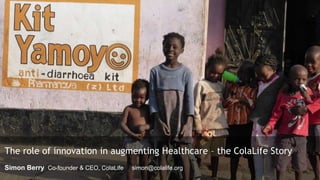
- 21. Kit Yamoyo brand, design & benefits.
- 22. Kit Yamoyo brand, design & benefits. Kit Yamoyo • Attractive
- 23. Kit Yamoyo brand, design & benefits. Kit Yamoyo • Attractive • ORS sachets are 200ml
- 24. Kit Yamoyo brand, design & benefits. Kit Yamoyo • Attractive • ORS sachets are 200ml • Packaging is also: ─ A measuring device for the water
- 25. Kit Yamoyo brand, design & benefits. Kit Yamoyo • Attractive • ORS sachets are 200ml • Packaging is also: ─ A measuring device for the water ─ A mixing device
- 26. Kit Yamoyo brand, design & benefits. Kit Yamoyo • Attractive • ORS sachets are 200ml • Packaging is also: ─ A measuring device for the water ─ A mixing device ─ A storage device (the soap tray is a lid) ─ A cup
- 27. our approach
- 28. Everything we do must be self-sustaining… We cannot become a permanent part of the solution Everything is done through local organisations/processes We therefore work through partnerships These must be *smart* partnerships Our approach.
- 30. Smart partnerships (we are the strings).
- 31. the trial (establishing the evidence base)
- 32. 60% Only 60% of carers mixed ORS correctly when given conventional litre sachets. 0 Suppliers sold ORS or Zinc in the private sector. <1% of children received the correct treatment for diarrhoea – ORS & Zinc 7.3km Average distance to ORS at clinics (1 L sachet only, no Zinc). September 2012 Before Kit Yamoyo. Rural, remote areas. Before Trial results.
- 33. 60% Only 60% of carers mixed ORS correctly when given conventional litre sachets. 0 Suppliers sold ORS or Zinc in the private sector. <1% of children received the correct treatment for diarrhoea – ORS & Zinc 7.3km Average distance to ORS at clinics (1 L sachet only, no Zinc). August 2013 After 12 months’ trial of new Kit Yamoyo design & distribution through existing private sector channels. September 2012 Before Kit Yamoyo. Rural, remote areas. Before After Trial results.
- 34. 60% Only 60% of carers mixed ORS correctly when given conventional litre sachets. 0 Suppliers sold ORS or Zinc in the private sector. <1% of children received the correct treatment for diarrhoea – ORS & Zinc 7.3km Average distance to ORS at clinics (1 L sachet only, no Zinc). >26k Kit Yamoyos sold into 2 remote rural areas in 1 year via existing market channels. August 2013 After 12 months’ trial of new Kit Yamoyo design & distribution through existing private sector channels. September 2012 Before Kit Yamoyo. Rural, remote areas. Before After Trial results.
- 35. 60% Only 60% of carers mixed ORS correctly when given conventional litre sachets. 0 Suppliers sold ORS or Zinc in the private sector. <1% of children received the correct treatment for diarrhoea – ORS & Zinc 7.3km Average distance to ORS at clinics (1 L sachet only, no Zinc). >26k Kit Yamoyos sold into 2 remote rural areas in 1 year via existing market channels. 45% of children in trial areas received ORS/Zinc. Up from a baseline of <1%. August 2013 After 12 months’ trial of new Kit Yamoyo design & distribution through existing private sector channels. September 2012 Before Kit Yamoyo. Rural, remote areas. Before After Trial results.
- 36. 60% Only 60% of carers mixed ORS correctly when given conventional litre sachets. 0 Suppliers sold ORS or Zinc in the private sector. <1% of children received the correct treatment for diarrhoea – ORS & Zinc 7.3km Average distance to ORS at clinics (1 L sachet only, no Zinc). >26k Kit Yamoyos sold into 2 remote rural areas in 1 year via existing market channels. 45% of children in trial areas received ORS/Zinc. Up from a baseline of <1%. 2.4km Distance to ORS/Zinc in the trial areas was reduced by two- thirds from 7.3km to 2.4km. August 2013 After 12 months’ trial of new Kit Yamoyo design & distribution through existing private sector channels. September 2012 Before Kit Yamoyo. Rural, remote areas. Before After Trial results.
- 37. 60% Only 60% of carers mixed ORS correctly when given conventional litre sachets. 0 Suppliers sold ORS or Zinc in the private sector. <1% of children received the correct treatment for diarrhoea – ORS & Zinc 7.3km Average distance to ORS at clinics (1 L sachet only, no Zinc). >26k Kit Yamoyos sold into 2 remote rural areas in 1 year via existing market channels. 45% of children in trial areas received ORS/Zinc. Up from a baseline of <1%. 2.4km Distance to ORS/Zinc in the trial areas was reduced by two- thirds from 7.3km to 2.4km. 93% of Kit Yamoyo users mixed ORS correctly, due to appropriate 200ml sachets and the kit’s measuring function. August 2013 After 12 months’ trial of new Kit Yamoyo design & distribution through existing private sector channels. September 2012 Before Kit Yamoyo. Rural, remote areas. Before After Trial results.
- 38. The vision.
- 41. The awards: trophies not millstones; kudos not baggage.
- 42. “The main thing is to keep the main thing the main thing” Stephen Covey
- 44. ORS Reduce number of sachets to 4 This may also enhance adherence to the combined therapy Zinc Produce locally Design the blister pack to enhance adherence to the 10- day regime Blister pack needs no box Soap Produce locally Leaflet Simplify – single fold. Same leaflet for all formats Packaging Remove constraint of fitting in Coca- Cola crate Produce locally Produce re-fill option Incorporating the learning into the scale-up.
- 45. The screw-top and the flexi-pack
- 46. The Kit Yamoyo bag can be used to measure the correct amount of water.
- 52. 0 100,000 200,000 300,000 400,000 500,000 600,000 700,000 800,000 2012-13 2014-15 2016-17 2018-19 Ex-factory sales - all formats Commercial ex-factory sales – Oct-12 to Sep-19 To Sep-19 Ex-factory sales – commercial formats
- 53. The Government ORS/Zinc co-pack
- 54. 0 100,000 200,000 300,000 400,000 500,000 600,000 700,000 800,000 2012-13 2014-15 2016-17 2018-19 Ex-factory sales - all formats Total ex-factory sales – Oct-12 to Sep-19 To Sep-19 Ex-factory sales – all formats
- 55. 0 100,000 200,000 300,000 400,000 500,000 600,000 700,000 800,000 2012-13 2014-15 2016-17 2018-19 Ex-factory sales - all formats Total ex-factory sales – Oct-12 to Sep-19 To Sep-19 To Dec-19 (projected) 0% 77% 86% 94% Ex-factory sales – all formats
- 56. Co-packaged ORS and Zinc added to the NEML
- 57. going global
- 58. Moving to the mainstream for global impact
- 59. key lessons
- 60. Foster innovation Move to the mainstream Fail fast, learn and move on Focus on want not need It’s not just what you do, it’s the way that you do it Key Lessons. Have a clear vision
- 61. Isenberg Family Charitable Foundation Norr Thank you to the ColaLife funders past and present.
Hinweis der Redaktion
- Hello everyone. Thank you very much for inviting me. It is a great honour to be here. I’ve been asked to talk about the role of innovation in improving healthcare and what we must do to ensure innovations have an impact. To do this I will be drawing heavily on ColaLife’s experience in improving access to co-packaged ORS and Zinc for the treatment of diarrhoea in Zambia. I will be highlighting the lessons we have learnt that I think will be helpful for anyone innovating in the healthcare sector.
- Let me start by telling what ColaLife is. ColaLife is a charity registered in the UK Charity number: 1142516 Two full-time workers and one part-time Six voluntary trustees Focus on saving children’s lives Independent Our fieldwork was carried out in Zambia but we are now working to have a global impact We have no commercial interest in the products described in this presentation
- This is the team. Jane works with me full-time. She is my partner in life and ColaLife. Rohit is based in Canada and works with us part-time. He is our public health adviser and monitoring and evaluation expert.
- So what is innovation? If you ask 10 innovation experts what they mean by innovation you are likely to get 10 different definitions. This is the definition I work to. Innovation is something new or different that delivers value to the world, with the key criteria that you’re not innovating if you’re not improving people’s lives. So innovation is not about technology. Just because you are using a mobile phone to do something doesn’t in itself make what you are doing innovative. You need to be improving people’s lives. Similarly, an idea may be innovative but it is not innovation until it is put into practice and improves people's lives.
- So why do we need innovation? Why is it important? Let me use under 5 child mortality as an example. In the UK we have a low child mortality rate and it is also declining…
- and if we project into the future, by 2050 child mortality rates will be very small indeed.
- Mortality rates in sub-Saharan Africa are a lot higher but are also declining. But you will note the massive inequality.
- If we project this decline into the future you can see that child mortality in sub-Saharan Africa will still be many times higher than in the UK right now. It will probably take at least 100 years for comparable survival rates to be achieved. But that assumes ‘Business as Usual’ or carrying on doing things we are doing now.
- However, innovation is by definition NOT ‘business as usual’. Innovation can cause a step-change in the progress made.
- This is why we need innovation – particularly in the health sector – so that we can remove the inequalities in health that exist across the world today. We need innovation in the healthcare sector because ‘Business as usual’ is not enough to stop growing health inequalities.
- Let’s bring this innovation theory to life by looking at innovation in practice. In 2008, ColaLife started to try and help solve the problem of high child mortality in sub-Saharan Africa.
- Child mortality is unacceptably high in developing countries. 1 in 13 children don’t make it to their 5th birthday.
- Just as shocking as this level of mortality is the fact that diarrhoea, an easily treated condition, is the second biggest killer. Dehydration from diarrhoea kills more children as Malaria, HIV/AIDS and Measles combined. Although diarrhoea is easily treatable with very simple medicines people don’t have easy access to them.
- But it is not just about mortality. In sub-Saharan Africa 40% of children are stunted which means they are smaller than they should be for their age. Diarrhoea is a key factor in stunting. If a child is stunted at the age of 2 there will be permanent effects on both physical and mental development. They will never reach their full potential.
- But we have known how to treat diarrhoea for more than 3 decades and the latest global recommendation – ORS with Zinc - is 15 years old. Both are cheap to produce and stable at ambient temperatures. The trouble is only 7% of children get this treatment. If all children with diarrhoea received zinc and ORS promptly, over 90% of these deaths could be prevented. So diarrhoea mortality is a problem of ACCESS to the known, effective treatment.
- This brings me to the idea…
- Coke gets everywhere. But whilst you can buy Coke, and many other commodities, in the remotest parts of the world, you cannot get ORS and Zinc to treat a child with diarrhoea.
- While small community shops are well stocked with the things people want, the public sector struggles to keep public health centres stocked with essential medicines like ORS and Zinc. The last remaining barrier to children getting the treatment we know works, and saves their lives, is ACCESS.
- And so our idea was born. Why don’t we put diarrhoea treatment kits in Coca-Cola crates? The logic was simple: Coke gets everywhere. So, if we put diarrhoea kits in the same crates, they would get there too
- The process of designing the anti-diarrhoea kit started here. We spoke to eight groups of caregivers about the challenges they faced treating diarrhoea in the home and we learnt so much. Firstly, litre sachets of ORS are too big for use in the home. ORS comes as a powder that needs to be mixed with safe water. Once mixed up it should be used as soon as possible and any solution still left after 24 hours needs to be thrown away as it gets contaminated. But a child will only drink about 400ml in 24 hours. So if you follow the instructions correctly you will throw away more ORS than you give to your child. Litre sachets of ORS were never designed for the home treatment of diarrhoea. They were designed for use in institutions – hospitals and clinics.. If you have five children lined up with diarrhoea it makes sense to make up ORS by the litre. The situation in the home where you are treating just one child is completely different and a litre is too much to mix up at one time. Measuring water is also a problem, in our trial only 60% of caregivers got this right. Caregivers resource-poor settings rarely have a litre measure and most will not know what a litre is. == These focus groups also gave us an indication of what caregivers would be prepared to pay for a diarrhoea treatment kit and the caregivers gave us their views on various naming and branding options.
- Kit Yamoyo Attractive
- ORS sachets are 200ml
- Packaging is also: A measuring device for the water
- Packaging is also: A measuring device for the water A mixing device
- Packaging is also: A measuring device for the water A mixing device A storage device (the soap tray is a lid) A cup As well as ORS, the kit contained Zinc supplements and so delivered the 12 year old international standard for diarrhoea treatment: ORS combined with Zinc. The kit also contained soap to help ensure handwashing.
- Before I go on to tell you what we did next, I’d like to tell you a little bit about the way we do things.
- The foundation of our approach is that everything we do must be ultimately self-sustaining and this defines everything else. It means that ColaLife cannot become a permanent part of the solution. This in turn means that we have to do everything through local organisations and processes. So we have to work through partnerships. But partnerships come with a health warning. They cannot be any old partnership they must be “smart” partnerships.
- In our case, we know that all the organisations that are needed to transform access to affordable diarrhoea treatment already exist in most countries: The policy makers The regulators The manufacturers The distributors The wholesalers The retailers The doctors, nurses and community health workers The marketeers And so on The task then, is NOT to set up parallel systems to do what these organisations are there to do, but to transform the way they operate together.
- We start by establishing what we call a “smart partnership”. Our role is to bring these players together around a shared vision NOT around ColaLife. When this job is done then ColaLife can withdraw and leave a sustainable, transformed local system behind. When we leave, we don’t want to leave with a bang, or with whimper. We don’t want anyone to notice that we’ve gone.
- Back to the story. Once we had designed our anti-diarrhoea kit - called Kit Yamoyo – we tested its distribution through the same channels used by Coca-Cola.
- The results were impressive. From a standing start, in 12 months, more that 26,000 kits were bought by retailers serving these communities. Our baseline showed that ORS or Zinc was not available through the private sector before we started. Treatment rates with ORS and Zinc rose from virtually zero to 45%. We reduced caregivers’ need to travel to access ORS by two thirds; from 7.3km to 2.4km because ORS and Zinc was available in community shops which are more numerous and therefore closer to people’s homes. And finally, we increased the accuracy with which caregivers mixed the ORS due to the measuring functionality built into the packaging.
- The results were impressive. From a standing start, in 12 months, more that 26,000 kits were bought by retailers serving these communities. Our baseline showed that ORS or Zinc was not available through the private sector before we started. Treatment rates with ORS and Zinc rose from virtually zero to 45%. We reduced caregivers’ need to travel to access ORS by two thirds; from 7.3km to 2.4km because ORS and Zinc was available in community shops which are more numerous and therefore closer to people’s homes. And finally, we increased the accuracy with which caregivers mixed the ORS due to the measuring functionality built into the packaging.
- The results were impressive. From a standing start, in 12 months, more that 26,000 kits were bought by retailers serving these communities. Our baseline showed that ORS or Zinc was not available through the private sector before we started. Treatment rates with ORS and Zinc rose from virtually zero to 45%. We reduced caregivers’ need to travel to access ORS by two thirds; from 7.3km to 2.4km because ORS and Zinc was available in community shops which are more numerous and therefore closer to people’s homes. And finally, we increased the accuracy with which caregivers mixed the ORS due to the measuring functionality built into the packaging.
- The results were impressive. From a standing start, in 12 months, more that 26,000 kits were bought by retailers serving these communities. Our baseline showed that ORS or Zinc was not available through the private sector before we started. Treatment rates with ORS and Zinc rose from virtually zero to 45%. We reduced caregivers’ need to travel to access ORS by two thirds; from 7.3km to 2.4km because ORS and Zinc was available in community shops which are more numerous and therefore closer to people’s homes. And finally, we increased the accuracy with which caregivers mixed the ORS due to the measuring functionality built into the packaging.
- The results were impressive. From a standing start, in 12 months, more that 26,000 kits were bought by retailers serving these communities. Our baseline showed that ORS or Zinc was not available through the private sector before we started. Treatment rates with ORS and Zinc rose from virtually zero to 45%. We reduced caregivers’ need to travel to access ORS by two thirds; from 7.3km to 2.4km because ORS and Zinc was available in community shops which are more numerous and therefore closer to people’s homes. And finally, we increased the accuracy with which caregivers mixed the ORS due to the measuring functionality built into the packaging.
- The results were impressive. From a standing start, in 12 months, more that 26,000 kits were bought by retailers serving these communities. Our baseline showed that ORS or Zinc was not available through the private sector before we started. Treatment rates with ORS and Zinc rose from virtually zero to 45%. We reduced caregivers’ need to travel to access ORS by two thirds; from 7.3km to 2.4km because ORS and Zinc was available in community shops which are more numerous and therefore closer to people’s homes. And finally, we increased the accuracy with which caregivers mixed the ORS due to the measuring functionality built into the packaging.
- However, our idea of transporting kits in crates did not work. What we thought was THE innovation was not the innovation at all. Less than 4% of retailers put the kits in Coca-Cola crates.
- In practice, this is what happened. Retailers strapped Kit Yamoyo to the back of their bicycle along with everything else. It wasn’t the space in the crates that was important, it was the space in the market for a diarrhoea treatment kit. We had designed and marketed an aspirational product (just like Coke) which people wanted and which retailers could make a profit on by bringing it to their communities to sell (just like Coke).
- This is why the retailers bought Kit Yamoyo. They bought it and brought it to their communities for same reason they buy and bring Coca-Cola – because people want it and they can make a profit selling it to them. And everyone else in the distribution chain responds to this same motivation. This PULLS the product into the remotest of communities. For these value chains to work you must design a product that people WANT. To understand what they want you need to ask them. This process is often referred to as Human Centred Design. Generally this is not the way the public health sector works. Most health products and services are designed by experts on the basis of what they think people need. Although this has to be the approach for many drugs, I would argue that patient-centred design processes could be used a lot more in the health sector than is currently the case. The big prize for designing a health product that people want, is that they are more likely to pay for it and, if they are, you can engage the existing private sector distribution channels to get it to them. You don’t have to set up your own distribution systems.
- This presented us with a very big problem. The world had signed up to the idea of the kits in the crates. And we had won some very prestigious global awards. We’d established ourselves as innovators in the eyes of the world but we now had to pivot? What were we to do?
- This is where business guru, Stephen Covey, comes in. He said that in business “The main thing is to keep the main thing the main thing” and that’s exactly what we did. We were in the business of saving lives not winning awards.
- It was time for our first re-think…
- At the end of the trial we ploughed all the learning into a re-design of Kit Yamoyo. This was aimed at improving the kit but we also had to drive out all subsidy. Nothing was exempt from this review. We even redesigned the much acclaimed packaging that fitted between the Coke bottles in a crate. Nothing was sacred!
- The result was two new formats: the screw-top and the flexi-pack Both of these maintained as many of the features as possible from the original design.
- In particular, the water measuring feature.
- We were even able to achieve this with the flexi-pack
- With our scale-up design in place, we started marketing this new product in the same ways you would market any fast moving consumer good. This is the artwork for the billboards used. You will notice that ColaLife’s name is not there; we are invisible to the customer as we are not a permanent part of the solution.
- This is the production line. Note that the local manufacturer is producing the product for the market. They are NOT producing it for us (ColaLife). This means that the whole initiative can be self-sustaining in the long term.
- So things were going well. We were well on our way to establishing a commercial diarrhoea treatment kit in the private sector. Kit Yamoyo was available in 100s of community shops.
- And nationwide in supermarkets.
- However, a series of events, meant that sales into the private sector remain a modest levels. Sales even fell after the trial when the donor-funded launch marketing ceased and Zambia has been hit by high inflation over the last two years. So, although our private sector model is working, sales volumes were not exciting from the manufacturer’s point of view. Had we stopped here we may have failed.
- However, after the trial the Zambian government started showing an interest in distributing a government branded version of the commercial flexi-pack which the manufacturer was able to produce very easily by simply changing the instruction leaflet that also carries the branding.
- The government orders transformed the sales for the manufacturer.
- And by the end of this year, when current orders have been fulfilled, the graph will look like this with 94% of sales going to the government. At this point it is interesting to reflect on the changes that have occurred from our original idea. We started off with the idea of distributing medicines through the unused space in Coca-Cola crates exclusively through the private sector and this is where we’ve come to by keeping resolutely focussed on our vision of “saving lives through better access to ORS and Zinc for the treatment of diarrhoea”.
- Crucial to this engagement by the government was a policy change and this took the form of the Zambian government adding co-packaged ORS and Zinc to their National Essential Medicines List. Without doing this the government would not have been able to buy co-packaged ORS and Zinc. To achieve this listing, we as private sector, product design innovators had to turn our hand to lobbying for policy change. And as I have said before, if we hadn’t done this our innovation may have failed.
- I want finish off by telling you what we plan to do next to have a global impact. Once it was clear that things in Zambia were going to be self-sustaining with no further support from ColaLife, we turned our attention to achieving a global impact. As things stood in 2017, the only way we saw of doing this was to move to another country and repeat the same process that we had gone through in Zambia. A trial was likely to be required, as our approach was seen as an innovation and not part of the mainstream. This would have been a tedious and slow process. So instead, we decided to apply our limited resources to trying to move our innovation to the mainstream of global child health policy.
- In 2017 ColaLife recruited the Diarrhoea Innovations Group to an effort to get co-packaged ORS and Zinc on the WHO Essential Medicines List. After more than a year of work, our application was submitted to the WHO in Nov-18. In Jul-19 WHO published a revised Essential Medicines List, adding co-packaged ORS and Zinc as the recommended treatment for diarrhoea. This is a game-changer and moves our work out of the ‘innovation box’ and into the mainstream of global child health. For most countries, the question is now “how do we implement the new WHO recommendation?” and not “should we test this co-packaging idea?” This will make globalisation much more straightforward and rapid. I want to finish by making the point that to have real impact innovations need to move to the mainstream – they need to become ‘the new way of doing things’. Thank you,
- So here are some key lessons from our work which may be more widely applicable.
- Firstly, we must foster innovation because we need the step-change that innovation can deliver to reduce health inequalities. The incremental improvement in health that we are seeing, particularly in developing countries, is far too slow and the health divide is increasing. You need to have a clear vision, something to refer back to when things don’t go the way you thought they would. Having a clear vision will help you fail fast, learn and move on. Innovations must be based on what your target group WANT. And to find that out, you must ask them. This has particular importance in the commercial sector but even in other settings it’s better to strive to deliver what you KNOW PEOPLE WANT rather than delivering WHAT YOU THINK PEOPLE NEED. To have a big impact, innovations should be self-sustaining. Key to achieving this is working in partnership and building these partnerships around a shared vision, not around you. And finally, to have a significant impact, you must move your innovation to the mainstream so that it becomes ‘the way we do things’. Thank you.
- Thank you very much.
- Let me finish with some key lessons from our work which may be more widely applicable.
