Organophosphate poisoning
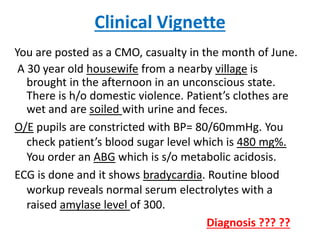
- 1. Clinical Vignette You are posted as a CMO, casualty in the month of June. A 30 year old housewife from a nearby village is brought in the afternoon in an unconscious state. There is h/o domestic violence. Patient’s clothes are wet and are soiled with urine and feces. O/E pupils are constricted with BP= 80/60mmHg. You check patient’s blood sugar level which is 480 mg%. You order an ABG which is s/o metabolic acidosis. ECG is done and it shows bradycardia. Routine blood workup reveals normal serum electrolytes with a raised amylase level of 300. Diagnosis ??? ??
- 2. Organophosphorus Poisoning Presenters : Dr Lohit Chauhan : Dr Dhananjay Gupta Moderator : Dr. Gurmeet Kaur
- 3. INTRODUCTION • OP are a group of insecticides or ‘nerve- agents’ which act at acetyl-cholinesterase • Have been used as insecticides, petroleum additives and chemical warfare agents • Carbamates are another group of insecticides which act at the same site, with a slight different MOA
- 4. WHO CLASSIFICATION (simplified) HIGHLY TOXIC MODERATELY TOXIC 1. Phosphamidon (Dimecron) 1. Malathion 2. Ethyl parathion 2. Fenthion (Baytex) 3. Methyl parathion 3. Temephos (abate) 4. Chloro-thiophos 4. Fenitrothin (tik-20) 5. Carbo-phenothion 5. Diazinon (spectacide) * Shivakumar S, Ishaq RM. Management of Organophosphorus compounds (OPC) Poisoning : Current Status 2008. taken from drshivkumar.org
- 5. Epidemiology (WHO) • Acute OP poisoning is one of the common and serious medical emergencies • Asia : 3 million cases/ year of acute pesticide poisoning • 3 lakh deaths per year (CFR =10-15 %) • 99% cases are seen in developing world
- 6. Indian Data • Poisoning is 4th MC cause of deaths annually • OP poisoning is the MC poisoning • Pattern of poisoning is region-dependant • OP poisoning is more common in south India • North India- aluminium phosphide > OP
- 7. RML Data
- 8. Why is OP poisoning common ?? • India is an agarian country • routinely used in farming CAUSES OF HIGH MORTALITY 1. High toxicity of available compounds 2. Time gap in transporting patients 3. Paucity of Health care personnel 4. Lack of training facilities 5. Lack of antidotes
- 9. Why is OP poisoning common ?? Limited resources and infrastructure for health care delivery
- 10. 1. Mode of poisoning 85% 15% SUICIDAL ACCIDENTAL * Banerjee I, Tripathi SK, Roy AS. Clinico-Epidemiological Characteristics of Patients Presenting with Organophosphorus Poisoning. N Am J Med Sc. Vol 4(3), JMarch 2012
- 11. 2. Occupation 42% 34% 10% 9% 5% HOUSE WIVES FARMERS SHOPKEEPERS LABOURERS STUDENTS * Maharani B, Vijayakumari M. Profile of poisoning cases in a tertiary care hospital in Tamil Nadu, India. J of App Pharma Sc. Vol 3(01), Jan 2013
- 12. 3. Seasonal distribution 21% 12% 32% 35% SPRING WINTER RAINY SUMMER * Maharani B, Vijayakumari M. Profile of poisoning cases in a tertiary care hospital in Tamil Nadu, India. J of App Pharma Sc. Vol 3(01), Jan 2013
- 13. 4. Type of Poison 36% 29% 19% 16% Me Parathion Diazinon Chlorpyriphos Dimecron * Banerjee I, Tripathi SK, Roy AS. Clinico-Epidemiological Characteristics of Patients Presenting with Organophosphorus Poisoning. N Am J Med Sc. Vol 4(3), JMarch 2012
- 14. 5. Relative human Toxicity Eddleston M et al. Differences between organophosphorus insecticides in human self- poisoning: a prospective cohort study. Lancet. 2005 Oct 22-28;366(9495):1452-9
- 16. Clinical Features 1. Acute O-P poisoning - Muscarinic features Resp distress - Nicotinic features Death - CNS features 2. Intermediate Syndrome 3. Delayed neuropathy (OPIDP) 4. Neuro-psychiatric disorder (COPIND)
- 17. 1. Acute O-P poisoning MUSCARININC FEATURES NICOTINIC FEATURES CNS FEATURES D iarrhoea Muscle weakness Fatigue U rination Muscle fasiculations Confusion M iosis Muscle paralysis Unconsciousness B ronchorrhea B ronchospasm Seizues E mesis Hypertension Ataxia L acrimation Tachycardia Resp. depression S alivation S weating
- 18. 2. Muscarinic / Wadia type 1 syndrome 1. Excessive Sweating 2. Miosis 3. Bronchorrhoea / spasm 4. Bradycardia 5. Hypotension
- 19. 3. Bronchorrhoea • Early cause of morbidity and mortality • Excess fluid is from airway secretions • Obstruction of upper and lower airways • Pulmonary edema - - hypoxia - - death
- 20. The Grading of Clinical severity Severity AChE (RBC) Muscarinic Nicotinic CNS Mild > 40% nausea, vomiting, diarrhoea, salivation, bronchorrhoea and -constriction, bradycardia headache, dizziness Moderate 20 - 40% as above, + miosis, incontinence fasciculations (fine muscles) as above, + dysarthria, ataxia Severe < 20% as above, + fasciculations (diaphragm, resp. muscles) as above, + coma, convulsions
- 21. 4. Intermediate syndrome • Described in 1987 (Karalliedde and Senanayake) • Occurs 24-96 hours after resolution of acute cholinergic crisis • Most imp. factor responsible is quantum of exposure of OPC • May occur from inadequate oxime therapy
- 22. IMS - pathophysiology • Incidence = 10-50 % • Prolonged effects on Nicotinic receptors • Primary motor end plate degeneration • Leads to muscle weakness
- 23. IMS- muscle weakness of • Muscles innervated by cranial nerves : III-VII and X • Neck flexors - a constant feature - one of the earliest signs - inability of patients to raise heads off pillow • Proximal limb muscle weakness - typically involve shoulder abductors, hip flexors • Respiratory muscles - death
- 24. IMS – other features • Deep tendon Reflexes : Usually absent / decreased • Sensory system usually intact • Muscarinic symptoms : absent rarely short relapses may occur
- 25. IMS- complications • Weakness -- Frank paralysis • Respiratory distress -- Death • Main cause of morbidity and mortality in Indian patients.
- 26. 5. OPIDP • OP induced Delayed Polyneuropathy • Delayed, rare, neurotoxic effect • 1-5 weeks after severe acute poisoning, due to slow release of OP from body fat • symmetrical sensory-motor axonal degeneration of the peripheral nerves and SC
- 27. 5. OPIDP - C/f Motor 1. Sharp cramp like pain in calf 2. High stepping gait (initially) 3. Shuffling gate in severe cases 4. Quadriplegia / paraplegia 5. Wrist and foot drop 6. Mild pyramidal signs Sensory 1. Glove-stocking anesthesia 2. Cerebellar signs +/-
- 28. 6. COPIND • Chronic OP induced Neuro-psychiatric disorder • Chronic low-dose exposure to OP compounds • 40 hours/week, 9 months/ year • No cholinergic symptoms • Non responsive to levodopa • Plasma cholinesterase levels are normal
- 29. 6. COPIND – c/f Neurological Symptoms Psychiatric Symptoms 1. Impairment in memory 1. Anxiety 2. Impairment in concentration 2. Dysthymia 3. Impairment in leaning 3. Depression 4. Chronic fatigue 5. EPS : dystonia 6. Resting tremor, bradykinesia 7. Rigidity of face Parkinson-like 8. Postural instability Non responsive to levodopa
- 31. Diagnosis of OP poisoning Diagnosis is mainly clinical, Based on : 1. H/o Ingestion of poison 2. Characteristic clinical features 3. Clinical improvement after atropine/ oxime 4. Inhibition of cholinesterase activity
- 32. 1. Inhibition of cholinesterase • Demonstrating a decrease in cholinesterase • Definitive or gold standard method • Theoretically RBC/ true cholinesterase is more accurate than plasma/ pseudo • But plasma / pseudo-cholinesterase is more easily available test
- 33. Diagnosis : Plasma / SChE : - easy to measure - easily available - more useful in acute exposure 1. 50 % reduction in normal values : diagnostic (baseline values usually NA) 2. Progressive increase in SChE with treatment
- 34. 2. Cholinesterase levels Useful in monitoring clinical course of illness persistent Low levels are a predictor of IMS (Intermediate syndrome) SChE activity is < 20 % during onset of IMS * Tajune J, Robert J. Organophosphoric poisoning. Ann Emerg Med 1987 ; 16:193.
- 35. 3. Electro-neuro-myogram (ENMG) • 30 Hz rapid nerve stimulation - decremental responses correlate best with clinical weakness • Most useful diagnostic test of IMS * * Senanayake N et al. Neurotoxic effects of OP insecticides : an intermediate syndrome. NEJM. 1987 ; 316 :761-63.
- 36. 4. Other tests of prognostic value a. Hyperglycemia b. Neutrophilic leucocytosis c. Proteinuria / glycosuria d. ECG changes (QTc prolongation) e. Blood pH (acidosis) f. Hyper amylasemia g. Serum CPK levels
- 37. 5. Hyperglycemia in OP-poison a. Oxidative stress b. Renal tubular damage c. Stimulation of adrenals d. Release of catecholamines Transient hyperglycemia and glycosuria are often seen in acute OP-poisoning * Namba T, Nolte CT, Jackrel J, Grob D. Poisoning due to organophosphate insecticides: Acute and chronic manifestations. Am J Med. 1971;50:475–92.
- 38. 6. Blood pH • Metabolic Acidosis develops in patients of OP poisoning, more common with hypotension*1. • Unknown mechanism. • If pH < 7.20, treatment with sodium bicarbonate beneficial*2. 1. *Prakash O.et al. Low ph predicts mortality in OPP and carbamates poisoning, JAPI 2002; 50:857. 2. *Roberts DM, Buckley NA. Alkalinisation for treating organophosphorus pesticide poisoning. Cochrane Database of Systematic Reviews 2005;1:CD004897.pub2.
- 39. 7. QTc prolongation • Indicates poor prognosis in OP- poisoning 1. Cholinergic stimulation of heart : M2 a. negative ionotropy b. negative chronotropy 2. Oxidative stress causes conduction problems * Shadnia S, Okazi A, et al. Prognostic value of long QTc interval in acute and severe OP poisoning. J of Med Toxico 2009 ; 5(4).
- 40. 8. Hyper- amylasemia • Cholinergic stimulation of salivary glands • Cholinergic stimulation of pancreas • Acute pancreatitis (rare) Raised amylase levels correlate with severity and presence of shock in acute OP poisoning * * Lin CL, Yang CT, Pan KY, Huang CC. Most common intoxication in nephrology ward organophosphate poisoning. Ren Fail 2004 ;26:349-54. .
- 41. 9. Acute Pancreatitis • d/t Excessive cholinergic stimulation and ductular hypertension • Painless Ac. Pancreatitis has been reported • Amylase (>300) : low Sn, low Sp • Lipase (>300) : useful for diagnosis * Hsiao CT, Yang CC, Deng JF, Bullard MJ, Liaw SJ. Acute Pancreatitis following Organohosphate Intoxication. J Toxicol Clin Toxicol. 1996 ;34(3):343-7.
- 42. Management
- 43. What to do ?? 1. Call AIIMS poison cell : (NPIC) - National Poisons Information Cell - Toll free no. 1800 116 117 - Other : 011 - 26589391 - Open 24 X 7 , 365 days a year
- 44. The Paradox of Poisoning…. “The only thing I know is that I don’t know anything” - Socrates
- 45. 1. Identification of poison • History by patient/ attendant • Clinical presentation. • By showing photographs. • WHO colour code on container.
- 46. Poison :Identification WHO colour code on container. Red label Extremely toxic Monocrotophos, zinc phosphide, ethyl mercury acetate, and others. Yellow label Highly toxic Endosulfan, carbaryl, quinalphos, and others. Blue label Moderately toxic Malathion, thiram, glyphosate, and others. Green label Slightly toxic Mancozeb, oxyfluorfen, mosquito repellant oils and liquids, and most other household insecticides.
- 47. Identification of poison • Signs of cholinergic excess or developing intermediate syndrome • Disparity between history and clinical presentation, follow, clinical judgment. • After identification classify as Organophosphorus and non-Organophosphorus. Organophosphosphate
- 48. Management :Immediate, Protocol Assess and record 15-point Glasgow Coma Scale. Pulse rate, BP and auscultate Patient : left lateral position- head lower than the feet. Oxygen, Intubate if respiratory distress. Start atropine : reduce bronchorrhoea. 0.9% normal saline, Aim SBP > 80 mm Hg & urine output >30 ml/h
- 49. When not sure about the poison..?? • ‘Atropine test‘ : Inject 0.6- 1 mg IV atropine. • If pulse rate goes up by 25 per minute or skin flushing develops patient has mild or no toxicity for OP’s.
- 50. Management : Specific General Principles of Therapy : • Decontamination, Resuscitation, Stablization. • Muscarinic antagonists • Fluids. • Acetylcholinesterase reactivators. • Gastric Decontamination. • Miscellaneous.
- 51. Decontamination • Healthcare workers and OP Poisoning. • Few western hospitals, reported such poisoning. • None shows inhibition of Acetyl/Butyryl cholinesterases. • Cases from Asia : Health-care workers take no special precautions , No cases of secondary poisoning reported.
- 52. Decontamination • Guidelines : Universal Precautions, Maximum Ventilation, Frequent rotation of staff to keep exposure minimum. • PPE should not consist Latex / Vinyl. • Patient : All clothing to be removed, discard in ventilated area. • Thorough irrigation with water. • Wash with soap and water. • Soaps containing 30% ethanol advocated. • Ocular decontamination : water only.
- 53. Initial Stabilisation • Patent Airway, adequate Breathing and Circulation. • Oxygen at first opportunity. • Little evidence, Atropine not to be given until oxygen availability*1. • However, in hospitals where oxygen not available, Atropine to be started early*2. • Patient Position : Left Lateral, Neck Extended. Reduce aspiration risk. Keeps airway patent. Decrease pyloric emptying and absorption of poison. *1 Erdman AR. Insecticides. In: Dart RC, Caravati EM, McGuigan MA, et al, eds. Medical toxicology, 3rd edn. Philadelphia: Lippincott Williams & Wilkins, 2004: 1475–96. *2 Aaron CK. Organophosphates and carbamates. In: Shannon MS,Borron SW, Burns M, eds. Clinical management of poisoning and drug overdose, 4th edn. New York, Elsevier Science, 2006.
- 55. Gastrointestinal decontamination • Often first intervention • To be considered only after stabilization, oxygen, atropine and oximes. • Lavage only if patient arrives within 1 hour. • Only consider if patient intubated or conscious and willing to cooperate. * The Hazards of Gastric Lavage for Intentional Self Poisoning in a Resource Poor Location Clin Tox 2007;45(2):136-43 Not beneficial, rather increases chances of Aspiration Pneumonia & Deaths*
- 56. Gastrointestinal decontamination • Induced emesis : Ipecacuanha induced , Contraindicated. • Activated charcoal : Studies failed to find any benefit ( Why..??) It binds in vitro, but not in gut due to rapid absorption. Ingested dose too large for the amount of charcoal. NO evidence suggests that patients with pesticide poisoning benefit with activated charcoal.* * Eddleston M, Juszczak E, Buckley NA, et al. Randomised controlled trial of routine single or multiple dose superactivated charcoal for self-poisoning in a region with high mortality. Clin Toxicol 2005; 43: 442–43.
- 57. Muscarinic antagonist Atropine Muscarinic Antagonist Good CNS penetration, cause Anticholinergic delirium, agitation and psychoses. Glycopyrrolate Less CNS penetration, Less CNS side effects. Lesser respiratory complications Ineffective in countering Coma and reduced respiration. Hyoscine methobromide and Hyoscine Hyoscine has the best CNS penetration Methbomide form not permeable to BBB.
- 58. Muscarinic antagonist • A small RCT found no difference in mortality or ventilator rates, comparing Atropine and Glycopyrrolate. • Hyoscine : best for severe Extra-pyramidal features with few peripheral signs • In animal studies, found more effective than Atropine for control of seizures induced by inhaled nerve gas agents. • However, Atropine remains mainstay of therapy. Easy and wide availability. Affordability . Moderate ability to penetrate CNS.
- 59. Muscarinic antagonist AIM OF THERAPY : ATROPINE • To reverse cholinergic features. • To improve Cardiac and Respiratory functions. • Target Endpoints of Atropinization. 1. Drying of Pulmonary secretions, ie. Clear lung fields on auscultation. (Most reliable) 2. Heart rate > 80 beats / min. 3. SBP > 80 mmHg. 4. Pupils : No longer pinpoint. 5. Dry Axillae. 6. Bowel sounds : just present.
- 60. End points of atropinisation 1. Lung secretions 2. Hypotension 3. Bradycardia 4. Sweating 5. Miosis 6. Bowels : Hyperactive A T R O P I N E 1. Clear Chest 2. SBP > 80mmHg 3. HR > 80/min 4. Dry Axillae 5. Pupils no longer pinpoint. 6. Bowel sounds : Just present
- 61. Atropine Dosing Incremental Dosing 1.8 to 3 mg Atropine (i/v) Repeat every 5 minutes with doubling the dose each time. Endpoint : Atropinization. Followed by : 10 to 20 % of total dose required for atropinization every hour via i/v infusion To be held once anticholinergic effects occur.(Absent bowel sounds, urinary retention, agitation). Bolus DosingV/S 2-5 mg Atropine every 10 to 15 min. Endpoint : Atropinization. Followed by maintenance using reduced doses or increasing time duration in b/w doses. Various studies clearely found Incremental Dosing far superior to bolus dose administration
- 62. Atropine Monitoring • Patient to be assessed every 15 min to check adequacy of dosages. • If clinical features recur, further increment in boluses and doubling. • Once parameters reached, Monitoring hourly for atleast 6 hours to check effectiveness of infusion. Time heart rate Clear lung Pupil Dry axilla SBP > 80 mm Hg Bowel sounds mental state Fever >37.5c SPO2 Atropine infusion dose OP / Carbamate Observation Sheet
- 63. Atropine : When to stop..?? Bronchorrhoea : most important, for titrating dose. • Atropine toxicity = absent bowel sounds + fever + confusion. • Stop infusion for 60 min, if toxicity. • Re-start infusion at 80% of initial rate, once the temp. comes down and patient calms. • Most do not need >3-5 mg (5-9 ml) / hour of atropine infusion. • Reduce rate by 20% every 4 hourly once patient is stable. STOP.
- 64. Oximes • Reactivate Acetyl cholinesterase, remove phosphoryl group. • Discovered in 1950’s by Wilson et al. • Among various oximes (obidoxime and trimedoxime) Pralidoxime (PAM) remains, most widely used. • Prevent continued toxicity by Scavenging and detoxifying enzyme. • Also endogenous anticholinergic effects. • Available in four Salts : chloride, iodide, metilsulfate, and mesilate. • Chloride and iodide most widely used in developing countries. • Chloride salt better than iodide. More active compound per gram of salt. No risk of thyroid toxicity.
- 65. Oximes Therapeutic effectiveness depends on 1. Concentration of poison consumed (Poison load). 2. Time lapse between poisoning and administration 3. Type of OPC. (More effective on diethyl than dimethyl). Dimethyl compound reactivate and “age” at slower rate. 4. Lipid solubility of OPC. 5. Concentration of Oxime in blood.
- 66. Oximes The Controversies • Two RCT’s in Vellore, India in early 1990’s noted, Harm from low dose PAM infusion. • A Cochrane review ( included two RCT’s , 2005) & two other meta-analysis reported no clear benefit or harm. • An RCT in Baramati, India studying very high dose of PAM in 200 patients with moderate OP poisoning showed reduced Case fatility. (1% vs 8%).
- 67. Oximes The consensus • Oximes will not be effective in very severe (large dose) poisoning. • Treatment with oximes should be started as early as possible, no role if started after 48 hours. • Less effective in severe complications such as aspiration pneumonia or hypoxic brain injury before treatment. • Less or no effectiveness with dimethyl compounds and atypical organophosphates. • Not effective in carbamates but are not contraindicated either.
- 68. Oximes Dosing • PAM : 1-3 gm/day, no role after 48 hrs. • Serum levels of > 4 mg/lit is necessary for effective treatment. • To achieve this, administered as bolus 20-40mg/kg followed by continuous infusion at 500mg/hr. • WHO recommendations : Loading dose 30mg/kg, followed by infusion of 8mg/kg/hr.
- 69. Oximes Therapeutic end point • Resolution of muscle fasciculation and weakness, Reactivation and Increment in SChE levels. • Use longer than 24 hours indicated if unaged OP’s release from fat tissue. • Infusion continued until patient remains symptom free for atleast 12 hours without additional atropine. • Or until extubated.
- 70. Role of Benzodiazepines • Control agitation. • Sedation in ventilated patients. • Many opioids, metabolized via SChE, so use for sedation in pulmonary edema can worsen CNS manifestation. • Control of seizures : First line therapy in OP poisoning, phenytoin not recommended d/t membrane stabilizing effects. • Seizures uncommon in oxygenated patients, more common in nerve gas agents (soman and tabum). • Diazepam reduce neural damage and prevent respiratory failure (animal studies).
- 71. Role of Magnesium Sulphate • MgSO4 (4g) i/v in first day after admission, decrease hospitalization period and mortality. • It blocks Calcium channels and reduce acetylecholine release from presynaptic terminals. • Also reduces CNS overstimulation from NMDA receptor activation.
- 72. Role of Clonidine • Centrally acting α2-adrenergic receptor agonists. • Reduces acetylcholine synthesis and release from presynaptic terminals • Animal studies, shown benefit in combination with atropine. Effect in humans unknown.
- 73. Advanced Neuroprotective Drugs 1. Ketamine : Noncompetitive NMDAR antagonist, within 1 hour of nerve gas agent induced seizures along with Midazolam/diazepam. 2. Tezampanel : Glutamate receptor antagonist specific for kainate subtype Rc, useful in soman(nerve gas) induced seizures and neuropathy. 3. Gacyclidine : Another antiglutamatergic compound found beneficial in conjunction to standard therapy in nerve gas poisoning .
- 74. Advanced Neuroprotective Drugs 4. For OPIDN : standard therapy plus corticosteroids. 5. Protease inhibitors : target esterase and prevent delayed neuropathy. 6. Intermediate syndrome resistant to standard treatment, artificial respiration. 7. Antioxidants : lipid peroxidation and thiobarbituric formed in OP poisoning, Antioxidant beneficial. Vitamin E reported to have therapeutic effect
- 75. Intermediate syndrome : Management • Usually presents 12 to 96 hours after exposure. • Early signs : action tremors and pharyngeal weakness (difficult deglutition , pooling of secretions). • Later : inability to flex neck, DTR’s lost, cranial neuropathies, proximal muscle weakness and respiratory muscle paralysis. • Not all require intubation and ventilation, but patients with tremors and pharyngeal weakness, at increased risk. • Treatment : totally symptomatic. Ventilator support if respiratory muscle paralysis.
- 76. Ventilatory Support Indicated in stupor / coma, Hypoxemia (PaO2 <60 mmHg) and profound muscle weakness. Predictors for need of mechanical ventilation. 1. Delay in the initiation of specific treatment. 2. Low level of sensorium at admission 3. Pinpoint pupils and generalized fasciculations. 4. Presence of convulsions 5. Presence of respiratory failure at admission. 6. High initial atropine requirement for atropinization.
- 77. Weaning off Ventilator • Asses respiratory muscle performance before weaning off patient. • Reduce slowly and gradually pressure support level in CPAP with PSV mode. • Extubate if : spontaneous breathing with no distress. generates VT >5 mL/kg at Pressure of 3-5 cm of H2O. Parameter Weaning threshold PaCO2 <50 mmHg Minute ventilation (spontaneous) <10-15 L/min Tidal volumes >5 mL/kg Maximum voluntary ventilation >20 L/min Respiratory frequency <35 breaths/min or >6 breaths/min
- 78. Role of Alkalinization • IV infusion of Soda. Bicarbonate produce moderate alkalinization (pH : 7.45 to 7.55) in OP poisoning. • Infusion of higher dosages (5mEq/Kg) in 60 minutes followed by 5-6 mEq/kg/day was shown useful.(In dogs) • More beneficial in Nerve agent poisoning. • Cochrane review : Insufficient evidence to establish use of NaHCO in human OP Poisoning.
- 79. Role of Early Enteral Feeding. • Early enteral feeds associated with improved outcomes in critically ill because it prevents enterohepatic circulation. • Early nutritional supplementation in OP poisoning assumes importance as these patients may require prolonged ventilatory support.
- 80. Role of Fresh Frozen Plasma. • FFP contains important components like clotting factors, proteins, enzymes, etc. • It is hypothesized that butyrylcholinesterase present in FFP sequester free poison in blood and remove it from circulation. • Two trials, both unfavourable to FFP intervention. Current evidence not strong enough to make clear conclusion regarding bioscavenger role of FFP
- 81. For the future….. • Removal of OP’s from blood : Hemodialysis, Hemoperfusion or hemofiltration. • Hemofiltration after dichlorovos poisoning revealed beneficial therapeutic effects. • Military research aims at : Injecting Butyrylcholinesterase after cloning into soldiers before exposure to nerve gases. Not practical for prophylaxis in self-poisoning as one cannot predict when a person is going to ingest pesticide. • Use of recombinant bacterial phosphotriesterases, or hydrolases to break down OP’s enzymatically.
- 82. Take home message 1. Early stabilization and resuscitation. 2. Incremental dose Atropine. 3. Early institution of Oximes. 4. External decontamination, MgSO4, Clonidine, Use of benzodiazepines and NMDA receptor antagonists, Alklinization, Early Enteral feeding were found to be beneficial. 5. FFP, forced emesis were found harmful. 6. Activated charcoal, Gastric lavage were found to have no benefit or harm. 7. Gastric lavage : easily performed, cheap could be used as an adjunct if performed within one hour.
- 83. Thank You
