Hepatitis b package final
- 1. Hepatitis-B
- 2. What is Hepatitis? • “Hepatitis” means inflammation of the liver. • The liver is a vital organ that processes nutrients, filters the blood, and fights infections. • When the liver is inflamed or damaged, its function can be affected.
- 3. Hepatic Physiology Liver: • Weight: 1.5kg (1-2.3kg) & receive 1500 blood/minutes • Largest solid organ in the body • Performs over 500 chemical processes • Produces over 160 different proteins • Makes clotting factors for the blood • Stores & releases sugar as glycogen • Metabolizes, detoxifies, synthesizes • Secrete about 500 ml bile/day
- 4. Functions of liver • Synthesis of plasma proteins • Synthesis of vitamin A • Production of heat • Metabolism of alcohol • Conversion of glucose to glycogen for storage • Storage of fat soluble vitamins: A,D,E, K, iron, copper, some water soluble vitamins e.g. riboflavine, niacin, pyridoxine, folic acid and vitamin B12
- 5. Functions of liver………………. • Desaturation of fat • Deamination of amino acids • Transamination: removing the nitrogenous portion of amino acids and adding it to other carbohydrate molecules forming new non- essential amino acids • Breakdown of erythrocytes • Detoxification of drugs • Inactivation of hormones • Secretion of bile to excrete bilirubin
- 6. General Concepts • Hepatitis = 'inflammation of the liver'. • Six medically important viruses are commonly described as “hepatitis viruses”: HAV,HBV,HCV,HDV,HEV,HGV
- 7. Table 24.12
- 8. Hepatitis-B
- 9. Hepatitis B In the World • Half worlds population: high risk of HBV • 400 million people are chronically infected. Most are unaware of their infection. • 10-30 million will become infected each year. • An estimated 1 million people die each year from hepatitis B and its complications. • Approximately 2 people die each minute from hepatitis B. • 10th Leading cause of death in worldwide.
- 10. • The WHO estimates the global burden of disease from occupational exposure to be 40% of the hepatitis B and C infections and 2.5% of the HIV infections among HCWs as attributable to exposures at work, While 90% of the occupational exposures occur in the developing world.
- 11. • The prevalence of HBV and HCV worldwide vary by region, ranging from 0.5 to 10% for hepatitis B and from 1 to 4% for hepatitis C. • The risks of transmission of infection from an infected patient to the HCW following a NSI are (CDC Report): Hepatitis-B : 3–10% Hepatitis-C : 3% HIV : 0.3%
- 12. Determinants of NSIs include: • Overuse of injections and unnecessary sharps • Lack of supplies: disposable syringes, safer needle devices, and sharps-disposal containers • Lack of access to and failure to use sharps containers immediately after injection • Inadequate or short staffing • Recapping of needles after use • Lack of engineering controls such as safer needle devices • Passing instruments from hand to hand in the operating suite • Lack of awareness of hazard and lack of training
- 13. In Nepal, there are about 3,15,000 people infected with chronic Hepatitis-B. According to the annual report 2009/2010 of Nepal Blood Transfusion Service, Hepatitis B was detected among 596 people and Hepatitis C was detected among 438 across the country. HBV is about 100 times more infectious than HIV.
- 14. • Acute Hepatitis B refers to the first 6 months, after someone is exposed to the Hepatitis B virus. • Some people are able to fight the infection and clear the virus for others, the infection remains and leads to a “chronic,” or lifelong, illness.
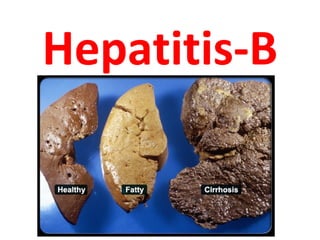
- 15. Why is Hepatitis B such a concern? • Hepatitis-B is the world’s most common blood- borne viral infection. • Approximately 10% of people who get Hepatitis B infections will become lifelong carriers of the disease even though they no longer have symptoms. • Hepatitis B carriers have a higher risk of developing liver cancer (about 25% chronic hepatitis patient develop liver disease).
- 16. How serious is Hepatitis B? • Over time, approximately 15%–25% of people with chronic Hepatitis B develop serious liver problems, including liver damage, cirrhosis, liver failure, and even liver cancer. • Every year more than 6,00,000 people worldwide die from Hepatitis B-related liver disease.
- 17. 3. HBV: Modes of Transmission Parenteral - IV drug abusers, health workers are at increased risk. Sexual - sex workers and homosexuals are particular at risk. Perinatal(Vertical) - mother(HBeAg+) →infant.
- 18. How is Hepatitis B NOT spread? • Hepatitis B is not spread through breastfeeding, sharing eating utensils, hugging, kissing, holding hands, coughing, or sneezing. • Unlike some forms of hepatitis, Hepatitis-B is also not spread by contaminated food or water.
- 19. Risk Groups • Have multiple sex partners • Have STIs • MSM • IVDUs: Sharing needles • Live with a person who has Hepatitis B • On hemodialysis • Are exposed to blood on the job
- 20. Risk Groups…………………….. • Sharing a needle during ear piercing, body piercing or tattoos. • Accidentally pricking with a used needle. • Sharing tooth brushes, razors, or other personal items • Cleaning cuts or open sores of an infected person • have an open cut on skin.
- 21. Concentration of Hepatitis B Virus in Various Body Fluids Low/Not High Moderate Detectable blood semen urine serum vaginal fluid feces wound exudates saliva sweat tears Breast milk
- 22. Hepatitis-B virus (HBV) HBV is a Hepadna virus. An extremely resistant strain capable of withstanding extreme temperatures and humidity. It can survive when stored for 15 years at -20°C, for 24 months at -80°C, for 6 months at room temperatures, and for 7 days at 44°C. Able to survive in dried blood for >1 week.
- 23. Properties of HBV • a member of the hepadna virus group • Circular partially double-stranded DNA viruses • Replication involves a reverse transcriptase. RNA Virus: RNA-Protein DNA Virus: DNA-RNA-Protein
- 24. HBV DNA RNA PROTEIN Reverse transcriptase 24
- 25. HBV : Structure
- 26. WBC: N/E/B/L/M (WBC Engulf antigen) Lymphocytes: produced & mature in stem cells in bone marrow, regulate immune system, kill cells that bear specific target antigen. -B: produce antibodies against the pathogen and are dependent on T-cells for the information of pathogen. produced in stem cells in bone marrow and travel to mature in thymus gland. -T: T=helper (CD4):recognize virus and stimulate B-cell to actively fight infection. T=Suppressor (CD8): Suppress T & B cell after control of infection. T= Cytotoxic (killer): recognize virus infected cells and Kill them directly. 26
- 27. 5. Pathogenesis & Immunity • Virus enters hepatocytes via blood • Immune response (cytotoxic T cell) to viral antigens expressed on hepatocyte cell surface responsible for clinical syndrome • 5 % become chronic carriers (HBsAg> 6 months) • Higher rate of hepatocellular cancer in chronic carriers, especially those who are “e” antigen positive • Hepatitis B surface antibody likely confers lifelong immunity (IgG anti-HBs)
- 29. Four stages in the viral life cycle Stage I: Immune Tolerance • The duration of this stage for healthy adults is approximately 2-4 weeks and represents the incubation period. • For newborns, the duration of this period often is decades. • Active viral replication is known to continue despite little or no elevation in the aminotransferase levels and no symptoms of illness.
- 30. Stage II: Immuno response • Inflammatory reaction: natural defense of body. • The immune system attack the hepatitis- B infected cells in the liver and start to clear the infection from body. • This phase lasts in few weeks if infected cells clears, other wise last for years if not clear infected cells.
- 31. Stage III: Viral clearance: • Known as seroconversion because body produce anti-body against surface antigen “e” of the HBV. • In this phase HBV stop reproducing it self. • In the host can target the infected hepatocytes and the HBV Viral replication no longer occurs. • HBeAb can be detected. • The HBV DNA levels are lower or undetectable, and aminotransferase levels are within the reference range. • HBsAg still is present.
- 32. Stage IV: Immunity to Hepatitis-B • When full antibody is produced and clear HBV from body. • Hepatitis-B genetic material (DNA) usually disappears. • Most of the individual develop life long immunity and 10% enter in stage II & III again and become chronic carrier. • They infect others, and chronic liver damage.
- 34. Incubation • Viral incubation ranges from 45-180 days. • Symptoms begin an average of 90 days (range: 60–150 days) after exposure to HBV.
- 35. C/F of Acute Hepatitis B A. Symptoms: 1. Pre-icteric Phase/ prodromal stage: 3–9 days - Lethargy, Chills, headache, malaise - Anorexia, distaste, nausea, vomiting, diarrhoea - Upper abdominal pain - Arthralgia, skin rashes and poly arthritis. Examination: fever with relative bradycardia + enlarged tender liver
- 36. 2. Icteric Phase: 2-4 w • Increase Jaundice with decrease fever & improvement of general condition • Constitutional symptoms diminishes • Dark- colored urine due to bilirubinuria • Clay- colored urine due to cholestasis • Loss of weight • Pruritus as a result of elevated serum bile acid/salt
- 37. 3. Post-icteric Phase (recovery phase) • Disappearance of jaundice • Urine and stool color become normal • Appetite improve • GI symptoms disappears Complete recovery of liver may take up to 6 months
- 38. B. Signs • Jaundice • Tender hepatomegaly • Spleenomegaly (10%) • Enlarged cervical lymph node
- 39. Symptoms of Chronic Hepatitis B • Many people with chronic Hepatitis-B do not have symptoms and do not know they are infected. • Even though a person has no symptoms, the virus can still be detected in the blood. • Symptoms of chronic Hepatitis-B can take up to 30 years to develop. • Damage to the liver can silently occur during this time. When symptoms do appear, they are similar to acute infection and can be a sign of advanced liver disease.
- 41. Diagnostic strategy • History & Physical examination • Jaundice • RUQ tenderness +- Hepatomegaly • Liver function tests • HBs Ag in serum: – Presence of HBsAg
- 43. The following tests are done to help diagnose and monitor people with hepatitis B: 1. HBsAg: Hepatitis-B surface antigen. A positive result means you have an active infection. 2. Anti-HBsAg: anti-body to surface antigen. No need Rx. 3. Anti-HBc: anti-body to core-antigen. 4. HBeAg: Hepatitis Be antigen- pre-core region of the HBV genome. 5. Anti-HBeAg: anti-body to e-antigen. 6. Virological Markers: HBV DNA 7. Biochemical marker: alanine aminotransferase (ALT) 8. Histological markers: liver biopsy.
- 44. Patterns of Abnormal • Elevations in ALT & AST only: suggests cellular injury • Elevations in Alk Phos & Bilirubin: suggests cholestasis or obstruction. • Mixed pattern: ALT, AST, AP & Bili: probably the most common scenario
- 45. Patterns of Abnormal • Consider degree of elevation: Very high ALT and AST usually only come from a couple of sources: - Acute viral hepatitis (A,B,C) - Acetominophen toxicity / overdose - “Shock Liver”; cardiac or surgical event?
- 46. Management: Approach 1. Clinical suspension: S/S, jaundice etc 2. Serology (with HCV): HBsAg +ve -Repeat 3. Counselling: explain prognosis- Ca lung, HCV, HIV, Cirrhosis, precautions 4. Stable patient: send viral load 5. HBe - +ve, = Acute infections 6. Liver biopsy: shows stage of liver damage 7. Rx: Lamivadine/Interferon + vitamins + symptomatic Rx -Drugs: Increase dose to decrease viral load - Duration: 6months to 2 years or life long, depends on viral load
- 47. Management • No specific treatment • Sever patient needs admission • Bed rest • Diet: ND with slight fat restriction, glucose & fruit juice beneficial, anti-emetic, ORS • Avoid: sedative & hypnotics if possible • Educate patient about preventive measures • Anti-viral drugs: if available
- 48. Management Three main drugs: 1. Interferon: expensive, very effective 2. Lamivudine: less expensive, not very effective 3. Adefovir Dipivoxil Newer drugs: 1. Entecavir 2. Telbivudine 3. Clevudine 4. Emtricitabine 5. Pegylated alpha interferon
- 49. Interferon alfa • Had been mainstay for therapy • Subcutaneous injection three times per week for 3 months or longer • 30% of patients who could tolerated regime had a successful response – Seroconverted to HBe antibodies – Normalization of LFTs • Multiple side effects – Fever, myalgia, thrombocytopenia, depression • Contraindicated in very advanced liver disease
- 50. 9. HBV PEP: Exposure to diagnosed HB Pt. exposed within 48 hours of the incident/ neonates whose mothers are HBsAg and HBeAg positive. Is previously vaccinated or not = yes – 3 dose, complete = Not sure/not complete: check for anti- HBsAg if anti-HBsAg Positive: no need vaccination
- 51. Post-exposure management Post-exposure prophylaxis (PEP) involves giving hepatitis B vaccine and possibly immunoglobulin too if required. – Immunoglobulin is given at a different site and it does not reduce the immune response to the vaccine. – If the status of the source is unknown assume infection. – It should be given within 48 hours and certainly no later than 7 days after exposure. – On site: clean wound with soap-water
- 52. Prevention • Universal/Standard Precautions: maintain • Vaccination - highly effective recombinant vaccines • Hepatitis B Immunoglobulin (HBIG) -exposed within 48 hours of the incident/ neonates whose mothers are HBsAg and HBeAg positive. • Other measures -screening of blood donors, blood and body fluid precautions. Drinking alcohol can make your liver disease worse.
- 53. Universal Precautions: The general Principles of Infection Prevention and Control (STANDARD PRECAUTIONS) CDC guidelines: Achieving optimum hand hygiene. Using personal protective equipment. Safe handling and disposal of sharps. Managing blood & bodily fluids. Decontaminating equipments. Managing accidents. Good communication. Training / education. Consider all the patients are infected: blood & body fluids
- 54. New CDC guideline recommends frequent use of alcohol-based handrubs New recommendations are shown on the following slides
- 55. When should you wash your hands with soap and water? Wash your hands with plain or antimicrobial soap and water if : • your hands are visibly soiled (dirty) • hands are visibly contaminated with blood or body fluids • before eating • after using the toilet
- 56. When should you use an Alcohol Based Handrub ? If hands are not soiled or contaminated with blood or body fluids, use an alcohol-based handrub : • before direct contact with patients • after direct contact with a patient’s skin • after having contact with body fluids, wounds or broken skin • after touching equipment or furniture near the patient • after removing gloves • after handwash with soap and water
- 57. Tips on how to wash your hands effectively • Wet hands first with water – not hot • Apply 3 to 5 ml of soap to hands • Rub hands together for at least 15 seconds • Cover all surfaces of the hands and fingers • Rinse with water and Dry • Use paper towel to turn off tap
- 58. Tips on how to use an alcohol handrub • Take 1.5 to 3 ml of an alcohol gel / rinse in the palm • Rub hands together x 10-15 seconds • Cover all surfaces of your hands and fingers • Include areas around / under fingernails • Continue rubbing hands together until alcohol dries It takes around 10 -15 seconds of rubbing for the hands to dry
- 59. Some more tips on how to use an alcohol-based handrub • If after cleaning your hands 8 to 10 times with an alcohol based handrub, you feel a “build-up” of emollients on your hands, wash your hands with soap and water • After cleaning your hands with an alcohol based handrub make sure the hands are totally dry before putting on gloves.
- 60. Chemicals used in Hospital – Chlorine (Boric acid power): 14 gm / lit. – Cidex (glutraldehyde) – 2% – Savlon: 1% ,2% ,5% – Betadine: 2.5% , 5% , 7.5% – Phenol (mob): 2% – Formalin: 40%, (10% biopsy). – Spirit – 70% – Carbolic aid. 2% – H2O2 = 30%
- 61. –Skin: spirit dry 2 min (Min 30 sec) (contact period) –Thermometer-clean - 70% alcohol. –Cheattle forceps: autoclave and dry. –Blood stained linen: 1% sodi. Hyp. – 30 min.
- 62. Hepatitis B Vaccine • Hepatitis B vaccine is the best protection. • For adults, the Hepatitis B vaccine is given as a series of 3 shots over a period of 6 months (0-30-180 days) (0-1-6 Months) • The entire series is needed for long-term protection. • Booster doses are not currently recommended.
- 63. VACCINE RECOMMENDATIONS • Hepatitis B vaccine available since 1982 • Routine vaccination of 0-18 year olds • Vaccination of risk groups of all ages • As of December 2006, 164 countries vaccinate infants against hepatitis B during national immunization programmes - a major increase compared with 31 countries in 1992, the year that the World Health Assembly passed a resolution to recommend global vaccination against hepatitis B.
- 64. Complications of Hepatitis 1. Fibrosis • scarring of the liver. The liver is damaged by constant inflammation and creates the scar tissue to repair itself. Unfortunately, this scar tissue keeps the liver from working as it once did. When the fibrosis becomes extensive, it is called cirrhosis.
- 65. 2. Cirrhosis of the Liver Extensive fibrosis is called cirrhosis. Hepatitis C and alcoholic hepatitis are two very common causes of cirrhosis, though there are many others. 3. Cancer of the Liver Hepatocellular carcinoma is a type of cancer that affects the liver cells. 4. Liver Failure Liver failure is a serious, but uncommon, complication of hepatitis 5. Glomerulonephritis Glomerulonephritis is a complicated disorder of the kidneys caused by inflammation and is seen in chronic hepatitis B and hepatitis C infections.
- 66. 6. Cryoglobulinemia Abnormal cluster of a kind of protein that blocks small blood vessels leading to circulation problems. 7. Hepatic Encephalopathy Severe loss of liver function, such as liver failure, can lead to inflammation in the brain called encephalopathy. This causes mental problems, like confusion, and can lead to coma. Advanced hepatic encephalopathy is a serious condition and is usually fatal.
- 67. 8. Portal Hypertension One of the liver's important jobs is to filter blood. However, cirrhosis and other problems can interfere with the liver's portal circulation system. When this portal system is blocked, blood can't return to the liver from the digestive system and pressure increases, called portal hypertension. This is a serious complication and can be fatal. 9. Porphyria Porphyria is a group of diseases caused by problems processing important chemicals in the body called porphyrins. One type, called porphyria cutanea tara, leads to blistering of the hands and face and is a rare complication of chronic hepatitis C infection.
- 68. 10. Viral Co-Infection A person who is infected with both the hepatitis B and the HIV viruses is said to have a HBV/HIV Co-infection. Approximately 10% of the HIV-infected population worldwide is infected with hepatitis B. This figure may approach 20% in Southeast Asia, and 5% in North America and Western Europe. ( I found 30% HB+ve)
- 70. Precautions • Practice safe sex: use condoms during sex • Do not share toothbrushes, razors or other personal items • Do not share needles, syringes or other injecting equipment • Do not donate blood, sperm, organs or any other tissues • Be careful about blood contact
- 71. Nursing Care Plan The symptoms of acute hepatitis B infection include: • Loss of appetite • Feeling tired • Muscle and joint aches • Low-grade fever • Abdominal pain • Yellowish discoloration of the skin • Tea- or cola-colored urine
- 72. • Grayish or clay-colored stools: A few people develop a severe form of hepatitis B known as fulminant hepatitis. • This form of the disease appears rapidly and can cause death. Its symptoms include: • Mental confusion, hallucinations, or extreme sleepiness • Jaundice • Noticeable swelling of the abdomen • Sudden collapse
- 74. Hepatitis-B: Summary • HBV: Blood, semen, saliva, vaginal secretions • Highly contagious; sexually transmitted • 90-95% self limited over 6 months • Chronic infection: >6 months • Nurses must be careful about it: vaccination and PEP is important
- 75. Thank you
- 76. Clinical outcomes of Hepatitis B infections Figure 66-11. Clinical outcomes of acute hepatitis B infection. (Redrawn from White DO, Fenner F: Medical virology, ed 3, New York, 1986, Academic Press From Murray et. al., Medical Microbiology 5 th edition, 2005, Chapter 62, published by Mosby Philadelphia,,
- 77. Acute Hepatitis B Virus Infection with Recovery Typical Serologic Course Symptoms HBeAg anti-HBe Total anti-HBc Titre HBsAg IgM anti-HBc anti-HBs 0 4 8 12 16 20 24 28 32 36 52 100 Weeks after Exposure
- 78. Interferon therapy Indication: 1. Detectable markers of HBV replication ALT >2 times Dose: • 5 MU(s/c) daily or10 MU(s/c) three times/ week X16 wks Contraindication: • ALT normal or <2 times • Immunocompromised • Decompensated disease • Childhood acquisition
- 79. Complications of interferon therapy • Flulike syndrome • Bone marrow suppression • Emotional liability • Autoimmune thyroiditis • Alopecia • Rashes
- 80. Lamivudine • Dose: • 100 mg OD X 12 month or till seroconversion Hbe Ag sero conversion 16-20% at 1 year Adefovir Dipivoxil Dose: • 10 mg OD X ≥48 wks • Complication: Nephrotoxicity
Editor's Notes
- 2 2 2
- 1 1 1
- 30
