Presentation1.pptx, ultrasound examination of the appendix.
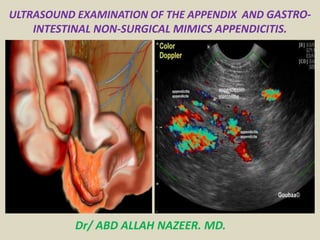
- 1. ULTRASOUND EXAMINATION OF THE APPENDIX AND GASTRO- INTESTINAL NON-SURGICAL MIMICS APPENDICITIS. Dr/ ABD ALLAH NAZEER. MD.
- 2. ULTRASOUND OF THE APPENDIX PROTOCOL Indications Focal RIF pain Rebound tenderness Pelvic pain Elevated WCC (white cell count) LIMITATIONS Bowel gas and patient habitus are the biggest limiting factors to visualizing the appendix. Up to 60% of appendix' are retrocaecal and thus may be obscured. Not identifying an appendix does NOT exclude appendicitis. PREPARATION Ideally the patient has fasted for 6 hrs. Water in the bladder is an advantage to rule out ovarian pathology. Unfortunately the appendix is usually an urgent "fit in" and the preparation cannot always be adhered to. EQUIPMENT SELECTION AND TECHNIQUE Use of a high resolution probe (7-15MHZ) is essential. Beam steering or compounding can help to overcome anisotropy in linear structures such as tendons. Good colour / power / Doppler capabilities. Be prepared to change frequency output of probe (or probes) to adequately assess both superficial and deeper structures.
- 3. SCANNING TECHNIQUE Finding the appendix is highly sonographer dependent. They must have a good skill level to undertake this examination. begins by placing the transducer in a transverse position and applying deep graded compression to the displace the gas and bring the bowel closer to the probe. Beginning at the hepatic flexure the bowel is traced down to the cecum. The patient should point to the location of pain . It is a good idea to have a protocol which includes the entire pelvis of all females with right lower quadrant pain and scanning the renal and biliary systems of all patients with a normal appendix. Sometimes the external iliac artery and vein can provide a good landmark for finding the appendix because of the location and pulsatility, compressible, and having Doppler flow.
- 4. ULTRASOUND CRITERIA TO DIAGNOSE APPENDICITIS In order to demonstrate all the possible presentations of appendicitis it is important that the entire appendix is visualized when the outer diameter of the appendix measures greater than 6 mm Echogenic inflammatory periappendiceal fat change The wall thickness can measure almost 3 mm or greater progressed appendicitis can demonstrate a gangrenous appendix. The lumen distends tremendously sometime upwards to 2 cm and is not compressible. An appendicolith may be present which will cast an acoustic shadow. An appendicolith may be present which will cast an acoustic shadow or a perforated appendix is demonstrated when the appendicular wall has ruptured producing fluid or a newly formed abscess. The appearance is hyperechoic with an echo-poor abscess surrounding the appendix. There may be a reflective omentum around the appendix, a thickened bowel, and enlarged lymph nodes. Asymmetrical wall thickening may indicate perforation. free fluid in the periappendiceal region.
- 5. DIFFERENTIAL DIAGNOSES VISIBLE ON ULTRASOUND: Ovarian abnormality •Mesenteric adenitis •Renal calculi COMMON PATHOLOGY: •Appendicitis •Mesenteric Adenitis •Ovarian pathology •Crohn's disease •Diverticulitis •Abscess
- 6. ULTRASOUND OF THE APPENDIX – Normal. NORMAL APPENDIX POSITIONS Visualization of the apex in its entirety is required because appendicitis will may only affect the tip.
- 7. Refer to this study which concluded that the location of the appendix has wide individual variability, and the limitations of McBurney's point as an anatomic landmark should be recognised. The appendix can be found from the groin, to the umbilicus or even higher under the liver. It is rarely midline or in the left iliac fossa.
- 8. Appendicitis can be diagnosed when the outer diameter of the appendix measures greater than 6mm. Normal Appendix.
- 9. This image highlilghts the position of the cecum and the appendix (mouseover).
- 10. Normal appendix. A and B, longitudinal (A) and transverse (B) sonogram, showing the appendix (arrowheads) with a diameter less than the 7 mm cut-off point, surrounded by normal non-inflamed fat.
- 11. Appendicitis. Longitudinal and transverse sonogram show an enlarged appendix (arrows) surrounded by hyperechoic inflamed fat (arrowheads).
- 12. Appendicitis with appendicolith and color as well as energy Doppler US images.
- 13. Focal appendicitis. (A) Longitudinal color Doppler image of right lower quadrant demonstrates enlarged and hyperemic appendiceal tip (arrow) with normal appearing proximal appendix. (B) Transverse view of right lower quadrant image shows enlarged appendiceal tip (arrow).
- 14. Acute appendicitis. (A) Long axis view through the right lower quadrant demonstrates a noncompressible, enlarged, fluid-filled blind-ending appendix (arrow). (B) Short axis scan shows a target appearance characterized by a fluid-filled center, subadjacent layer of hyperechoic mucosa, and outer layer of hypoechoic muscle (arrow).
- 15. Acute appendicitis with increased blood flow at Doppler images.
- 16. Inflamed appendix at sonography. Longitudinal (A) and transverse (B) cross-section show a distended noncompressible appendix, surrounded by hyperechoic inflamed fat (arrowheads).
- 17. Ultrasound image obtained near in an oblique plane shows an echovoid fluid collection (A) representing a small abscess adjacent to a portion of the abnormal appendix (large arrows). Appendicitis complicated by an appendiceal abscess.
- 18. Appendiceal abscess with a collection in the right iliac fossa with very well visualized inflamed appendix.
- 19. Right lower quadrant in longitudinal plane, shows an enlarged, non-compressible appendix (small arrows), which contains appendicoliths (large arrow). Note that the walls of the appendix are asymmetric, thicker posteriorly than anteriorly, and there is loss of the expected multilayered appearance. These findings may be associated with perforated appendicitis. Perforated appendicitis on US. Dual gray scale compression US image (right plot before compression; left plot during compression) showing an uncompressible distended appendix (cursors) surrounded by a fluid collection (arrows).
- 20. Perforated appendicitis. (A) Short axis view through right lower quadrant demonstrates enlarged appendix (arrowhead) with surrounding collection in right iliac fossa and appendicolith (arrow) in the fluid collection consistent with perforated appendix. (B) Color Doppler image in another patient shows complex collection (arrow) in right iliac fossa without internal vascularity consistent with abscess secondary to appendicular perforation
- 21. Perforated appendix or appendiceal perforation.
- 22. View full size version of Retro-cecal chronic appendicitis.
- 25. Gastrointestinal nonsurgical mimics of Appendicitis Mesenteric adenitis Mesenteric adenitis has been reported to be the second most common cause of right lower quadrant pain after appendicitis, accounting for 2- 14% of the discharge diagnoses in patients with a clinical suspicion of appendicitis. It is defined as a benign self-limiting inflammation of right-sided mesenteric lymph nodes without an identifiable underlying inflammatory process, occurring more often in children than in adults. Sonography and CT show clustered adenopathy.
- 26. Mesenteric adenitis. Sonogram of the right lower quadrant shows a cluster of enlarged mesenteric lymph nodes (arrowheads). The appendix was normal (not shown) and no other abnormalities were found.
- 27. Mesenteric lymphadenopathy. (A) Longitudinal view through the right lower quadrant using graded-compression sonography shows several enlarged, oval- shaped, mesenteric lymph node with echogenic central hilum (arrow). (B) Color Doppler scan in another patient shows an enlarged node (arrow) with central flow
- 28. Bacterial ileocecitis Because adenopathy also frequently occurs with appendicitis, the normal appendix must be confidently visualized on imaging studies before assigning a diagnosis of mesenteric adenitis. Infectious enterocolitis may cause mild symptoms resembling a common viral gastroenteritis, but it may also clinically present with features indistinguishable from appendicitis. This latter presentation may occur in bacterial ileocecitis, caused by Yersinia, Campylobacter, or Salmonella. Imaging studies show mural thickening of the terminal ileum and cecum without inflammation of the surrounding fat , and moderate mesenteric adenopathy.
- 29. Bacterial ileocecitis. A and B, Sonography shows moderate mural thickening of the terminal ileum and cecum, surrounded by normal noninflamed fat. Moderate mesenteric lymphadenopathy was also present (not shown).
- 30. Yersinia enterocolitis. (A) Longitudinal and (B) axial scan of the right lower quadrant show abnormal ileum with thickened hypoechoic bowel wall (arrows) surrounding central echogenic mucosa. The bowel lumen is collapsed. (C) Color Doppler image shows hyperemic bowel wall
- 31. Epiploic appendagitis Epiploic appendages are small adipose protrusions from the serosal surface of the colon. An epiploic appendage may undergo torsion and secondary inflammation, causing focal abdominal pain that simulates appendicitis when located in the right lower quadrant. Epiploic appendagitis is a self-limiting disease that has been reported in approximately 1% of patients clinically suspected of having appendicitis. Sonography and CT depict an inflamed fatty mass adjacent to the colon, containing a characteristic hyperattenuating ring of thickened visceral peritoneal lining on CT.
- 32. Epiploic appendagitis. A, Sonography of the right lower quadrant reveals a hyperechoic inflamed fatty mass (arrowheads) adjacent to the colon (arrow), at the spot of maximum tenderness. B, On unenhanced CT the fatty lesion contains a characteristic hyperattenuating ring (arrow) corresponding to thickened visceral peritoneal lining.
- 33. Omental infarction Omental infarction has a pathophysiology and clinical presentation similar to that of epiploic appendagitis, with the infarcted fatty tissue being a right-sided segment of the omentum. Imaging shows a cakelike inflamed fatty mass, larger than in epiploic appendagitis and lacking a hyperattenuating ring on CT. Omental infarction. A, Sonography of the right middle abdomen shows a large area of inflamed intraperitoneal fat (arrowheads). B, Unenhanced CT depicts the lesion as a cake-like area of dense inflamed omental fat (arrowheads), larger than in epiploic appendagitis and lacking a hyperattenuating ring.
- 34. Right-sided colonic diverticulitis Right-sided colonic diverticulitis may clinically mimic appendicitis or cholecystitis, though the patient's history is generally more protracted. In contrast to sigmoid diverticula, right-sided colonic diverticula are usually true diverticula, that is, outpouchings of the colonic wall containing all layers of the wall. This may possibly explain the essentially benign self- limiting character of right-sided diverticulitis. Sonography and CT findings consist of inflammatory changes in the pericolic fat with segmental thickening of the colonic wall, at the level of an inflamed diverticulum.
- 35. Right-sided colonic diverticulitis. A, Unenhanced CT shows extensive with fat-standing along the cecal wall (arrowheads), and a normal appendix (arrow). B, Sonography reveals the cause of the inflammation by depicting an inflamed cecal diverticulum (arrow) centred in the hyperechoic fat.
- 36. Crohn disease Crohn disease often causes long-standing symptoms, but up to one third of patients with ileocecal Crohn disease present with initial symptoms so acute that they are misdiagnosed as appendicitis. In the acute active phase of ileocecal Crohn disease, imaging shows transmural bowel wall thickening, often predominantly of the submucosal layer, with frequent inflammatory changes of the surrounding fat. Acute ileocecal Crohn disease. A and B, Sonography shows transmural wall thickening of the terminal ileum (arrows) in longitudinal (A) and transverse (B) section, with hyperechoic inflammatory changes of the surrounding fat (arrowheads).C, Contrast-enhanced CT confirms the wall thickening and luminal narrowing of the terminal and pre-terminal ileum (arrowheads), with regional fat-stranding.
- 37. Gynecologic conditions Gynecologic conditions such as pelvic inflammatory disease or a hemorrhagic functional ovarian cyst can cause acute pelvic pain that may simulate appendicitis. In pelvic inflammatory disease the imaging findings vary according to the severity of the disease, and may be normal in early conditions. In more advanced stages, findings may include enlargement of the internal genital organs with indistinct contours, and free pelvic fluid. In absence of a drainable tubo-ovarian abscess, treatment is medically with antibiotics. An hemorrhagic ovarian cysts appears as a complicated cyst at sonography and a high- attenuation adnexal mass at unenhanced CT, and does not require any treatment.
- 38. Pelvic inflammatory disease. A, Endovaginal sonography shows an inhomogeneously enlarged right ovary (arrowheads).B and C, Contrast- enhanced CT shows enlargement of the ovaries (B, arrows) with ill-defined contours of the ovaries and uterus, and some free pelvic fluid (C, arrow).
- 39. Color Doppler image through the ovary (red arrowheads) shows absence of blood flow demonstrating ovarian torsion. Ovarian Torsion Whirlpool Sign Ultrasound.
- 40. Urolithiasis Urolithiasis may present with right lower quadrant pain when obstruction is caused by a distal ureteral stone. Unenhanced CT is more accurate in detecting ureteral stones than sonography. Ureteral stone. A and B, Sonography shows right-sided hydronephrosis (A), and an obstructing calculus (B, arrow) in the distal ureter at the level of the iliac vessels.
- 41. Rectus sheath hematoma A rectus sheath hematoma may be easy to diagnose in patients presenting with a painful palpable mass under anticoagulant therapy, however, small nonpalpable hematomas may clinically masquerade as appendicitis and also occur in patients without anticoagulantia. Sonography and CT show a hemorrhagic mass within the sheath of the rectus abdominis muscle. Rectus sheath hematoma. A, Sonography depicts a small painful lesion (arrow) within the sheath of the rectus abdominis muscle in the right lower quadrant. The lesion contains a fluid-fluid level. B, Unenhanced CT depicts the lesion as a partly hyperdense mass (arrow) within the rectus sheath.
- 42. Meckel's diverticulum The omphalomesenteric duct is an in utero structure connecting the mid-gut at the level of the ileum to the yolk sac. It usually involutes in the first trimester. Meckel's diverticulum develops when the ileal end of the duct remains open. Patients may present with abdominal pain due to inflammation or intussusception with the diverticulum as the lead point (see discussion below). At sonography, the inflamed Meckel's diverticulum appears as a hypoechoic tubular or cyst-like structure on the antimesenteric border of the distal ileum Doppler sonography reveals hyperemia of the wall. This appearance can mimic that of appendicitis, but an origin from small bowel rather than cecum should suggest the diagnosis of Meckel's diverticulum. Meckel's diverticulum. (A) Longitudinal view of right lower quadrant shows oval structure (arrow) with central echogenic mucosa and peripheral hypoechoic muscle. (B) Longitudinal view of right lower quadrant shows connection (arrow) of this oval hypoechoic structure with distal ileum (arrow head) Normal appendix was seen separate from the lesion. On surgery, inflamed Meckel's diverticulum was identified.
- 43. Intussusception Intussusception is one of the most common causes of acute abdominal pain in early childhood, typically affecting children between 3 months and 2 years of age. Approximately 90% of intussusceptions are ileocolic; the rest are ileoileocolic, colocolic, or Ileoileal. More than 90% of intussusceptions have no pathologic lead point and are believed to be due to inflammation of Peyer patches (lymphoid tissue in the ileum). Meckel's diverticulum, intestinal polyps, enteric duplication cysts, intramural hematoma, and lymphoma may also cause intussusception. Intussusception. (A) Transverse view through the right mid-abdomen demonstrates a soft-tissue mass. Note the hypoechoic outer rim representing the receiver loop, or intussuscipiens. The central region, or intussusceptum, has loops of bowel and echogenic mesenteric fat and two lymph nodes (arrows) . (B) Longitudinal view shows a reniform shape of the intussuscipiens. (C) Transverse color Doppler image shows normal vascularity in the intestinal wall in intussusceptum and intussuscipiens.
- 44. Vasculitis Henoch-Schφnlein purpura is an idiopathic systemic vasculitis characterized by purpura, abdominal pain, arthralgia, and sometimes nephritis. The common sites of bowel involvement are the proximal jejunum and distal ileum. Abdominal pain can precede the onset of the skin lesions and mimic acute appendicitis. Sonography shows circumferential bowel wall thickening, usually ranging between 5 and 8 mm in diameter Henoch-Schönlein purpura: Long axis of the terminal ileum show thickened echogenic small bowel wall (arrow).
- 45. Thank You.
