Care of patient with cancer thyroid and parathyroid
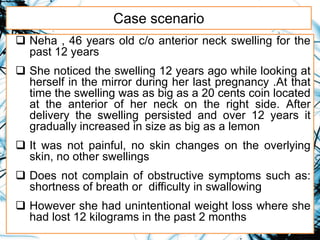
- 1. Case scenario Neha , 46 years old c/o anterior neck swelling for the past 12 years She noticed the swelling 12 years ago while looking at herself in the mirror during her last pregnancy .At that time the swelling was as big as a 20 cents coin located at the anterior of her neck on the right side. After delivery the swelling persisted and over 12 years it gradually increased in size as big as a lemon It was not painful, no skin changes on the overlying skin, no other swellings Does not complain of obstructive symptoms such as: shortness of breath or difficulty in swallowing However she had unintentional weight loss where she had lost 12 kilograms in the past 2 months
- 2. Care of patient with cancer Thyroid and parathyroid Moderator: Dr.L.Gopichandran Lecturer AIIMSCON Presenter: Saumya P.Srivastava Msc.Nsg 2nd year Oncology Nursing AIIMSCON
- 3. Objectives At the end of the class group will be able to: • Introduce the topic • Explain epidemiology of thyroid cancer • Describe anatomy and physiology of thyroid cancer • Enumerate etiology and risk factors associated with thyroid cancer • Elaborate on types of thyroid cancer • Explain pathogenesis of thyroid cancer • Describe classification (TNM, Staging) of thyroid cancer • List down clinical manifestation of the patient with Ca thyroid • Explain diagnostic workup of the patient with ca thyroid • Explain management of thyroid cancer
- 4. Introduction • Thyroid cancers represent approximately 1% of new cancer diagnoses in the United States each year. • Thyroid malignancies are divided into papillary carcinomas (80%), follicular carcinomas (10%), medullary thyroid carcinomas (5-10%), anaplastic carcinomas (1-2%), primary thyroid lymphomas (rare), and primary thyroid sarcomas (rare).
- 5. Cont.. • Hürthle cell carcinoma is a rare thyroid malignancy that is often considered a variant of follicular carcinoma. • Hürthle cell carcinomas account for 2-3% of all thyroid malignancies.
- 6. Epidemiology • Uncommon cancer but most common malignancy of the endocrine system. • The incidence of this malignancy has been increasing over the last decade • Women >men . • Mean age of presentation 40-45 yrs (females), 65-69 yrs (males). • Women are 3 times more likely to develop thyroid cancer than men. • Higher in young age < 40 years • The vast majority of thyroid cancers is highly treatable.
- 7. Epidemiology • Thyroid cancer is the sixth most common cancer in women. • About 2% of cases occur in children and teens. • Men have a worse prognosis than women when there is a diagnosis of thyroid cancer. • Overall, the 5-year survival rate for people with thyroid cancer is 98%. • For localized anaplastic thyroid cancer, the 5-year survival rate is 30%. • In India relative frequency of thyroid cancer 0.1%– 0.2%. • Highest incidence is in Thiruvanantpuram district.
- 8. Thyroid cancer: incidence and deaths in u.s
- 10. Trends in thyroid cancer incidence in India janeesh sekkath veedu, kevin wang et al, J Clin Oncol 36, 2018 • Aim: To investigate the trends in thyroid cancer incidence in India by region, gender and age group. • Methods: data from the Population Based Cancer Registries (PBCRs) compiled by the National Cancer Registry Program (NCRP) of the Government of India. Analyzed data from 14 regions from 2004/05 to 2013/14. • Results: Over a decade, the incidence rate of thyroid cancer in India in women increased from 2.4 to 3.9 and in men from 0.9 to 1.3 per 100,000 persons, a relative increase of 62% and 48% respectively. The relative increase in thyroid cancer incidence in women over 10 years was 121% in age group < 30 years, 107% in age group of 30-44, 50% in 45-59, 15% in 60-74 and 27% in ≥75. Similarly, the greatest relative increase in thyroid cancer incidence in men was in age group < 45. • Conclusions: The incidence of thyroid cancers is rapidly increasing in India particularly among the younger population (age group < 45).
- 12. Anatomy
- 15. Vascular Supply
- 16. Innervation
- 18. Functions of thyroid • It plays a major role in the metabolism, growth and development of the human body • The thyroid gland uses iodine from the diet to make thyroid hormone (thyroxine). • The release of thyroid hormone is controlled by the thyroid stimulating hormone that stimulates the thyroid to make and release more thyroid hormone. • The thyroid gland also secretes a hormone called calcitonin that is produced by the parafollicular cells (also called C cells).
- 20. Control of Thyroid Hormone Synthesis and Secretion
- 21. Etiology and Risk Factors NON- MODIFIABLE : • Gender: 3 times more common in women • Hereditary: Mutations in RET proto-oncogene causing familial medullary thyroid carcinoma (FMTC) and multiple endocrine neoplasia type 2 (MEN 2a and MEN 2b) • Family history: Having a first-degree relative (parent, brother, sister, or child) with thyroid cancer • Race : Asian MODIFIABLE: • Diet low in iodine, H/O Goitre :Follicular thyroid cancers • Radiation exposure: Sources include radiotherapy, X rays, CT scans ,power plant accidents or nuclear weapons. Risk increases with larger doses and with younger age at exposure
- 22. Etiology and Risk Factors • Radiation therapy for hodgkin lymphoma or other form of lymphoma in the head and neck. • Race-White people and Asian people are more likely to develop thyroid cancer. Breast cancer survivors may have a higher risk of thyroid cancer, particularly in the first 5 years after diagnosis and for those diagnosed with breast cancer at a younger age.
- 23. Anaplastic thyroid cancer is usually diagnosed after age 60. Older infants (10 months and older) and adolescents can develop MTC, especially if they carry the RET proto-oncogene mutation.
- 24. Research Input The Risk Factors in the Lifestyles of Thyroid Cancer Patients and Healthy Adults of South Korea Yoo, Yang Gyeong PhD, RN et al Cancer Nursing: January/February 2018 - Volume 41 - Issue 1 - p E48–E56 • Objective: The aim of this study were to identify lifestyle and habit differences in thyroid cancer patients and healthy adults and to investigate risk factors that influence the development of thyroid cancer. • Methods: The study was designed as a retrospective comparison survey study of thyroid cancer patient group and healthy adult group. • Conclusion: Based on the results of this study comparing thyroid cancer patients and healthy adults, it is recommended to encourage an increase in physical activity, minimize both direct and indirect exposure to smoking, develop healthy eating habits of consuming more vegetables, and effectively manage stress levels.
- 25. Types of thyroid cancer Differentiated Thyroid Carcinoma (DTC): 90% » Papillary carcinoma (80%) » Follicular carcinoma (10%): Hurthle cell carcinoma(2-3%) Medullary Thyroid Carcinoma (5- 10%) Anaplastic Carcinoma (1-2%): Undifferentiated
- 26. Other types: (rare) Primary tumours: Sarcomas Lymphomas Epidermoid carcinomas Teratomas. Secondary tumors: Metastasis from lung, breast, and kidney.
- 27. Papillary carcinoma • Papillary carcinoma is the most common thyroid malignancy, representing approximately 80%. • Papillary carcinoma is a slow-growing tumor that arises from the thyroxine (T4)- and thyroglobulin-producing follicular cells of the thyroid. • Women develop papillary cancer 3 times more frequently than men do, and the mean age at presentation is 34-40 years. • Tumors typically appear after a latency period of about 10-20 years. • Increased incidence of papillary cancer is hypothesized among patients with Hashimoto thyroiditis (chronic lymphocytic thyroiditis).
- 28. Papillary carcinoma Pathology: • Histologic feature is the presence of psammoma bodies, which occur in 50% of papillary carcinomas. • Thyrocytes may have so-called "Orphan Annie eyes," ie, large round cells with a dense nucleus and clear cytoplasm • The tumors are unencapsulated neoplasms that characteristically grow with papillae
- 30. Papillary Carcinoma Local invasion: • Tumors can grow directly through the thyroid capsule to invade surrounding structures. • Growth into the trachea can occur, producing hemoptysis. • Extensive involvement can cause airway obstruction. • The recurrent laryngeal nerves can become involved because of their proximity in the tracheoesophageal groove. • Patients present with a hoarse, breathy voice and, occasionally, dysphagia.
- 31. Papillary Carcinoma Regional and metastatic disease- • The most common site of lymph node involvement is in the central compartment (level 6) ,(levels 2-4) are the next most common sites of cervical node involvement. • Lymph nodes in the posterior triangle of the neck (level 5) may also develop metastases. • Approximately 5-10% of patients with papillary thyroid carcinoma develop distant metastases. Distant spread of papillary carcinoma typically affects the lungs and bone.
- 32. Follicular Carcinoma • Second most common thyroid malignancy and represents about 10% of thyroid cancers. • Usually arises in iodine deficient areas. • Similar to papillary carcinoma, follicular carcinoma occurs 3 times more frequently in women than in men. • The mean age range at diagnosis is late in the fourth to sixth decades. • Arise from the follicular cells of the thyroid. • Metastasise to lungs and bones via blood vessel invasion rather via lymphatic system
- 33. Follicular carcinoma Histology: • The tumors appear as round, encapsulated, light brown. • Fibrosis, hemorrhage, and cystic changes are found in the lesions. • Encapsulated lesion and may demonstrate well- defined follicles containing colloid. • The follicular cells in these tumors do not have characteristic features like papillary carcinoma cells. • Immunohistochemical staining for thyroglobulin and cytokeratins is nearly always positive.
- 34. Follicular Carcinoma Local invasion: • Local invasion can occur as it does with papillary carcinoma, with the same presenting features: • Hemoptysis. • Airway obstruction • A hoarse, breathy voice and, occasionally, dysphagia.
- 35. Follicular Carcinoma Cervical and distant metastases: • Unlike papillary carcinoma, cervical metastases from follicular carcinomas are uncommon. • Lung and bone are the most common sites.
- 37. Hurthle cell carcinoma • Rare thyroid malignancy.Variant of follicular carcinoma • Also known as oncocytic carcinoma • Encapsulated thyroid lesion comprising at least 75- 100% Hürthle cells. • Mean age : 50-60 years • Higher risk to metastasise among follicular cancers HISTOLOGY: • Hurthle cells/Oncocytic cells/ Oxyphilic cell : Enlarged cells with abundant eosinophilic granular cytoplasm as a result of accumulation of altered mitochondria.
- 38. Medullary Thyroid Carcinoma • MTCs represent approximately 5% of all thyroid malignancies. • Tumors arise from the parafollicular C cells of the thyroid gland. • About 75% of MTCs occur sporadically, and 25% occur familially. • More aggressive than papillary and follicular cancers. • Usually inherited and associated with MEN (2A and 2B)
- 39. MTC • Mutation of RET proto onco-gene • Age: 5th or 6th decade of life [MTC] 2nd or 3rd decade of life [MTC with MEN] •Elevated serum calcitonin levels > 100 pg/ml •No response to radioactive iodine therapy Histology: • MTCs are fairly well circumscribed, though they are unencapsulated. • Most tumors arise in the middle and upper third of the thyroid lobes. • Calcitonin and carcinoembryonic antigen are microscopically useful for differentiating MTC from other tumors.
- 40. Anaplastic carcinoma • Fastest growing and most aggressive • Less than 2 % of all thyroid cancers • 5 year survival rate < 10% • Presents with a rapidly growing neck mass. Metastases, particularly in the lung present at diagnosis >50% of the time • Peak age of incidence : 6th to 7th decade of life • At least one half of patients already have distant metastases at the time of diagnosis. • The most common sites of involvement are the lungs, bones, and brain.
- 41. Anaplastic carcinoma Pathology: • Anaplastic thyroid carcinoma is a large and invasive tumor. • Areas of focal necrosis and hemorrhage may be present throughout the tumor. • Believed to arise from a preexisting, well differentiated thyroid carcinoma. • Immunohistochemical stains are often positive for low-molecular-weight keratins and occasionally positive for thyroglobulin.
- 42. Primary Thyroid Lymphoma • Represent approximately 2-5% of all thyroid malignancies. • Most thyroid lymphomas are non-Hodgkin B-cell tumors. • The incidence peaks in the sixth decade of life. • This tumor is highly associated with chronic lymphocytic thyroiditis (Hashimoto thyroiditis). • Shows local extension and involvement of the recurrent laryngeal nerve.
- 43. Sarcoma of the Thyroid Gland • They are aggressive tumors that most likely arise from stromal or vascular tissue in the gland. • The treatment for thyroid sarcomas is total thyroidectomy. • Radiation therapy may be used in an adjunctive setting. • Recurrence is common • patient's overall prognosis is poor.
- 44. Pathogenesis
- 46. Staging papillary and follicular carcinoma Patients aged <45 years Stage I Any T, Any N, M0 Stage II Any T, Any N, M1
- 47. Staging papillary and follicular carcinoma Patients aged > 45 years Stage I T1N0M0, T2N0M0 Stage II T1N1M0, T2N1M0, T3 Any N M0 Stage III T4a Any N M0 Stage IV A T4b Any N M0 Stage IV B Any T Any N M1
- 48. T1N0M0, T2N0M0 T1N1M0, T2N1M0, T3 Any N M0
- 49. T4a Any N M0 T4b Any N M0
- 50. Medullary Thyroid Cancer • Stage I: T1, N0, M0 Stage II: T2, N0, M0 ; T3, N0, M0 Stage III: T1–T3, N1a, M0 Stage IVA: T4a, Any N, M0; T1–T3, N1b, M0 Stage IVB: T4b, Any N, M0 Stage IVC: Any T, Any N, M1 •
- 51. Anaplastic thyroid cancer • All patients are considered to have stage IV disease
- 52. Clinical manifestations Early signs: • Lump or swelling in neck • Painless (often), palpable, thyroid nodules ( Hard and fixed nodules) on physical examination • Pain if present may radiate up to ears Late signs: • Hoarseness : Involvement of the recurrent laryngeal nerve and vocal fold paralysis. • Firm cervical masses : Regional lymph node metastases. • Dyspnea or stridor: Tracheal compression • Dysphagia : Esophageal compression • Persistent cough (not due to cold)
- 53. Diagnostic workup • History • Physical Examination: Painless, Hard consistency, Ill- defined borders, Fixed in respect to surrounding tissues, Moves with the trachea at swallowing • Thyroid ultrasound : To examine thyroid nodule and nearby lymph nodes • Ultrasonographically guided fine-needle aspiration biopsy: 80% sensitivity, 100% specificity.Confirmatory • Thyroid scintigraphy (or radio iodine scanning) with I 131 : Malignant nodules appear as cold nodules • Chest Xray : To rule out lung metastases
- 55. Diagnostic workup • CECT or MRI : To assess tumour invasion and lymph node involvement • (PET) or PET-CT scanning : Recurrent cancers when tumor markers are positive and negative anatomic imaging • Laryngoscopy (direct or indirect) : For vocal cord examination • Biopsy: cells are removed from the nodule that are then examined by a cytopathologist. This test is often done with the help of ultrasound. Fine needle aspiration, Surgical biopsy.
- 56. PET-CT SCAN
- 57. Diagnostic workup • Molecular testing of the nodule sample:This is done to identify specific genes, proteins, and other factors unique to the tumor. • Blood tests: Thyroid function studies : To assess thyroid function. Thyroglobulin(Tg and TgAb): Elevated Serum calcium and calcitonin : Elevated in medullary carcinoma Carcinoembryonic antigen (CEA) : Positive in medullary thyroid cancers (>3 ng/dl)
- 58. Diagnostic Workup Radionuclide scanning: • This test may also be called a whole-body scan. • The scan will either be done using a very small, harmless amount of radioactive iodine I-131 or I- 123, called a tracer. • The patient swallows the tracer, which is absorbed by thyroid cells. This makes the thyroid cells appear on the scan image. • TECHNETIUM 99m, I123, DMSA AND MIBG SCAN
- 62. Precautions after RAI therapy • Sleep alone for 3 to 5 nights after treatment, depending on the strength of your dose. • Personal contact with children (hugging or kissing, for example), should be avoided for 3 to 7 days, depending on the strength of your dose. • For the first 3 days after treatment, stay a safe distance away from others (6 feet is enough). Avoid public places and drink plenty of water (to encourage the removal of radioactive iodine through your urine). • For the first three days, do not share items (utensils, bedding, towels, and personal items) with anyone else. Do your laundry and dishwashing separately. Wipe the toilet seat after each use. Wash your hands often, and shower daily.
- 63. Differential diagnosis • Goitre • Grave’s disease • Parathyroid carcinoma • Thyroid nodule • Thyroiditis
- 64. Management • Surgery - Lobectomy - Sub-total thyroidectomy - Near total thyroidectomy - Total thyroidectomy - Extent of neck dissection • Hormonal therapy • Radioactive iodine therapy • EBRT • Chemotherapy
- 65. SURGERY • Surgery is the primary treatment of localised thyroid cancer . • Major surgical approaches are: Lobectomy(Hemithyroidectomy) Subtotal Thyroidectomy Near-total Thyroidectomy Total Thyroidectomy
- 66. Hemithyroidectomy(Lobectomy) • Hemithyroidectomy, or unilateral thyroid lobectomy, refers to removal of half the thyroid gland. • It is typically performed via a transcervical collar incision, but endoscopic and transoral routes have also been described. • The procedure involves mobilization of the thyroid lobe, ligation of thyroid vessels, preservation of parathyroids, protection of the recurrent laryngeal nerve and dissection away from the trachea.
- 67. Lobectomy in the management of thyroid cancer • Age between the age of 15 and 45 years with PTC tumor <4 cm • No prior radiotherapy • No distant metastasis • No cervical LN metastasis • No extrathyroidal extension • Absence of aggressive histologic variant
- 68. Subtotal Thyroidectomy • Subtotal thyroidectomy—Removal of majority of both lobes leaving behind 4-5 grams (equivalent to the size of a normal thyroid gland) of thyroid tissue on one or both sides • This used to be the most common operation for multinodular goitre.
- 69. Near-total Thyroidectomy Near total thyroidectomy:Both lobes are removed except for a small amount of thyroid tissue (on one or both sides) in the vicinity of the recurrent laryngeal nerve entry point and the superior parathyroid gland.
- 70. Total Thyroidectomy • Entire gland is removed. • Done in cases of papillary or follicular carcinoma of thyroid, medullary carcinoma of thyroid. • This is now also the most common operation for multinodular goitre. • video-assisted thyroidectomy and robot-assisted thyroidectomy have recently emerged
- 71. Indications of complete thyroidectomy • Tumor > 4 cm in diameter • Positive margin • Gross extrathyroid extension • Macroscopic multifocal disease • Macroscopic nodal metastasis • Confirmed contralateral disease • Vascular invasion
- 72. Complications related to surgery • Hypothyroidism in up to 50% of patients after ten years • Recurrent laryngeal nerve damage: Unilateral damage results in a hoarse voice. Bilateral damage presents as laryngeal obstruction after surgery and can be a surgical emergency: an emergency tracheostomy may be needed. • Hypoparathyroidism temporary (transient) in many patients, but permanent in about 1-4% of patients • Hypocalcemia
- 73. Cont.. • Wound Infection :Incidence is 0.2-0.5% • Stitch granuloma • Chyle leak • Haemorrhage/Hematoma (This may compress the airway, becoming life-threatening.) • Removal or devascularization of the parathyroids Airway obstruction: In the first 24 hours is most likely from compressive hematoma. After 24 hours consider laryngeal dysfunction secondary to hypocalcemia.
- 74. Neck dissection in thyroid cancer • Cervical lymphadenectomy, or neck dissection, is the treatment of choice when there is evidence of lymph node metastasis from thyroid cancer. • A neck dissection can also be performed "prophylactically" at the time of thyroidectomy to avoid a second operation due to recurrence.
- 75. Recommendation for Neck Dissection • Central compartment ( level VI) is recommended for all patients with clinically involved nodes. • Prophylactic central neck dissection in clinically N0 patients with T3 or T4 tumors • Level I, V, VII should only be dissected when clinically suspicious • Central and lateral neck dissection are part of standard primary therapy for all patients with sporadic and hereditary forms of medullary thyroid cancer
- 76. Complications associated with Neck Dissection Central neck dissection 1) Hypoparathyroidism – temporary/permanent 2) Recurrent laryngeal nerve injury 3) Superior laryngeal nerve injury Lateral neck dissection 1) Hypoparathyroidism – temporary/permanent 2) Chyle leak 3) Hemorrhage 4) Seroma 5) Wound infection 6) Nerve injuries – accessory, ramus mandibularis, sympathetic (Horner’s syndrome), phrenic, brachial plexus, cutaneous cervical
- 77. RADIOACTIVE IODINE ABLATION • If residual disease is found, adjuvant therapy with radioactive iodine (RAI) may be considered. • RAI ablation is indicated for patients with any of the following: • Large (>4 cm) tumors • Known distant metastasis • Gross extrathyroid extension • 4-6 weeks after total thyroidectomy to detect and destroy any metastasis and residual tissue in the thyroid using I131. • For iodine sensitive papillary and follicular cancers
- 78. RAI Therapy
- 79. RAI Therapy RAI ablation is not recommended for the following: • Small (<1 cm), solitary tumors • Multifocal tumors when all foci are < 1 cm Available forms: • I131 is available in the form of: Capsule, Liquid preparation, Intravenous • Capsule is the most common used because of safety and easy of administration
- 80. Patient preparation for I-131 • Low iodine diet: A diet that is low in iodine( <50mcg/day) for 2 weeks before,and 2 days after I- 131- Salty product to be avoided. • Stop thyroid hormone replacement:Levothyroxine and other thyroid replacement should be withheld 6 weeks before I-131. • Lithium carbonate to increase the potency of I-131
- 81. Short-term side effects of RAI treatment • Neck tenderness and swelling • Nausea and vomiting • Swelling and tenderness of the salivary glands • Dry mouth • Taste changes
- 82. Tsh suppression for differentiated thyroid cancer • Rationale- Administration of subtherapeutic doses of T4 in an effort to drive the TSH below detectable limits( < 0.1 Miu/L), thereby decreasing stimulation of residual benign and malignant follicular derived thyroid cells. • 2.5-3.5 mcg/kg of L-T4 every day to inhibit TSH to a value of 0.1-0.5 mU/L • RECOMMENDATION • TSH suppression to just below 0.1 Mu/L for high risk patient. • Maintainance of TSH at or slightly below the lower limit of normal(0.1-0.5 Mu/l) in low risk patients
- 83. Tsh Suppression Limitations • Subclinical and even overt thyrotoxicosis • Tachyarrhythmia • Conduction abnormalities • Ventricular hypertrophy • Systolic and diastolic dysfunction
- 84. External beam radiation therapy • Most often used to treat medullary thyroid cancer and anaplastic thyroid cancer. • Better treatment for cancers that take up iodine. • As palliation for unresectable and metastatic tumors • Dosage:6000-6500 cGy • External beam radiation therapy is usually given 5 days a week for several weeks.
- 85. Toxicity Of EBRT • Acute toxicity • Mucositis • Fibrosis • Pharyngitis • Dysphagia • Hoarseness • Radiation dermatitis • Weight loss • Malnutrition Late Toxicity • Fibrosis and atrophy of skin, lung apices, musculature • Taste changes • Xerostomia
- 86. Chemotherapy • Systemic chemotherapy has no significant role in the management of DTC • Poor response rate on the order of 25- 40% • The most commonly used agent is doxorubicin, either alone or in combination with cisplatin. Palliative chemotherapy:For metastatic and recurrent cancers
- 87. Complications associated with Chemotherapy • Mucositis • Hair loss • Low blood counts • Peripheral neuropathy • Loss of apetite • Ototoxicity
- 88. Targeted therapy Tyrosine kinase inhibitors: Sorafenib , Lenvatinib For iodine resistant papillary and follicular thyroid cancers Tyrosine kinase inhibitors of RET receptor kinase: Vandetanib, Cabozantinib for medullary thyroid cancers
- 89. Side effect of Targeted Therapy • Common side effects include fatigue, rash, loss of appetite, diarrhea, nausea, high blood pressure, and hand foot syndrome (redness, pain, swelling, or blisters on the palms of the hands or soles of the feet.
- 90. Treatment According to type of thyroid cancer Papillary and follicular • Localized: Surgery: Total thyroidectomy, Lobectomy,RAI therapy, Thyroid suppression therapy,EBRT. • Metastatic: Iodine sensitive: RAI therapy, Thyroid suppression therapy • Iodine resistant: Thyroid suppression therapy,Targeted therapy, Surgery, EBRT Medullary thyroid cancer • Localized: Total thyroidectomy , EBRT • Locally advanced and metastatic disease:Targeted therapy, Palliative chemotherapy
- 91. Cont.. Anaplastic thyroid cancer • Surgery, EBRT, Chemotherapy
- 92. Research Input Effect of Comprehensive Nursing Intervention on Thyroid Stimulating Hormone Suppression for Patients with Differentiated Thyroid Cancer Zhou Miaoli et al American Journal of Nursing Science. Vol. 8, No. 1, 2019, pp. 32-35. Objective- to investigate the effect of comprehensive nursing intervention on thyroid stimulating hormone (TSH) suppression for patients with differentiated thyroid cancer (DTC). Method: a total of 90 patients with DTC, receiving 131I treatment in the Department of Nuclear Medicine of the First Affiliated Hospital of Jinan University are enrolled in this study. All patients have received TSH suppression treatment for at least 3 months prior to admission, and are given individual-based comprehensive nursing intervention on TSH suppression after admission. Through questionnaire and telephone follow-up, patients’ awareness of TSH suppression and their medication compliance before and after nursing intervention are analyzed and compared.
- 93. Cont.. Result: the awareness of the knowledge of TSH suppression and medication compliance are significantly improved in 90 patients after comprehensive nursing intervention. Conclusion: Individual-based comprehensive nursing intervention can effectively improve awareness of the knowledge of TSH suppression, medication compliance and confidence in cure in patients with DTC, which helps promote the harmonious relationship between nurses and patients and improve the prognosis of patients.
- 94. Prognosis • Differentiated thyroid cancers: 10 year survival rate > 90%.(Good prognosis) • Hurthle cell carcinoma: 5 year survival rate: 50 - 60%. • Medullary : 10 year survival rate 75-85% • Anaplastic: 5 year survival rate: <10%. (Poor prognosis)
- 95. Prognostic factors (poor prognosis) • Tumour size > 5 cm • Age : Men >40 yrs, Women > 50 yrs • Extrathyroidal invasion • Distant metastases
- 96. Ca Parathyroid
- 97. Objectives At the end of the class group will be able to: • Introduce the topic • Explain epidemiology of parathyroid cancer • Describe anatomy and physiology of parathyroid gland • Enumerate etiology and risk factors associated with parathyroid cancer • Describe classification (TNM, Staging) of parathyroid cancer • List down clinical manifestation of the patient with Ca parathyroid • Explain diagnostic workup of the patient with ca parathyroid • Explain management of parathyroid cancer • Describe nursing management of patient with cancer thyroid and parathyroid
- 98. Introduction • Parathyroid carcinoma is an extremely rare but aggressive and life-threatening form of primary hyperparathyroidism (pHPT). • Most hyperparathyroidism is caused by a single benign adenoma (approximately 85%) or by parathyroid hyperplasia or multiple adenomas. • Parathyroid carcinoma accounts for less than 1% of cases of hyperparathyroidism. • Patients with HPT-JT also have an increased risk of developing parathyroid carcinoma, ranging from 15% to 37.5% in different case series.
- 99. Cont.. • Untreated, parathyroid carcinoma leads to severe hyperparathyroidism, with signs and symptoms including hypercalcemia, bone pain, osteoporosis, fractures, and kidney stones or other renal damage. • Rarely diagnosed preoperatively, PC is often discovered in the treatment of primary hyperparathyroidism
- 100. Anatomy • The parathyroid glands are four or more small glands, about the size of a grain of rice, located on the posterior surface of the thyroid gland. • 4 parathyroid glands, 2 superior and 2 inferior glands; located on the posterior and lateral surface of the thyroid gland. • Arterial supply : Inferior thyroid artery • Lymphatics :deep cervical and pretracheal lymph nodes • Nerve supply: Recurrent laryngeal nerve • Functional cells : Chief cells, which secrete parathyroid hormone
- 101. Function • Parathyroid gland maintains the body’s calcium level within a very narrow range. • PTH works in concert with another hormone, calcitonin, that is produced by the thyroid to maintain calcium homoeostasis. • Parathyroid hormone acts to increase blood calcium levels, while calcitonin acts to decrease blood calcium levels
- 103. Epidemiology • Parathyroid cancer is a rare disease. • More recently the annual incidence has stabilized to a rate of approximately 11 cases per 10 million persons. • Parathyroid cancer occurs equally in males and females. • Males fare slightly worse in prognosis. • Median Age : 44 to 54 years
- 104. Cont.. • Almost all tumors that develop in the parathyroid gland are benign. • They may result in hypercalcemia that is difficult to control or could cause death. • The current 5-year survival rate for people with parathyroid cancer ranges broadly, from 20% to 85%.( Cancer.Net Editorial Board)
- 105. Etiology and risk factors • Unknown in most cases. • Genetic disease [CDC73 mutation]: Hyperparathyroidism–Jaw Tumor (HPT-JT) • Familial isolated hyperparathyroidism. • Primary parathyroid hyperplasia. • History of radiation to the neck
- 106. TNM Classification T (tumor) • (Tx) - No information available • T1 - Evidence of capsular invasion • T2 - Invasion of surrounding soft tissues, excluding the vital organs of the trachea, larynx, and esophagus • T3 - Evidence of vascular invasion • T4 - Invasion of vital organs, such as the hypopharynx, trachea, esophagus, larynx, recurrent laryngeal nerve, carotid artery
- 107. TNM Classification N (node) • (Nx) - Lymph node not assessed • N0 - No regional lymph node metastases • N1 - Regional lymph node metastases M (metastasis) • (Mx) - Distant metastases not assessed • M0 - No evidence of distant metastases • M1 - Evidence of distant metastases
- 108. Classes • Class I - T1 or T2 N0M0 • Class II - T3 N0 M0 • Class III - Any T, N1 M0, or T4 • Class IV - Any N, M1
- 109. High/low risk system Criteria are as follows: • Low risk - Capsular invasion combined with invasion of surrounding soft tissue • High risk - Vascular invasion and/or lymph node metastases and/or invasion of vital organs and/or distant metastases
- 110. Pathology Gross description • May be circumscribed • Gray-white, firm, irregular, may exceed 10 g, may adhere to adjacent structures, rarely within thyroid gland. Microscopic (histologic) description • Uniform cells with minimal atypia in nodular or trabecular patterns with dense fibrous bands • Tumor cells are spindled, mitotic figures are frequent, • Vascular invasion (81% had tumor inside vessel and attached to vessel wall), perineural invasion (19%) and soft tissue invasion usually reliable indicators of malignancy • May produce amyloid • Diffuse nuclear enlargement with macronucleoli suggests malignancy
- 111. The nests of neoplastic cells that are not very pleomorphic. Note the bands of fibrous tissue between the nests.
- 112. Clinical presentation • Palpable central neck mass in combination with hyperparathyroidism or hypercalcemia • Onset: Abrupt Bone pain, pathologic fracture (90% of patients) Renal stones (50-80%) Symptoms of hypercalcemia - Fatigue, weakness, confusion, depression, constipation
- 113. Diagnostic workup Blood tests: • Simultaneous calcium and parathyroid hormone (PTH) levels should be determined. • PTH :3 times the normal limit • Profound hypercalcemia X-ray : • Hand: Subperiosteal bone resorption of the distal phalanges • Skull: Ground glass or Salt and pepper appearance.
- 114. Subperiosteal bone resorption of the distal phalanges Ground glass or Salt and pepper appearance.
- 115. Cont.. • Ultrasonography: Larger, More hypoechoic, Hypervascular, irregular borders, Greater infiltration into surrounding tissues compared to benign lesions • CT and PET scans: To determine metastasis and staging respectively. • Genetic Testing: Genetic testing for germline CDC73 mutation should be considered to rule out HPT-JT. • Histologic Findings: The parathyroid glands are usually large (2-10 g).Tumors are usually encapsulated and often have fibrous septa extending into the gland. The majority of tumors are fibrotic. The parenchyma of the tumor usually has a predominance of chief cells.
- 116. Sestamibi parathyroid scintigraphy • Sestamibi scanning is the preferred way to localize diseased parathyroid glands prior to an operation. • However, sestamibi scans are wrong at least 50% of the time, even at the best places in the world. Tc99m-sestamibi is absorbed faster by a hyperfunctioning parathyroid gland than by a normal parathyroid gland
- 117. Fine-needle aspiration is contraindicated in the workup for parathyroid carcinoma.Diagnosis of parathyroid carcinoma is generally made at the time of surgery.
- 118. Differential diagnosis • Hypercalcemia • Hyperparathyroididsm • Paraneoplastic syndromes • Thyroid nodule
- 119. Treatment and Management • Two kinds of treatment are used: • Surgery and radiation therapy (using high-dose x-rays to kill cancer cells). • Chemotherapy is being studied in a few clinical trials, but there have been no good chemotherapy drugs identified as effective up to this point.
- 120. Treatment and Management • Medical care is limited to the control of hypercalcemia (if necessary). • The diagnosis of parathyroid carcinoma is usually not known prior to surgery. • Unusually severe hyperparathyroidism or a palpable mass should trigger suspicion for parathyroid carcinoma. • Surgery: Parathyroidectomy or En bloc resection of the parathyroid tumor and invaded adjacent tissues, ipsilateral thyroid lobe, and any enlarged lymph nodes
- 121. Parathyroidectomy • Parathyroidectomy is surgery to remove the parathyroid glands or parathyroid tumors. • Most parathyroidectomies are performed for primary hyperparathyroidism. Minimally invasive surgeries: • Minimally invasive parathyroidectomy • Video-assisted parathyroidectomy. • Endoscopic parathyroidectomy
- 122. Parathyroidectomy
- 123. Complications related to Parathyroidectomy • Bleeding and hematoma: Airway compromise • Infection • Injury to recurrent laryngeal nerve: Change in voice • Hypoparathyroidism: Hypocalcemia • Thyrotoxic storm: Due to manipulation of the thyroid gland during surgery • Hypothyroidism
- 124. En bloc resection • Surgery to remove the entire parathyroid gland and the capsule around it. Sometimes lymph nodes, half of the thyroid gland on the same side of the body as the cancer, and muscles, tissues, and a nerve in the neck are also removed. • While en bloc resection results in fewer reoperations for disease, limited data exist on the implications of prophylactic lymph node dissections for PC
- 125. Cont.. • Tumor debulking: A surgical procedure in which as much of the tumor as possible is removed. Some tumors cannot be completely removed.
- 126. The MIRP Procedure (Minimally Invasive Radioguided Parathyroid surgery) • The concept is to make the hyper-active parathyroid cells radioactive with a mild radioactive substance that is absorbed by the overactive cells. • The surgeon operates using a very small (pencil size) radiation detector. • Parathyroid disease is typically cured in under 20 minutes using minimally invasive methods. • All patients can (and should) have minimally- invasive (radioguided) parathyroid surgery...
- 127. Advantages of MIRP • Surgeon has a very good idea which one of the four parathyroid glands is hyperactive prior to beginning the operation. • Allows the surgeon to operate on one very small area of the neck. • Potential risks are expected to be less than that of a complete neck exploration. • The band-aid comes off in one week. There are no stitches to take out. • Does not require an endotracheal tube and deep anesthesia
- 128. Resection of recurrence • Reoperation for local and regional recurrence is indicated and may provide substantial palliation from hypercalcemia, in some cases for many years. • Resection or ablation of pulmonary or hepatic metastases also may provide palliation.
- 129. Adjuvant treatment • Use of Adjuvant therapy is questionable • Fair number of Parathyroid tumors are considered radioresistant. • Cytotoxic chemotherapy is used even less frequently than external beam radiation therapy, and only isolated reports with very small numbers of patients exist.
- 130. Radiation therapy • External beam radiation therapy (EBRT) is controversial. • Postoperative EBRT may decrease local recurrence, but the evidence for this is not strong. • EBRT may also be used in specific circumstances for treatment of a metastasis. • Use of radiotherapy is often restricted to palliative treatment of advanced disease or in the presence of distant disease • In general, however, parathyroid carcinoma is relatively resistant to radiation therapy.
- 131. Management of hypercalcemia • Intravenous hydration with saline and calcium wasting loop diuretic (Furosemide) • IV Bisphosphonates , IV Calcitonin • Cinacalcet : In hypercalcemia refractory to bisphosphonates • Denosumab (120 mg/month): In hypercalcemia resistant to bisphosphonates and cinacalcet.
- 132. Prevention First-degree relatives of patients with parathyroid cancer or HPT-JT should also be genetically screened for CDC73 mutation (when mutation is known) or periodically screened for primary hyperparathyroidism.
- 133. Long-Term Monitoring After surgical treatment, periodic follow-up with serum calcium determinations is mandatory. If serum calcium begins to rise, elevation of parathyroid hormone level can confirm recurrence. • Once suspected, the location of the recurrence should be determined: • Neck imaging with CT scan, MRI, or ultrasound is indicated. • PET scanning may detect distant metastases but its accuracy in this disease is not clearly defined. • A chest radiograph is indicated, but a chest CT scan may reveal pulmonary metastases missed on plain radiograph.
- 134. Prognostic Factors • Prognosis is poor • 2/3rd of patients develop reccurence and 1/3rd can die from tumor progression or refractory hypercalcemia. • Male gender, younger age,higher calcium level are associated with poor prognosis. • Most common site of metastasis are: upper mediastinum, lung, pleura and bone
- 135. Preoperative Assessment: • Explore patient’s feelings and concerns regarding the diagnosis, treatment, and prognosis. • Palpate for mass on the anterior part of neck • Assess for pain on the mass • Assess for dyspnes, dysphagia, hoarseness of voice, stridor • Assess for bruits by auscultation due to increased thyroid vascularity. • Assess for fear, anxiety and concerns regarding the disease condition and treatment
- 136. Preoperative management • The patients should be subjected to fasting for 12 hours and fasting water for 6-8 hours before surgery. • Preoperative cross-matching blood should be prepared for the patients with huge thyroid tumor for use. • Prophylactic antibiotics should be administered before surgery. • Before surgery, the patients with secondary hyperthyroidism should receive oral treatment of Lugol’s iodine solution.
- 137. Psychological Nursing • Doctors and nurses should adopt the ward rounds, health education and others together to communicate with the patients. • Explain the circumstances of surgery and methods of cooperation. • Relieve tension of patients and establish a good relationship between the patients and nurses. • The operation site and incisions should be marked by the doctors and nurses together to improve the safety of the operation
- 138. Acute pain related to enlargement of thyroid nodule and radiation of pain to ear as evidenced by pain scale =5/10 Assess verbal and nonverbal reports of pain, noting location, intensity (0–10 scale), and duration. Place in semi-Fowler’s position and support head and neck with sandbags or small pillows. Maintain head and neck in neutral position and support during position changes. Give cool liquids or soft foods, such as ice cream Administer analgesics and/or analgesic throat sprays and lozenges as necessary. Encourage patient to use relaxation techniques
- 139. Imbalanced Nutrition less than body requirement related to difficulty in swallowing as evidenced by weight loss • Monitor daily food intake. Weigh daily and report losses. • Provide semi-liquid diet and gradually transferred to a normal diet. • Assess choking, aspiration or other symptoms. • Maintain Calm surrounding while giving meals
- 140. Post-operative management Routine postoperative nursing: • Tracheostomy kit has to be prepared at the bedside conventionally after surgery. • The patients should be placed on ECG monitoring and low-flow oxygen inhalation to observe the change of vital signs closely. • 70°semi-reclining position should be kept • Inform doctors of abnormal drainage timely. • Additionally, the drainage tube should be removed if the drainage volume was less than 5ml/24h . • The patients should be encouraged to move 24h after surgery.
- 141. Post-operative management Diet nursing: • Postoperative diet should be cool and not too hot to avoid overheating which could induce neck blood vessels to dilate and increase bleeding. • Semi-liquid diet can be given if there was no discomfort in the patients (gradually transferred to a normal diet). • Nurses needed to observe whether choking, aspiration or other symptoms occurred in the patients. • If coughing occurred, the patients can be guided to drink a small amount of water each time.
- 142. Post-operative management Trachea management: • It is of great significance to prevent respiratory obstruction and infection. • The patients should be placed in semi-recumbent position after surgery and given continuous low-flow oxygen inhalation and continuous mask oxygen inhalation if necessary, with their oxygen saturation of blood maintained around 98- 100%. • Daily aerosol inhalation should be given routinely in order to help clearing secretion in the airway. • For those patients with indwelling endotracheal tube, continuous intratracheal instillation of 0.45% saline and medicine should be given to reduce sputum production.
- 143. Nursing of postoperative complications Bleeding: • Bleeding mostly occurs within 24 hours after surgery. • Nurses should observe the symptoms including whether thickened neck, subcutaneous congestion, bleeding exudation in wound dressings, sudden increase of drainage liquid in the negative-pressure drainage tube on the wound, bright red drainage and dyspnea and other symptoms of tracheal compression occurred in patients.
- 144. Cont… • Sandbag oppression could be employed for hemostasis of mild subcutaneous hematoma, or cold compression using ice packs could be adopted to alleviate the symptoms of bleeding. • Drainage tube can be squeezed once within 30-60 minutes depending on the conditions in order to prevent clogging of the drainage tube.
- 145. Nursing of postoperative complications Dyspnea : • In most cases,dyspnea is induced by bilateral recurrent laryngeal nerve (RLN) injury, hematoma compression, laryngeal edema, tracheal collapse. • Sterile tracheotomy kit and sterile gloves should be prepared at the bedside after surgery. • Timely inspections of wards should be carried out to observe whether dyspnea, cyanosis, irritability and other kinds of discomfort with thickened neck circumference, decrease in oxygen saturation, expectoration and sputum tone occurred.
- 146. Nursing of postoperative complications Hoarseness and drinking cough: • Hoarseness and drinking cough are often induced by injury of laryngeal nerve and recurrent nerve. • After surgery, the patients should be encouraged to speak, and observed to find whether there were some symptoms including hoarseness, aphonia, dyspnea, tone lowering, drinking cough. • The patients should be guided to drink a small amount of water each time and to speak gradually when they were awake after anesthesia.
- 147. Nursing of postoperative complications Limb twitch and lip numb: • Limb twitch and lip numb are often caused by parathyroid damage. • Patient should be managed on intravenous injection of 10% calcium gluconate . • Followed by oral and intravenous treatment of calcium supplements.
- 148. Postoperative management Shivering and fever: • Belonging to symptoms of thyroid storm, shivering and fever mostly occurred within 12 h-36 h after surgery. • After surgery, the patients should be monitored for changes in vital signs. • Patients may show fever, irritability, delirium, sweating, vomiting and can exhibit coma, shock and even death if they were not promptly treated. • Patients should be immediately given treatments of oxygen, cooling, sedation, oral intake of iodine, intravenous injection of hydrocortisone.
- 149. Postoperative management Acute Pain related to surgical interruption/manipulation of tissues/muscles Assess verbal and nonverbal reports of pain, noting location, intensity (0–10 scale), and duration. Place in semi-Fowler’s position and support head and neck with sandbags or small pillows. Maintain head and neck in neutral position and support during position changes. Give cool liquids or soft foods, such as ice cream Administer analgesics and/or analgesic throat sprays and lozenges as necessary. Encourage patient to use relaxation techniques: guided imagery, soft music, progressive relaxation
- 150. Monitor respiratory rate, depth, and work of breathing Auscultate breath sounds, noting presence of rhonchi. Assess for dyspnea, stridor, “crowing,” and cyanosis. Note quality of voice. Suction mouth and trachea as indicated, noting color and characteristics of sputum Assist with repositioning, deep breathing exercises, and/or coughing as indicated Check dressing frequently, especially posterior portion. Keep tracheostomy tray at bedside. Provide steam inhalation; humidify room air.
- 151. Risk for tetany related to loss of parathyroid glands Monitor vital signs: remaining alert for elevated temperature, tachycardia, dysrhythmias, respiratory distress and cyanosis. Evaluate reflexes periodically. Observe for neuromuscular irritability (twitching, numbness, paraesthesias, positive Chvostek’s and Trousseau’s signs, seizure activity). Keep side rails raised/padded, the bed in low position, and an artificial airway at bedside. Avoid use of restraints.
- 152. Impaired Verbal Communication related to vocal cord injury /laryngeal nerve damage Assess speech periodically. Encourage voice rest Keep communication simple. Ask yes or no questions. Provide alternative methods of communication as appropriate: slate board, picture board. Anticipate needs as possible. Visit patient frequently. Maintain quiet environment.
- 153. Research Input Effect of teaching patients neck stretching exercises on neck pain and disability following thyroidectomy sahar a. Et al Journal of Nursing Education and Practice 2018, Vol. 8, No. 1 • METHODS: Randomized controlled trial • SAMPLE: 60 adult male and female patients scheduled to undergo thyroidectomy. Neck stretching exercises :relax your neck and shoulders ,look down, turn your face to the right side, turn your face to the left side, incline your head to the right side, incline your head to the left side, turn your shoulders round and round, and slowly raise your shoulders fully then lower them again. • RESULT: 56.7% patients in study group as compared to 10% in control group had no disablity and pain on the neck 7 days post thyroidectomy • CONCLUSIONS: Teaching and applying neck stretching exercises significantly improved the neck condition of patients in the study group regarding pain and disability of the neck.
- 154. Discharge teaching Encourage well-balanced, nutritious diet rich in calcium and vitamin D. and, when appropriate, inclusion of iodized salt. Teach postoperative exercises to be instituted after incision heals: flexion, extension, rotation, and lateral movement of head and neck. Encourage rest and relaxation, avoiding stressful situations and emotional outbursts. Instruct in incisional care: cleansing, dressing application Advice to apply moisturising cream after healing to minimise scarring Reinforce to take thyroxine supplements throughout the life Notify physician on developing fever, chills, continued or purulent wound drainage, erythema, nausea and vomiting, insomnia, constipation, drowsiness, intolerance to cold, fatigue. Stress necessity of continued medical follow-up.
- 155. Conclusion • Many thyroid cancers remain stable, microscopic, and indolent. Total thyroidectomy increases survival rates and decreases recurrence rates. Treatment with 131I, Molecular-targeted therapies, such as TKIs, have kept the mortality rate for thyroid cancer low, despite the recent increase in its incidence. • Designing clinical trials for new treatments is very challenging due to the rarity of parathyroid cancer. Adequate en-bloc excision of the tumour at initial surgery offer the best chance of cure and elongated disease-free survival. • Observation and nursing during perioperative period is very crucial for preventing postoperative complications.
- 156. References • Kandil E, Noureldine SI, Abbas A, Tufano RP. The impact of surgical volume on patient outcomes following thyroid surgery. Surgery 2013; 154: 1346- 1352; discussion 1352-1343. 1. https://www.thyroid.org/thyroid-cancer 2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC44151 74 3. https://emedicine.medscape.com/article/2500021- overview 4. https://emedicine.medscape.com/article/280908- overview 5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC30592 45 6. https://en.wikipedia.org/wiki/Parathyroid_carcinoma