Equine reproductive disorders
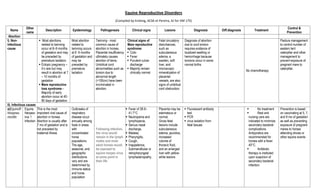
- 1. Equine Reproductive Disorders (Compiled by Embing, ACSK et Pereira, AJ for VM 175) Name Other name Description Epidemiology Pathogenesis Clinical signs Lesions Diagnosis Diff.diagnosis Treatment Control & Prevention Abortion I). Non- Infectious cause Most abortions related to twinning occur at 8–9 months of gestation and may be preceded by premature lactation Ectopic pregnancy – it‘s rare but may result in abortion at 7 – 10 months of gestation Mare reproductive loss syndrome - Majority of early abortion occur at 40- 80 days of gestation. Most abortion related to twinning occurs at 8 -9 months of gestation and may be preceded by premature lactation. Twinning - most common cause of abortion in horses. Placental insufficiency ultimately causes abortion of twins. Umbilical cord abnormalities such as torsion due to abnormal length (>100cm) have been incriminated in abortion. Clinical signs of Mare reproductive syndrome: Colic Fever Purulent vulvar discharge Majority remain clinically normal Fetal circulatory disturbances, such as subcutaneous edema, a swollen, soft liver, and microscopic mineralization of placental vessels, are also signs of umbilical cord obstruction. Diagnosis of abortion due to cord torsion requires evidence of localized swelling or hemorrhage because torsions occur in some normal births No chemotherapy Pasture management to control number of eastern tent caterpillar and other management to prevent exposure of pregnant mare to caterpillar. II). Infectious causes a)EquinoR hinopneu monitis Equine Herpesv irus 1 Infection This is the most important viral cause of abortion in horses. Abortion is usually after 7 mo of gestation and is not preceded by maternal illness Outbreaks of respiratory disease occur annually among foals in areas with concentrated horse populations. The age, seasonal, and geographic distributions vary and are determined by immune status and horse population Following infection, the virus would remain in the lymph nodes and most adult horses would be exposed to equine herpes virus at some point in their life Fever of 38.9– 41.7°C Neutropenia and lymphopenia, Serous nasal discharge, Malaise, Pharyngitis, Cough, Inappetence, Submandibular or retropharyngeal lymphadenopathy. Placenta may be edematous or normal. Gross fetal lesions include subcutaneous edema, jaundice, increased volume of thoracic fluid, and an enlarged liver with yellow- white lesions Fluorescent antibody test PCR virus isolation from fetal tissues No treatment Rest and nursing care are indicated to minimize secondary bacterial complications. Antipyretics are recommended for horses with a fever 40°C. Antibiotic therapy is instituted upon suspicion of secondary bacterial infection. Prevention is based on vaccinating at 5, 7, and 9 mo of gestation as well as preventing exposure of pregnant mares to horses attending shows or other equine events
- 2. b) Equine viral arteritis Epizooti c cellulitis Pinkeye Equine typhoid Equine viral arteritis (EVA) is an acute, contagious, viral disease of equids caused by equine arteritis virus (EAV) Natural and experimental host range of EAV is restricted principally to equids, there are very limited data to suggest the virus may also infect alpacas and llamas. There is no evidence that EAV is transmissible to people. EAV invades the upper and lower respiratory tract and multiplies in nasopharyngeal epithelium,tonsillar tissue, bronchial and alveolar macrophages. Infected cells of the monocytic lineage and CD3+ T lymphocytes transport the virus to the regional lymph nodes, where it undergoes a further cycle of replication before being released into the bloodstream. The cell-associated viremia that follows ensures dissemination of EAV throughout the body. Fever Depression Anorexia Leucopenia Supra- or periorbital edema, Nasal discharge, Respiratory distress, Skin rash, Temporary subfertility in affected stallions, Abortion, and infrequently, illness and death in young foals Strains of EAV can cause abortion throughout much of pregnancy (3 mo to more than 10 mo). Abortion may occur late in the acute phase or early in the convalescent phase of the infection, with or without prior clinical signs of EVA Edema, Congestion, and hemorrhages, especially in the subcutis of the limbs and abdomen; excess peritoneal, pleural, and pericardial fluid; and edema and hemorrhage of the intra- abdominal and thoracic lymph nodes and of the small and large intestine, especially the cecum and colon. Aborted fetuses are often partly autolyzed. History of EVA shortly before abortion, virus isolation or PCR of placenta and/or fetal tissues, or by seroconversion of the dam No specific antiviral treatment available Symptomatic treatment (eg, antipyretic, anti- inflammatory, and diuretic drugs) is indicated only in severe cases, especially in stallions. Prevention of EVA is by management to minimize viral transmission in breeding populations and to prevent development of carrier stallions. Vaccinaiton of non- pregnant mares c). Bacterial abortion Potomac horse fever caused by Ehrlichiaristicii may be followed by abortion in mid- to late gestation Potomac horse f ever is found throughout in North America and has been reported in most regions of the United States and Canada One route of exposure is believed to be inadvertent ingestion of hatched aquatic insects that carry N risticii in the metacercarial stage of a trematode. The incubation period is ~10–18 days Mild depression Anorexia, followed by a fever of 38.9°– 41.7°C placentitis and the placenta is often retained Histologically, there is fetal colitis PCR oxytetracycline (6.6 mg/kg, IV, bid) fluids NSAIDs There is a vaccine for Potomac horse fever, but its efficacy in preventing abortion is not known. Leptospir osis Most fetuses are aborted after 6 mo of gestation and the Leptospirosis is responsible for 2–4% of all There are no gross lesions in the fetus or luorescent antibody staining of placenta or fetal kidney, liver, or lung Antibiotics have not been shown to significantly reduce the There are no leptospiral vaccines for horses.
- 3. mares are usually healthy. Infection does not appear to spread horse-to-horse, and often only a single mare on a farm aborts equine abortions annually, although high rainfall and flooding may result in abortion outbreaks. placenta, but microscopically there is suppurativeplace ntitis and by fetal serology. shedding period. In acute disease, systemic antibiotics are useful, and antibiotics are also used to prevent further abortions in co-housed or exposed pregnant mares Brucellos is It is commonly called fistulous withers or poll evil. The disease is prevalent in most countries of the world. It primarily affects cattle, buffalo, bison, pigs, sheep, goats, dogs, elk, and occasionally horses. The disease in people, sometimes referred to as undulant fever WhenBrucellaabortus is ingested, the bacteria travel through the oral mucosa to the regional lymph nodes. Infection leads to bacteraemia, which is usually transient; the organisms ultimately settle in the reproductive tissues or musculoskeletal system. late abortions in mares, Generalized illness marked by fever, stiffness, and lethargy may be seen. Suppurative bursitis, a pus- filled inflammation of connective tissue over the shoulders or poll. Affected bursae have thickened capsule and clear fluid, unless fistulated in which case exudates is usually purulent. Osteomyelitis of dorsal spinous process may present Isolation of Brucella spp. Serological test. Fistulous withers may also result from infection of the supraspinous bursa by other agents, usually secondary to trauma or penetration of a foreign body Other causes of abortion and fever. Treatment is unsuccessful because of the intracellular sequestration of the organisms in lymph nodes, the mammary gland, and reproductive organs. NSAIDS to reduce fever and inflammation such as flunixinmeglumine or phenyl butazone Horses should not be housed or pastured with seropositive cattle. Trauma is considered to be a predisposing factor for the development of fistulous withers, properly-fitting saddles and tack should always be used. reduce the incidence of Onchocercaspp. Vaccination with strain 19 vaccine Cystic ovary disease The presence of persistent follicles, anovulatory follicles or cystic structures on the ovary accompanied by pathological condition. When diagnosing, it must be remembered that normal follicle size during estrus is 4–6 cm in diameter it is most common in cattle, particularly the dairy breeds, but it occurs sporadically in dogs, cats, pigs, and perhaps mares Ovulation failure can also be found in mares that are having irregular estrous cycles during the spring or fall transition phases of the reproductive cycle Presence of persistent follicles The granulosa cell tumor condition in mares causes marked enlargement of one ovary. The condition is diagnosed mainly through rectal palpation where the presence of cysts can be felt on ovaries. Ultrasound Difficult to treat Surgical removal of the cyst of the affected ovary. Equine coital Enxanthe ma Genital horse pox Equine coital exanthema (ECE) is an infectious, venereally transmitted Occasionally stallions are more severely affected than Equine coital exanthema (ECE) is a predominantly sexually-transmitted Dull Anorectic‘ Febrile Vesicles appear within 2-5 days on the penis and Based on clinical signs Serology Virus isolation Demonstration of viral Trauma Early squamous cell carcinoma When infection is suspected or diagnosed in a stallion, mating
- 4. mucocutaneous disease of mares and stallions caused by a herpesvirus. The disease is characterised by the development of superficial pock-like eruptions and erosions or ulcers on the external genital organs. Incubation period: 2- 10 days Transmission : Venereal mares. The disease is generally limited to reproductive tract. The virus is endemic in UK and most horse breeding populations internationally. disease caused by infection with EquidHerpesvirus 3 (EHV-3), a highly contagious but otherwise non- invasive and relatively benign virus. later on the prepuce Mares develop multifocal areas of sharply demarcated vulvar erosions that develop into scabs which then slough leaving ulcerated areas up to 1.5 cm in diameter. Lesions rarely occur on the nasal and oral mucosa. DNA in the skin lesion Frostbite Habronemiasis bacterial infection. should cease until the stallion is confirmed free of disease Sanitation A commercial vaccine against ECE has not been developed. Mastitis Mastitis is inflammation of the mammary gland and is almost always due to a bacterial infection. Streptococcus zooepidemicus is the most frequent pathogen, but S equi, S equisimilis,Sagalactiae , and S viridans are also found. Acute mastitis occurs occasionally in lactating mares, most commonly in the drying-off period, in one or both glands. Infectious organism can colonize the mammary gland tissue by routes that are; hematogenous, percutaneous or ascending. Establishment of infection and production of disease state depend on virulence of organism, ability of local defense mechanism, Ascending infection can occur via the teat canal, or a breach in the mammary gland integument. Warm, swollen and painful udder Edema on the abdomen in front of the udder Other signs of illness such as fever and depression may occur Suppurous lactation secretion An increased degenerated and non-degenerated neutrophils and necrotic debris. Physical examination Bacterial isolation and sensitivity test. Histopathology – mammary gland biopsy may be helpful Cushing disease Edema near the mammary gland may also be a symptom of other conditions, such as a viral infection, liver disease, immune disorders or other problems. Frequent hand milking to remove inflammatory cells, fluid and bacteria.. Chemotherapy:Trimeth oprim-ulfonamide combination of penicillin (20,000 IU/kg, IM, bid) and gentamicin sulfate (2 mg/kg, IV, tid) To help prevent mastitis, check udders often, and be aware of each mare‘s udder appearance— and note abnormal changes, especially in lactating mares. Avoid any unnecessary handling of the udder and make sure your hands are clean (or wear sterile gloves). Contagio us equine Metritis Contagious equine metritis (CEM) is an acute, highly contagious venereal disease of horses. CEM is caused by the The disease occurs primarily in Europe, but technical challenges in propagation of CEM is transmitted primarily at mating, but infected fomites (instruments and equipment) also play a role Copious mucopurulent discharges in mares. Chronically infected mares show no signs. Most mares don‘t Edema and hyperemia of endometrium, endocervix and vaginal mucosa. Microscopic Isolation of causative organism. Serological tests. o Chlorhexidine o Nitrofurazone o Surgical excision of clitoral sinuses may be required to rid them of infection. Control of CEM depends on identification of infected carrier animal and on their treatment or
- 5. gram-negative, microaerophiliccoccob acillus Taylorellaequig enitalis, also known as the contagious equine metritis organism (CEMO). the causative organism prevent accurate determination of the precise distribution of the disease. conceive at the time of infected mating. lesions include invasion of affected tissue by neutrophils during acute stage and by macrophages, lymphocytes and plasma cells later in the course of infection elimination from breeding program. Strict import regulation CONGENITAL & INHERITED ANOMALIES OF REPRODUCTIVE SYSTEM Cryptorch idism rig Failure of one or both testicles to descend into the scrotum and is seen in all domestic animals. It is the most common disorder of sexual development in horses. Bilateral cryptorchidism results in sterility. Unilateral cryptorchidism is more common Cryptorchids are classified as ‗abdominal‘ or ‗inguinal‘, depending on the location of the retained testicle.Inguinal retention is by far the more common of the two. It is common in stallions and boars and is the most common disorder of sexual development in dogs. All breeds of horses may be exhibit cryptorchidism, but there is a higher frequency in Quarter Horses, Saddlebreds, Percherons, and ponies. As the foetus develops, the testicles start to descend towards the inguinal canal and usually pass through the canal and into the scrotum during the final weeks of pregnancy. The testicle can be retained anywhere along its descentThe condition is likely the result of a complex combination of genetic, hormonal, and mechanical factors. Physical examination None The condition is considered heritable, so affected pets should be castrated to help prevent continuation of this congenital defect. Retained Fetal Membran e Equine fetal membranes are normally expelled within 3 hours after parturition, but Mares that have retained their fetal membranes appear to be at The cause of retention of fetal membranes often is not known, but the condition is Non-expulsion of the fetal membrane after 3 hours. It is common practice to administer oxytocin (5 U, IM, every 2–3 hr) beginning 3–4 hr after parturition if the In cases of prolonged retention of fetal membranes, antimicrobials should be administered
- 6. expulsion may be delayed for 8–12 hours or even longer without signs of illness. increased risk of recurrence of the condition, and Friesian mares may be particularly predisposed. Retention of just a portion of the fetal membranes entirely within the uterus (usually at the tip of the previously nongravid uterine horn) is less conspicuous but equally likely to result in complications. For this reason, the chorionic surface of the expelled membranes should be examined to ensure that they have been completely expelled. associated with infection, abortion, short or prolonged gestation, uterine atony, and dystocia. Retention of fetal membranes may mediate development of metritis or even peritonitis. Laminitis is a potential sequela. membranes have not yet been expelled. Manual removal of retained membranes carries the risk of uterine damage or prolapse and is not recommended beyond gentle tugging to displace already loosened membranes. prophylactically, along with NSAID and other therapeutic strategies aimed at preventing laminitis Uterine Prolapse and Eversion Prolapse of the uterus invariably occurs immediately after or within several hours of parturition, when the cervix is open and the uterus lacks tone. It is rare in mares Invagination of the tip of the uterus, excessive traction to relieve dystocia or retained fetal membranes, uterine atony, hypocalcemia, and lack of exercise have Replacement of the prolapsed uterus in mares is usually done with the mare sedated but standing, taking care not to perforate the uterus. Treatment involves Complications tend to develop when laceration, necrosis, and infection occur, or when treatment is delayed. Shock, hemorrhage, and thromboembolism are potential sequelae of
- 7. all been incriminated as contributory causes. removing the placenta (if still attached), thoroughly cleaning the endometrial surface, and repairing any lacerations. Rubbing the surface of the uterus with glycerol helps reduce edema and provides lubrication. The uterus is then returned to its normal position. An epidural anesthetic should be administered first. The cleansed uterus should be elevated to the level of the vulva on a tray or hammock supported by assistants, and then replaced by applying steady pressure beginning at the cervical portion (or at the level of the invagination of the non- prolapsed uterine horn) and gradually working toward the apex. Once the uterus is replaced, a hand should be inserted to the tip of both uterine horns to be sure that there is no remaining invagination that could incite abdominal straining and another prolapse. Installation of warm, sterile saline solution is useful for ensuring complete replacement of the tip of the uterine horn without a prolonged prolapse. In some instances, the bladder and intestines may prolapse into the everted uterus. These require careful replacement before the uterus is replaced. The bladder may be drained with a catheter or needle passed through the uterine wall. Elevation of the hindquarters and pressure on the uterus aid in replacement of bladder and intestines. It may be necessary to incise the uterus carefully (in a longitudinal direction) to replace these organs. Supportive treatment and antibiotic therapy are indicated.
- 8. trauma. Vaginal and Cervical Prolapse Cervicovaginal prolapse is more common in stabled than in pastured animals, suggesting that lack of exercise may be a contributing factor. Predisposing factors include increased intra-abdominal pressure associated with increased size of the pregnant uterus, intra-abdominal fat, or rumen distention superimposed upon relaxation and softening of the pelvic girdle and associated soft-tissue structures in the pelvic canal and perineum mediated by increased circulating concentrations of estrogens and relaxin during late pregnancy. Intra- abdominal pressure is increased in recumbent animals. The prolapse begins as an intussusception-like folding of the vaginal floor just cranial to the vestibulovaginal junction. Discomfort caused by this eversion, coupled with irritation and swelling of the exposed mucosa, results in straining and more extensive prolapse. Eventually the entire vagina may be prolapsed, with the cervix For replacement of the prolapsed vagina, an epidural anesthetic is first administered. The organ is washed and rinsed, and the bladder is emptied if necessary. Usually, this can be achieved by elevating the prolapsus to allow straightening of the urethra; occasionally, needle puncture through the vaginal wall may be necessary. The vagina is well lubricated (glycerol provides lubrication and reduces congestion and edema by osmotic action) and replaced and then held in position until it feels warm again. Retention is achieved by insertion of a Buhner suture—a deeply buried, circumferential suture placed around the vestibulum to provide support at the point at which the initial eversion of the vaginal wall occurs. The Buhner suture has largely superseded earlier attempts to prevent prolapse by various patterns of sutures in the vulvar lips (which do not prevent the initial eversion of the vagina into the vestibulum) or Permanent fixation techniques (cervicopexy or vaginopexy) in which the cervix or vaginal wall is anchored to other pelvic structures have been described. They may be useful in individual cases of chronic or recurrent prolapse, but most cases are resolved by a well- placed Buhner suture.
- 9. conspicuous at the most caudal part of the prolapsus. The bladder or loops of intestine may be contained within the prolapsed vagina. As the bladder moves into the prolapsed vagina, the urethra may be occluded. The bladder then fills and enlarges, which hinders replacement of the prolapsed vagina unless the bladder is first drained. The bladder may even rupture with potentially fatal consequences. by methods that relied on placement of a retention device within the vagina (which tend to cause discomfort and further straining). Buhner sutures should generally be removed before parturition to prevent extensive laceration. Although the cervical os may be edematous and inflamed, cervicovaginal prolapse seldom interrupts pregnancy and does not specifically predispose to dystocia or postpartum uterine prolapse, which has a different etiology. Vulvitis and Vaginitis Contusion and hematoma of the vagina are noted infrequently after parturition in all species but particularly in mares and sows. Necrotic vaginitis, vestibulitis, and vulvitis may follow dystocia in all species. Possible consequences of necrotic vaginitis include permanent stricture of the vagina, transvaginal adhesions, or perivaginalabscessatio n. Onset of signs, consisting of arched back, elevated tail, anorexia, dysuria, straining, vulvar and perivulvar swelling, and possibly a fetid, serous discharge, begins within 1–4 days of parturition and may persist for 2–4 wk. . In most cases, only gentle and conservative treatment is needed. Prophylactic antibiotic treatment is wise because clostridial or other organisms may proliferate in the damaged tissue and cause tetanus, blackleg, or other forms of clostridial myositis.
- 10. Mammary Tumors The cause of mammary tumors is unknown Mammary tumors are rare in mares Hormones play an important role in the hyperplasia and neoplasia of mammary tissue, but the exact mechanism is unknown. Estrogen or progesterone receptors (or both) have been reported on mammary tumor cells in animals; these may influence the pathogenesis of hormone-induced mammary neoplasia as well as the response to hormone therapy. A mammary tumor is usually suspected on detection of a mass during physical examination. The length of time the mass has been present is usually unknown, but the rate of growth may be helpful in determining prognosis. Palpation of the regional lymph nodes can help determine the extent of spread. Thoracic radiographs, preferably 3 views (a ventral-dorsal and 2 laterals), should be taken to detect pulmonary metastases. Fine-needle aspirates may differentiate between inflammatory and neoplastic lesions but may lead to erroneous conclusions and delay of surgery. The diagnosis is determined by histopathology and is important in defining treatment and prognosis. From a practical view, all mammary tumors should be regarded as potentially malignant regardless of the size or number of glands involved. Mammary tumors are treated surgically, although there is no consensus as to the best procedure. Removal of the tumor alone (lumpectomy), simple mastectomy (removal of the affected gland only), modified radical mastectomy (removal of the affected gland and those that share lymphatic drainage and associated lymph nodes), and radical mastectomy (removal of the entire mammary chain and associated lymph nodes) all have their proponents. In theory, the use of anticancer drugs to combat micrometastatic disease (adjuvant chemotherapy) is a reasonable consideration. Neither radiation therapy nor antiestrogenic compounds have been effective. Dourine Dourine is an often chronic venereal disease of horses that is transmitted during The disease is recognized on the Mediterranean Signs may develop over weeks or months. Early signs include Characteristic plaques 2–10 cm in diameter appear on the Demonstration of trypanosomes from urethral or vaginal discharges, skin plaques, Quinapyramine sulfate (curative), Quinapyraminedimethyl sulfate(prophylactic), When eradication is required, strict control of breeding and elimination of stray
- 11. coitus and caused byTequiperdum. coast of Africa and in the Middle East, southern Africa, and South America; distribution is probably wider. Mortality in untreated cases is 50–70%. mucopurulentdischar ge from the urethra in stallions and from the vagina in mares, followed by gross edema of the genitalia. skin, and the horse becomes progressively emaciated. or peripheral blood is difficult unless the material is centrifuged. Infected horses can be detected with the complement fixation test but only in areas where T evansi or T brucei are not found because they have common antigens. An ELISA test may become available for diagnosis. horses has been successful. Alternatively, infected horses may be identified using the complement fixation test; euthanasia is mandatory. References: Buckelew, Thomas P. Parasitology Images: An Auto-tutorial with Additional Instructional Aids. California University of Pennsylvania. Retrieved from: ―http://workforce.calu.edu/Buckelew/trypanosoma_equiperdum _from_the.htm‖.Retrieved on: 29 December 2013. Buergelt, C.D., & Del Piero, Fabio.2014.Color atlas of equine pathology.USA: Jhon Wiley and sons, inc. Carleton, C.L. Equine theriogenology. Blackwell‘s five minute veterinary consult clinical companion Eilts, Bruce. (2009).Equine Pregnancy.School of Veterinary Medicine.Louisiana State University. Baton Rouge, LA. Retrieved From: ―http://www.vetmed.lsu.edu/eiltslotus/ theriogenology-5361/equine%20pregnancy_2.htm‖. Retrieved on : 29 December 2013. Eilts, Bruce. (2007).Non-infectious Infertility.School of Veterinary Medicine.Louisiana State University. Baton Rouge, LA. Retrieved From: ―http://www.vetmed.lsu.edu/eiltslotus/ theriogenology-5361/cannine%20noninfection%20_2.htm‖. Retrieved on : 29 December 2013. Gilbert, Robert O. (2012). Overview of Mammary Tumors.The Merck Veterinary Manual. Retrieved from: ―http://www.merckmanuals.com/vet/reproductive_system/ mammary_tumors/overview_of_mammary_tumors.html‖. Retrieved on: 04 December 2013. Gilbert, Robert O. (2012). Overview of Uterine Prolapse and Eversion. The Merck Veterinary Manual. Retrieved From: ―http://www.merckmanuals.com/vet/ reproductive_system/uterine_prolapse_and_eversion/overview_of_uterine_prolapse_and_eversion.html‖. Retrieved on: 04 December 2013. Gilbert, Robert O. (2012). Overview of Vaginal and Cervical Prolapse.The Merck Veterinary Manual. Retrieved from: ―http://www.merckmanuals.com/vet/reproductive_system/ vaginal_and_cervical_prolapse/overview_of_vaginal_and_cervical_prolapse.html‖. Retrieved on: 04 December 2013.
- 12. Gilbert, Robert O. (2012). Overview of Vulvitis and Vaginitis in Large Animals.The Merck Veterinary Manual. Retrieved from:―http://www.merckmanuals.com/vet/reproductive _system/vulvitis_and_vaginitis_in_large_animals/overview_of_vulvitis_and_vaginitis_in_large_animals.html‖. Retrieved on: 04 December 2013. Gilbert, Robert O. (2012). Retained Fetal Membranes in Mares.The Merck Veterinary Manual. Retrieved from: ―http://www.merckmanuals.com/vet/reproductive_system/retained_fetal_membranes_in_large_animals/ retained_fetal_membranes_in_mares.html?qt=retained%20fetal%20membrane&alt=sh‖. Retrieved on: 04 December 2013. Holmes, Peter H. (2011). Trypanosomiasis.The Merck Veterinary Manual. Retrieved from:―http://www.merckmanuals.com/vet/circulatory_system/blood_parasites/trypanosomiasis.html?qt=dourine&alt=sh‖. Retrieved on: 04 December 2013. Kahn, C.M. 2010. The Merck veterinary manual.10th Ed. USA: Merk and Co., Inc. Knottenbelt, DC; Pascoe, PR. (2003).Color Atlas of Diseases and Disorders of the Horse. Saunders. Philadelphia, USA. pp.386-7. Mair, T.S., &Diver,T.J. Brucellosis in the horse. Bell Equine Veterinary Clinic, Mereworth, Maidstone, Kent ME18 5GS, UK; and †Department of Clinical Sciences, College of Veterinary Medicine, Cornell University, Ithaca, New York 14853, USA. Retrived on December 09. 2013 @http://www.bellequine.co.uk/downloads/275-280_eve_man_08-027_mair.pdf Abortion.School of veterinary medicine.Louisiana state university. McCue, P.M. Mastitis in mares. Equine reproduction laboratory.Colarado State University.Retrived December 09,2013 @ http://csu-cvmbs.colostate.edu/Documents/Learnmares46-reprodprob-mastitis-apr09.pdf Munroe, Graham A.; Weese, J. Scott. (2011). Equine Clinical Medicine, Surgery and Reproduction.Manson Publishing. London, UK. p.290. Opperdoes, Fred. (1997). Trypanosomes Infecting Man and Animals. De Duve Institute. Retrieved from: ―http://www.icp.ucl.ac.be/~opperd/parasites/tryps2.htm‖.Retrieved on: 29 December 2013. Orsini, James A; Divers, Thomas J. (2014). Equine Emergencies: Treatment and Procedures , 4th Ed. Elsevier. St. Louis, MO. p.440. Pozor, Malgorzata. (2013). Equine placenta – marvelous organ and a lethal weapon.Retrieved from: ―http://extension.vetmed.ufl.edu/files/2013/01/Equine-placenta-marvelous-organ-and-a-lethal-weapon-updated-on-Jan-29- 2.pdf‖.Retrieved on: 24 December 2013. Radostits, O.M.,et al. 2007.Veterinary medicine: a textbook of diseases of cattle, sheeps, goats, pigs and horses. 10th Ed. Saunders Ltd. Sorden, Steve; Andreasen, Claire. (2013). Disease Images: Dourine. The Center for Food Security and Public Health. Retrieved from: ―http://www.cfsph.iastate.edu/ DiseaseInfo/disease-images.php?name=dourine‖. Retrieved on : 29 December 2013. Spadari, A.; Valentini, S.; Sarli, G.; Spinella, G.; Millanta, F. (2008). Mammary Adenoma in a Mare: Clinical, Histopahtological and Immunohistochemical Findings. Equine Veterinary Education, 20: 4–7. doi: 10.2746/095777308X258982
