Bpd,nnf kerala,march 2019 - Dr Karthik Nagesh
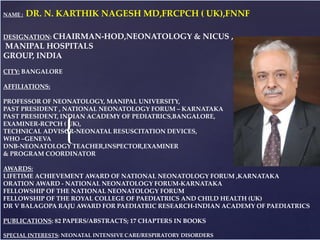
- 1. { PHO TO NAME : DR. N. KARTHIK NAGESH MD,FRCPCH ( UK),FNNF DESIGNATION: CHAIRMAN-HOD,NEONATOLOGY & NICUS , MANIPAL HOSPITALS GROUP, INDIA CITY: BANGALORE AFFILIATIONS: PROFESSOR OF NEONATOLOGY, MANIPAL UNIVERSITY, PAST PRESIDENT , NATIONAL NEONATOLOGY FORUM – KARNATAKA PAST PRESIDENT, INDIAN ACADEMY OF PEDIATRICS,BANGALORE, EXAMINER-RCPCH ( UK), TECHNICAL ADVISOR-NEONATAL RESUSCITATION DEVICES, WHO –GENEVA DNB-NEONATOLOGY TEACHER,INSPECTOR,EXAMINER & PROGRAM COORDINATOR AWARDS: LIFETIME ACHIEVEMENT AWARD OF NATIONAL NEONATOLOGY FORUM ,KARNATAKA ORATION AWARD - NATIONAL NEONATOLOGY FORUM-KARNATAKA FELLOWSHIP OF THE NATIONAL NEONATOLOGY FORUM FELLOWSHIP OF THE ROYAL COLLEGE OF PAEDIATRICS AND CHILD HEALTH (UK) DR V BALAGOPA RAJU AWARD FOR PAEDIATRIC RESEARCH-INDIAN ACADEMY OF PAEDIATRICS PUBLICATIONS: 82 PAPERS/ABSTRACTS; 17 CHAPTERS IN BOOKS SPECIAL INTERESTS: NEONATAL INTENSIVE CARE/RESPIRATORY DISORDERS
- 2. CURRENT STRATEGIES IN MANAGEMENT OF BPD DR KARHIK NAGESH N
- 3. NICU, Manipal hospital, Bangalore
- 4. BPD Bronchopulmonary dysplasia is characterized by alveolar simplification , arrest in lung growth, impaired vascular development and abnormal pulmonary function As per NICHD, BPD is defined as oxygen use and/or respiratory support at 36 weeks PMA(or 56 days of age for infants at >32 weeks GA)* Optimal definition of BPD -controversial, since oxygen use at 36 weeks have failed to predict long term respiratory morbidities. Update on strategies for the prevention and management of BPD * Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–1729
- 5. 28 Weeks POG…Stormy Course! 1993 • Baby S, outborn -28 weeks, 1.1kg. • No Surfactant • RDS from Birth: blow by oxygen given and shifted • Intubated at our NICU. Hypoxia, acidosis • Ventilated,(Pressure Mode,IMV) for severe RDS for 4weeksSignificant PDA ligated in OT > weaned off IMV • Sepsis with DIC • NEC perforated Resection > colostomy > re-anastamosis • ROP CryoSurgery done in OT. • Day 86 discharged home • CLD RDS (HMD) RDS (HMD) Pressure Limited Time Cycled Ventilators
- 6. BPD-STG.II Fallout of MV …2000, Severe CLD • 24-28 Weeks POG • APH • Antenatal Steroids • Severe RDS • IPPV with AMBU Bag at Birth…T- Piece • High Ventilatory Requirements • Surfactant…Bovine • CLD…Ventilated…Months O2 Dependent… 8 months
- 7. ELBW---25 Weeks POG 2016 (IVF-Donor Ovum) by LSCS (REDF) at 25 weeks. Antenatal steroids given At birth, intubation/IPPV through T-Piece resuscitotor. Birth weight 460gm Early rescue Surfactant (Porcine) given and extubated after 12 hours to CPAP (INSURE). Aggressive TPN nutrition program instituted-Day1 Apnoea needing continued CPAP/HHHFNC (21% FiO2) Stable in Room Air …by 10 days GERD….Full OG Feeds at 2 weeks , KMC
- 9. How do Antenatal Steroids Work? Science • Accelerate development of pneumocytes, thus improving lung mechanics (maximal lung volume, compliance) and gas exchange • Increases surfactant production • Induction of surfactant release, absorption of alveolar fluid, increase lung antioxidant enzymes Reduction in RDS, moderate to severe RDS Reduction in Intraventricular hemmorhage, Necrotising enterocolitis, mortality, systemic sepsis
- 10. Capillary leak A syndrome of inflammation Diffuse alveolar epithelial damage Breakdown of endothelial barrier Interstitial edema Proteinaceous alveolar flooding Type 2 cell Apoptotic Type 1 cell Pathophysiology of Acute Lung Injury in HMD Acute Lung Injury in Preterms
- 11. Complications of Invasive ventilation Pressure VILI Volume Trauma Barotrauma Atelectotrauma “Inappropriate Ventilation Of A Neonate Can Be More Harmful Than The Disease Itself ”
- 12. COIN* Trial • 610 infants, 25 to 28 weeks • Distress at 5 minutes of life • CPAP or Ventilation • Surfactant only if intubation and criteria for this not pre-specified • In CPAP group – Only 46% required intubation in first 5 days – Nearly 50% escaped surfactant Early Rescue CPAP *CPAP or Intubation and Ventilation without surfactant (CPAP or Intubation (COIN Trial)) ,Morley CJ et al,2008 Grade A
- 13. CPAP is an alternative to intubation and surfactant in preterm infants (Grade A) • 1316 infants, 24 to 27 weeks • CPAP vs. Intubation and Surfactant at birth • For CPAP group surfactant was given – If intubated at birth – Failed CPAP i.e. FiO2>50% • In CPAP group – 33% did not receive surfactant – 83% got intubated – Lesser need for ventilation in first 7 days • Prophylactic CPAP “SUPPORT” trial,NEJM,2010
- 14. Both SUPPORT and COIN trials support CPAP alone a safe alternative to intubation and surfactant Primary outcome was Death or BPD •Intubation rates of 83% and 46% Only • 33% and 50% lesser need of surfactant
- 15. IN-SU-RE technique Stevens et al. Cochrane 2007 Reduction in mechanical ventilation, BPD, mortality Always combine with early CPAP Grade A Grade A
- 16. Volume Targetted Ventilation Uses Lesser PIP once Lungs Improve • Relatively constant Tidal Volumes • Prevention of Overdistension and Volume Trauma- Sudden changes in Compliance • Automatic-Weaning • Compensation for Variable Respiratory Drive Grade A ( Cochrane,2011)
- 17. How does NIV work? CPAP • ↑FRC • Stabilization of the chest wall • ↓in airway resistance • Improvement in lung volume and oxygenation NIPPV • ↑in MAP allowing better recruitment of alveoli • ↓work of breathing • ↑in Vt and minute volume • Improving the respiratory drive
- 18. Minimally Invasive Surfactant Therapy • These techniques have included administration of exogenous surfactant by • Brief tracheal catheterization, • Aerosolization, and laryngeal mask. • Of these, the methods involving brief tracheal catheterization have been most extensively studied, with surfactant administered by using both a flexible feeding tube and a semi-rigid vascular catheter
- 19. Less Invasive Surfactant Administration…The Future • Surfactant administration by minimally invasive methods that allow for spontaneous breathing might be safer and more effective than administration with endotracheal intubation and mechanical ventilation in preterms ‘at risk’ or with RDS American Academy of Pediatrics ,July 2014, VOLUME 15 / ISSUE
- 20. Management of early BPD • Exogenous surfactant replacement therapy has been effective in RDS , but has not decreased the incidence of BPD. • Multicentre RCTs evaluating outcomes of infants who were on MV and received late surfactant at 2 weeks did not show significant difference in the outcome of severe BPD, but surfactant treated group had lesser respiratory morbidity at 1 yr of age.* • Cochrane review with meta-analysis of RCTs showed slight decrease in the risk of BPD or mortality associated with use of animal derived versus synthetic surfactant in preterm infants at risk of developing RDS* • RCT is in progress comparing synthetic surfactant CHF5633 to Curosurf in extremely preterm infants with BPD as one of the outcome * Hascoet JM, Picaud JC, Ligi I, et al. Late Surfactant Administration in Very Preterm Neonates With Prolonged Respiratory Distress and Pulmonary Outcome at 1 Year of Age: A Randomized Clinical Trial. JAMA pediatrics. 2016;170:365-372. * Ardell S, Pfister RH, Soll R. Animal derived surfactant extract versus protein free synthetic surfactant for the prevention and treatment of respiratory distress syndrome. Cochrane Database Syst Rev. 2015;8:CD000144 EARLY BPD
- 21. Surfactant Delivery And Ventilation Statergy • Mode of surfactant delivery- Meta-analysis of 6 RCTs have concluded that LISA decreases the risk of BPD, death ,early CPAP failure or invasive ventilation requirements. • Meta analysis comparing prophylactic CPAP to assisted ventilation with or without surfactant in preterm infants less than 32 weeks gestation demonstrated reduction in the incidence of BPD* • No significant difference in the outcome of BPD was noted with prophylactic INSURE vs CPAP. • NIPPV is more effective than NCPAP in preventing BPD, however as primary respiratory support no difference was seen in incidence of BPD. * Rigo V, Lefebvre C, Broux I. Surfactant instillation in spontaneously breathing preterm infants: a systematic review and meta-analysis. European journal of pediatrics.2016;175:1933-1942. EARLY BPD
- 22. VENTILATION STATERGY • Ventilation strategy- As lung compliance changes rapidly during RDS and its treatment, volume targeted ventilation appears to be appropriate. • Cochrane review reported 21% reduction in death/BPD for VTV compared to pressure limited MV.* • Cochrane review on elective use of HFOV soon after intubation showed significant reduction in death/BPD at 36-37 weeks PMA or discharge and in BPD alone.* EARLY BPD * Klingenberg C, Wheeler KI, McCallion N, et al. Volume-targeted versus pressure limited ventilation in neonates. Cochrane Database Syst Rev 2017;10:CD003666. *Cools F, Offringa M, Askie LM. Elective high frequency oscillatory ventilation versus conventional ventilation for acute pulmonary dysfunction in preterm infants. Cochrane Database Syst Rev 2015:CD000104
- 23. Steroids In BPD • PREMILOC TRIAL- Large multicentre randomised placebo controlled trial designed to look at the effect of early low dose hydrocortisone on survival without BPD in extremely preterm infants with gestation 24 0/7 to 27 6/7 wks.* • Hydrocortisone was administered at a dose of 1mg/kg/day divided into two doses on days 1-7 followed by one dose 0.5 mg/kg/day for next 3 days.* • 60% survived without BPD compared to 51% assigned to placebo , Odds ratio -1.48* (p<0.04) • Long term follow up results showed no significant difference in neurodevelopmental outcomes between infants in the 2 groups at 2 year follow up.* EARLY BPD Baud O, Maury L, Lebail F, et al. Effect of early low-dose hydrocortisone on survival without bronchopulmonary dysplasia in extremely preterm infants (PREMILOC): a double-blind, placebo-controlled, multicentre, randomised trial. Lancet. 2016;387:1827
- 24. Inhaled Steroids In BPD • NEUROSIS TRIAL-Inhaled budesonide vs placebo was administered to extremely premature infants (23 0/7 to 27 6/7 weeks GA) starting within 24 hrs after birth.* • Budesonide was administered at dose of 400 mcg every 12 hrs in the first 14 days of life and 200 mcg from day 15 until infants no longer need respiratory support.* • Infants who received budesonide had lower rate of BPD but higher death rate (16.9 vs 13.6 %)* • Meta-analysis of published trials have concluded that inhaled steroids were associated with significant reduction in BPD, however long term studies are needed before routine recommendation* EARLY BPD *Bassler D, Plavka R, Shinwell ES, et al. Early Inhaled Budesonide for the Prevention of Bronchopulmonary Dysplasia. N Engl J Med. 2015;373:1497-1506
- 25. Surfactant With Steroids for BPD • Meta-analysis of 2 RCTs demonstrated intratracheal budesonide-surfactant mixture was associated with decreased risk of BPD and composite outcome of death/BPD. • In the above studies, very low birth weight infants with severe RDS requiring mechanical ventilation and fractional inspired concentration >0.5 were randomised to receive either intratracheal budesonide combined with survanta or survanta alone within four hours after birth. • Intervention group had significantly lower incidence of BPD/death with number needed to treat 4.1 95% CI 2.8-7.8* EARLY BPD *Yeh TF, Chen CM, Wu SY, et al. Intratracheal Administration of Budesonide/Surfactant to Prevent Bronchopulmonary Dysplasia. Am J Respir Crit Care Med. 2016;193:86-95
- 26. • Intra-tracheal administration of budesonide- surfactant combination was associated with decreased incidence of BPD alone or composite outcome of death or BPD in VLBW Intra-Tracheal Administration of Budesonide-Surfactant in Prevention of Bronchopulmonary Dysplasia in Very LBWs: A Systematic Review and Meta-Analysis. Venkataraman , Kamaluddeen , Hasan SU, Robertson HL, Lodha A Pediatr Pulmonol. 2017 Jul;52(7):968-975. doi: 10.1002/ppul.23680. Epub 2017 Feb 6. EARLY BPD
- 27. AZITHROMYCIN AND BPD Meta-analysis support (12 RCTs) the association between ureaplasma infection and development of chronic lung disease in preterm infants. Macrolide antibiotics has immunomodulatory effects suppressing lung inflammation Treatment with azithromycin has been promising in a meta-analysis demonstrating reduction in BPD in preterm infants when given prophylactically. Studies combining use of all macrolides in ureaplasma colonised ventilated preterm infants did not show reduction in BPD ,hence routine use for the prevention of BPD is not recommended.* EARLY BPD *Nair V, Loganathan P, Soraisham AS. Azithromycin and other macrolides for prevention of bronchopulmonary dysplasia: a systematic review and meta-analysis. Neonatology. 2014;106:337–347
- 28. Nitric Oxide And BPD Infants with BPD are at increased risk for secondary pulmonary hypertension due to intermittent episodes of hypoxia causing pulmonary vasoconstriction. 17 clinical RCTs - iNO was administered as either treatment during first three days of life, routine use in preterm babies along with respiratory support or later treatment for infants at increased risk for BPD . Cochrane systematic review showed no consistent long term improvement in mortality or the incidence and severity of BPD when using iNO in preterm infants as prevention or rescue strategy.* EARLY BPD * Barrington KJ, Finer N, Pennaforte T. Inhaled nitric oxide for respiratory failure in preterm infants. Cochrane Database Syst Rev. 2017;12:CD000509.
- 29. • 22 RCTs were incorporated. Risk of BPD was significantly lower in preterm infants supplemented with iNO (relative risk [RR] = 0.88; P = 0.0007)
- 30. Proven Benefits in BPD! CAFFEINE- RCT of Caffeine for apnoea of prematurity (CAP) trial provide unequivocal evidence in the reduction of BPD by 36 % in VLBW infants. BPD was decreased by 52 % if caffeine was given on postnatal days 1- 3 compared to 23 % reduction if given after day 3.* Phase 4 trial is evaluating if administration of caffeine at earlier time (2 vs 12 hrs of life ) in infants born <32 weeks will have an effect on intubation rates* VITAMIN A- BPD rates was reduced by 13 % in infants <1000 gms receiving Vit A( 3*5000 IU/week intramuscular over 4 weeks) compared with placebo EXCLUSIVE BREAST MILK-Data from german neonatal network have shown exclusively formula fed infants have 2.6 times increased risk of BPD than breast milk fed infants* EARLY BPD *Schmidt B, Roberts RS, Davis P, et al. Caffeine therapy for apnea of prematurity. N Engl J Med 2006;354:2112–21. *Darlow BA, Graham PJ. Vitamin A supplementation to prevent mortality and shortand long-term morbidity in very low birthweight infants. Cochrane Database Syst Rev
- 31. Other Strategies in BPD…Promising! PENTOXIFYLLINE- It decreases production of inflammatory cytokines and has significant immunomodulatory properties. Pilot study of 150 VLBW infants had shown nebulised pentoxifylline reduced risk of BPD , however recent RCT in preterm infants in 81 preterm infants demonstrated nebulised pentoxifylline did not reduce duration of oxygen supplementation* OMEGA 3 LONG CHAIN PUFA-Meta-analysis including 18 RCTs showed that omega 3 LCPUFA supplementation was not associated with decreased risk of BPD, but when considering RCTs less than 32 weeks of gestation, authors found trend toward reduced BPD rates* EARLY BPD *Lauterbach R, Szymura-Oleksiak J, Pawlik D, Warchol J, Lisowska-Miszczyk I, Rytlewski K. Nebulized pentoxifylline for prevention of bronchopulmonary dysplasia in very low birth weight infants: a pilot clinical study. J Matern Fetal Neonatal Med. 2006;19:433–438. *Zhang P, Lavoie PM, Lacaze-Masmonteil T, Rhainds M, Marc I. Omega-3 long- chain polyunsaturated fatty acids for extremely preterm infants: a systematic review. Pediatrics. 2014;134:120–134
- 32. Management in ‘EVOLVING BPD’ STOP-BPD TRIAL-Effect of hydrocortisone initiated between 7 and 14 days after birth on death/BPD in very preterm infants Preterm infants with gestational age of less than 30 weeks and/or birth weight of less than 1250 g were randomly assigned to receive 22 day course of systemic hydrocortisone or placebo * Death or BPD occurred in 128 of 181(70.7%) infants randomised to hydrocortisone and in 140 of 190(73.7%) infants randomised to placebo. Among mechanically ventilated very preterm infants administration of hydrocortisone between 7 and 14 days after birth, compared with placebo did not improve the composite outcome of death or BPD at 36 weeks postmenstrual age. *Onland W et al. Effect of hydrocortisone therapy initiated 7-14days after birth on mortality or bronchopulmonary dysplasia among very preterm infants receiving mechanical ventillation. JAMA 2019; 321:354-363
- 33. Diuretics and BPD Premature infants with BPD develop interstitial and alveolar edema due to iatrogenic fluid overload to maintain adequate hydration and nutrition , capillary leak due to pulmonary inflammation or patent ductus arteriosus due to pulmonary over circulation. Diuretics improve pulmonary edema and lead to decreased pulmonary vascular resistance and improved pulmonary compliance. However Cochrane meta-analysis revealed enteral administration of furosemide in preterm infants at 3 weeks of age resulted in minimal effect on BPD, whereas single dose of aerosolized furosemide in preterm infants >3 weeks of age found transient improvement in pulmonary function. Cochrane meta-analysis of six studies on the use of thiazides in preterm infants demonstrated improvement in lung mechanics and decreased need for supplemental furosemide boluses *Brion et al. Aerolised diuretics for preterm infants with chronic lung disease. Cochrane database systemic review. EVOLVING BPD
- 34. Therapy in Established BPD DIURETICS-Thiazides and spironolactone comprise together most commonly used diuretic in established BPD. In a randomised double blind crossover trial with sequential analysis, oral diuretics improved pulmonary mechanics in 10 infants with BPD. Long term use of combination therapy for oxygen dependent BPD infants was studied in randomised double blind placebo controlled study where infants receiving spironolactone and hydrochlorothiazide had significant improvement in lung mechanics, decrease in fraction of inspired oxygen compared to placebo. Large meta-analysis in preterm infants greater than 3 weeks of age with chronic lung disease, acute and chronic administration of thiazide diuretics showed improved pulmonary mechanics. ESTABLISHED BPD *Kao LC, Warburton D, Cheng MH, Cedeño C, Platzker AC, Keens TG. Effect of oral diuretics on pulmonary mechanics in infants with chronic bronchopulmonary dysplasia: results of a double-blind crossover sequential trial. Pediatrics 1984;74:37- 44. * Kao LC, Durand DJ, McCrea RC, Birch M, Powers RJ, Nickerson BG. Randomized trial of long term diuretic therapy for infants with oxygen dependent
- 35. Therapy in Established BPD INHALED STEROIDS-Infants with established BPD are more likely to experience respiratory illness and episodes of wheezing requiring hospitalisation during first 2 yrs of life. In randomised placebo controlled trial -30 infants CLD, who received fluticasone or placebo via metered dose inhaler and spacer starting at 36 wks reported no difference in respiratory symptoms, duration of supplemental O2 use, respiratory illness or need for hospitalization. Yuskel et al showed improvement in respiratory symptoms in premature infants with chronic lung disease who received beclomethasone compared to placebo ESTABLISHED BPD *Beresford MW, Primhak R, Subhedar NV, Shaw NJ. Randomised double blind placebo controlled trial of inhaled fluticasone propionate in infants with chronic lung disease.
- 36. Therapy in Established BPD SYSTEMIC STEROIDS-No clear indication exists for use for systemic steroids with established BPD Single center study showed the effect of oral prednisolone on weaning oxygen in infants with established BPD (63 % of patients were successfully weaned off supplemental oxygen prior to hospital discharge).* Infants who were successfully weaned off supplemental oxygen received oral prednisolone for single course, no additional benefit was conferred with multiple courses. ESTABLISHED BPD * Bhandari A, Schramm CS, Kimble C, Pappagallo M, Hussain N. Effect of a short course of prednisolone in infants with oxygen-dependent bronchopulmonary dysplasia. Pediatrics 2008;121:e344-349.
- 37. Therapy in Established BPD BRONCHODILATORS-Higher rates of airway reactivity exists in BPD survivors, but eosinophilic inflammation doesn’t contribute to obstructive lung disease in BPD. Structural abnormalities in the airways along with small airway caliber, reduced elastic recoil increase airway narrowing with smooth muscle contraction in BPD survivors. In clinical practice, BPD survivors who exhibit wheezing will respond to albuterol even they don’t fit into asthma paradigm. No randomised trials evaluating effects of anticholinergic medications such as ipratropium bromide in infants with established BPD. ESTABLISHED BPD * Baraldi E, Bonetto G, Zacchello F, Filippone M. Low exhaled nitric oxide in school-age children with bronchopulmonary dysplasia and airflow limitation. Am J Respir Crit Care Med 2005;171:68-72.
- 38. BPD and pulmonary hypertension Thresholds for initiating vasodilator therapy include Trjet velocity >3 /sec, estimated RV/LV systolic pressure >0.5 and septal flattening in absence of significant right to left shunt. Sildenafil PDE5 inhibitor commonly used first line therapy for BPD associated PH ,is usually well tolerated. Large retrospective cohort study had identified 17 % of the 598 infants diagnosed with BPD associated PH received sildenafil. Milrinone: PDE3 inhibitor increases cAMP levels in arterial smooth muscles and myocardium resulting in decreased pulmonary vascular resistance and increased cardiac contractility. Small series suggested that milrinone improved biventricular output and reduced RV pressures in NO resistant preterm infants with PH. Bosentan: Orally active non selective ETA and ETB receptor antagonist is FDA approved for children 3yrs of age and above. Limited data exists for use in PH. * Backes CH, Reagan PB, Smith CV, Jadcherla SR, Slaughter JL. Sildenafil Treatment of Infants With Bronchopulmonary Dysplasia-Associated Pulmonary Hypertension. Hosp Pediatr. 2016;6(1):27- 33.
- 39. EMERGING THERAPIES for BPD INOSITOL-Cochrane metanaysis showed significant reduction in death compared with untreated controls, Phase 3 trial is currently in progress for prevention of BPD. Recombinant Human Club Cell 10-Kilodalton protein-Levine et al in pilot study of 22 VLBW ventilated preterm infants with RDS found no difference in the BPD rates between rhCC treated and control infants. Phase 2 trial is in progress evaluating survival in ELBW infants. Mesenchymal stem cell therapy-Five ongoing clinical trials are in progress, however recent phase 1 clinical trial, nine preterm infants with Mean GA of 26 weeks at high risk for BPD were treated with intratracheal dose of Allogenic umbilical cord derived MSCs and BPD appears to be lower compared with controls. *Chang YS, Ahn SY, Yoo HS, et al. Mesenchymal stem cells for bronchopulmonary dysplasia: phase 1 dose-escalation clinical trial. J Pediatr. 2014;164:966.e6- 972.e6. * Levine CR, Gewolb IH, Allen K, et al. Safety, pharmacokinetics, and antiinflammatory effects of intratracheal recombinant human Clara cell protein in premature infants with respiratory distress syndrome. Pediatr Res. 2005;58:15–21.
- 40. THANK YOU