Dengue in children notes from cpg.pdf
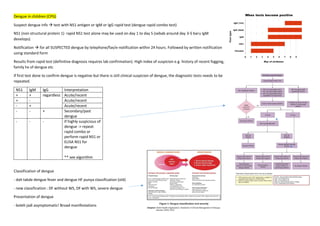
- 1. Dengue in children (CPG) Suspect dengue infx test with NS1 antigen or IgM or IgG rapid test (dengue rapid combo test) NS1 (non structural protein 1) rapid NS1 test alone may be used on day 1 to day 5 (sebab around day 3-5 baru IgM develops) Notification for all SUSPECTED dengue by telephone/fax/e-notification within 24 hours. Followed by written notification using standard form Results from rapid test (definitive diagnosis requires lab confirmation). High index of suspicion e.g. history of recent fogging, family hx of dengue etc If first test done to confirm dengue is negative but there is still clinical suspicion of dengue, the diagnostic tests needs to be repeated. NS1 IgM IgG Interpretation + + regardless Acute/recent + - Acute/recent - + Acute/recent - - + Secondary/past dengue - - - If highly suspicious of dengue -> repeat rapid combo or perform rapid NS1 or ELISA NS1 for dengue ** see algorithm Classification of dengue - dah takde dengue fever and dengue HF punya classification (old) - new classification : DF without WS, DF with WS, severe dengue Presentation of dengue - boleh jadi asymptomatic! Broad manifestations
- 2. - infection to one DENV serotype confers protection to that particular serotype only. So, still susceptible to be infected with other serotypes in secondary dengue infx. (greater risk of severity) - features of lab confirmed dengue : n&v, absence of URTI, liver enlarged, thrombocytopenia ( pt <100,000/microL) and leukopenia (leukocyte <4000/microL) Phases of dengue fever - incubation period 4-10 days after the bite 1. Febrile phase (lasts 2-7 days) (difficult to diff with other causes of febrile illness; refer table dydx) - high grade fever (sudden) - facial flushing, skin erythema, generalized body aching, myalgia, arthralgia, retro-orbital pain, photophobia, rubelliform exanthema, headache, anorexia, n&v - dydx table - EARLIEST abnormality detected in investigation is DECREASED IN WBC COUNT (leucopenia) (high probability of dengue) - can also have hematological manifestations i.e. gum bleedm petechiae, nose bleed, easy bruising or bleeding at venipuncture sites - complications in this phase : dehydration & febrile seizures 2. Critical phase (after 3rd day of illness (maybe earlier or as late as 8th day of illness)) (usually lasts 24-48 hours) - occurs around time of defervescence (temp drops and remains below 38) - plasma leakage can happen d/t increased capillary permeability [evidence of plasma leakage is by an elevated HCT level and rapid onset of thrombocytopenia or warning signs] - HCT level : a/w loss of plasma volume. The higher the hemoconcentration, the greater the severity of disease - manifests as warning signs - increased and continuous vascular permeability (main pathophysio) continuous plasma leakage hemoconcentration and hypovolemia shock (dengue shock syndrome, DSS) - severe organ failure can also occur without plasma leakage or shock (hepatitis, encephalitis, myocarditis) - early stages of shock -> body tries to compensate by maintaining the normal SBP. ** stages of shock
- 3. 3. Recovery phase (24-48 hours after onset of plasma leakage) - gradual reabsorption of extravascular compartment in the next 48-72 hours (may have new onset of respiratory distress d/t fluid overload) - cardiac manifestations : bradycardia, hypertension - patients GC improved gradual return of appetite, no more GI symptoms, stabilized hemodynamic status, commencement of diuresis - HCT may decrease due to dilutional effects of reabsorbed fluid warrants no further action soon will have increase WBC f/b recovery of platelet count - development of confluent erythematous or petechial rash with small areas of normal skin over the extremities (isles of white in the sea of red) Risk factors for severe dengue **(kalua rajin boleh baca other predictors of severe dengue in children) - lethargy - abdominal pain - bleeding tendencies - hepatomegaly - HCT >22% from baseline - thrombocytopenia <100,000 micr/L
- 4. MANAGEMENT ikut phase (around 5% of all cases will develop severe dengue) 1. febrile phase - arrive at correct diagnosis! - outpatient or admit? (positive NS1 Ag test is NOT an indication for admission bcs 65% of non severe dengue are NS1+) - Acetaminophen (PCM) may be used for fever & pain. But dose need to be adjusted since there is theoretical risk of liver injury. So, recommend PCM 10mg/kg/dose, not more than 3-4 times in 24 hours in children - Perform tepid sponging if pt still has high fever - DO NOT prescribe : Aspirin (acetylsalicylic acid), ibuprofen, other NSAIDS OR Intramuscular injections (can aggravate gastritis and bleeding) - If outpatient what to do 1. Daily vital signs monitoring (temp, pulse, BP, CRT) 2. Daily FBC monitoring (HCT & Pt especially) (daily FBC is recommended until critical phase has resolved) 3. Daily fluid intake and urine output (advise caregivers to record) (adequate urine output? 4-6 times/day) 4. Advise to come if condition worsen or if presence of warning signs. 5. Provide with dengue monitoring card and dengue home care leaflet. - If inpatient (Admitted) what to do - how frequent to monitor clinical and lab paramenters depends on severity and phase of illness ; refer - must document finding in dengue chart - perform rapid hemodynamic assessment at bedside : C (colour of skin) C (CRT) T(temperature of extremities) V (volume ; pulse) R (rate; pulse) CCRTV
- 5. 2. critical phase - what are our top 3 priorities in critical phase? 1. Replace plasma loss 2. Early recognition and tx h’ge 3. Prevent fluid overload - overweight or obese patient use ideal body weight for calculating fluid infusion rates) - Must separate fluid resuscitation and fluid maintenance - Goals of fluid resuscitation ^ improve in circulation : so check if decreasing tacychardia, BP improve, pulse volume improve, warm & pink extremities, CRT <2 ^ improve in end organ perfusion : improve consciousness and improve urine output ^ appropriate decrease in HCT - all patients in SHC=OCK must have blood sample taken and cross matched - when to admit to PICU **refer text tepi - choice of resuscitation fluid : ISOTONIC CRYSTALLOID SOLUTION ; these fluids should NOT contain glucose(bcs glucose causes osmotic diuresis which worsens the hypovolemic shock). For maintenance pun sama isotonic crystalloid. - colloid guna when there is persistent shock despite resuscitation with crystalloid. (colloids not used for early intervention. Colloids ni kita concern sebab dia boleh cause allergic adverse reactions) -Treatment of Warning signs 49324i0923jedm - Treatment of compensated shock 1. Obtain baseline HCT 2. Secure IV/IO access within 5 minutes 3. Start IV fluid resuscitation with isotonic crystalloid solutions at 10-20 ml/kg/hr 4. Reassess patients vitals, CRT, HCT, UO 4. if improve or oral intake improve -> reduce fluid accordingly 5. Stop IV fluid if patient shows sign of reabsorption 6. If vital signs unstable or shock persists, check HCT urgent
- 6. 7. If HCT increases or still high with evidence of shock, repeat crystalloid at 10-20 ml/kg/hr. then consider changing to colloid 10-20 ml/kg/hr after resuscitation with 40ml/kg of crystalloid - decreasing HCT with unstable vital signs -> bleeding occult. Transfuse with FWB/Packed cells - Treatment of decompensated shock (hypotensive shock) 1. Secure IV access within 5 mins 2. Initiate IV fluid resuscitation with crystalloid solution at 20 ml/kg as a bolus over 15-30 minutes 3. consider colloid if pulse pressure <10 mmHg 4. monitor closely and urine output hourly with an indwelling catheter - continuous ECG and pulse oximetry is advisable in unstable patients (shock patients) - the higher the fluid infusion rate, the more frequent monitoring has to be done (to avoid fluid overload) - IV fluid administer using infusion or saline pumps - how frequent to check UO? Each hour until the patient is out of shock, then every 1-2 hours. [continuous bladder catheter is essential] [ UO 0.5-1 ml/kg/hr] - monitoring with bedside USG if available to detect pleural effusion and ascites after fluid boluses if previously not detected. (monitor breathing and assess need of respiratory support) - how frequent to monitor HCT? Monitor before and after fluid boluses until stable, then 4-6 hourly. Also must take HCT whenever there are changes in fluid infusion rate - rise of HCT beyond 30% of baseline during critical phase indicated significant plasma leakage interpretation of HCT **table above - additionally, severe dengue patients, must monitor for [blood glucose, RFT, LFT, coagulation profiles] before resuscitation and as indicated - if hypoglycaemia is there, treat emergency with bolus of 2ml/kg of D10% - maintain euglycaemia with glucose-isotonic solution (NS D5% running at maintenance rate according to Holiday Segar formula) - sodium bicarbonate for metabolic acidosis c/b tissue hypoxia is not recommended for PH >/= 7 . (a/w sodium and fluid overload, increase in lactate, hypercarbia and decrease ionized calcium) - acute encephalopathy in dengue is managed by supportive measures and emphasis on correction of underlying metabolic & hemodynamic abnormalities
- 7. - to prevent nosocomial infections, venofix/branula need to be removed once there is no longer indication of IV fluid therapy - small doses of IV furosemide 0.1-0.5 mg/kg/dose BD/TID or continuous infusion 0.1mg/kg/hr may be indicated for patients who are out of critical phase Criteria to discharge Vaccine to prevent dengue : CYD-TDV dengvaxia