Selected human infectious diseases part 2
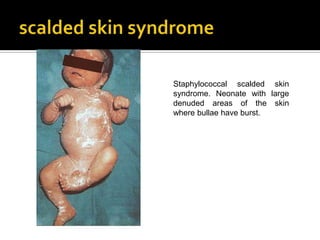
- 1. Staphylococcal scalded skin syndrome. Neonate with large denuded areas of the skin where bullae have burst.
- 2. Staphylococcal scalded skin syndrome. Large areas of epidermal loss, with some bullae still intact.
- 3. Staphylococcal scalded skin syndrome. Red raw denuded areas where skin has sloughed off.
- 4. The peeling is caused by the toxin which produces a cleavage plane high in the epidermis at the stratum granulosum level. As the areas of exfoliation dry, a flaky desquamation and then replacement with new epidermis occurs within two weeks.
- 5. SSSS is treated with a penicillinase-resistant penicillin, given intravenously, together with measures to counter hypovolaemia.
- 6. A clinically identical syndrome to SSSS, termed toxic epidermal necrolysis or Lyell's syndrome, is seen in older children or adults as a manifestation of drug allergy (particularly to sulphonamides) or viral infections.
- 7. Many advocate the use of high-dose corticosteroids for the treatment of toxic epidermal necrolysis differentiation from SSSS by means of a skin biopsy is important.
- 8. Toxic epidermal necrolysis (Lyell’s syndrome). Loss of epidermis in a black child associated with sulphonamide therapy.
- 9. This is a necrotizing infection of subcutaneous tissues usually occurring as a result of trauma or operations in the perineum, abdomen or lower extremities.
- 10. It may be caused bynclostridial species sometimes by aerobic bacteria such as streptococci, staphylococci and coliforms.
- 11. There is a gradual onset of swelling and erythema and frank crepitus in the involved area.
- 12. Postoperative gangrenous cellulitis. A huge area of ulceration filled with gangrenous skin and slough lies adjacent to the wound. There is surrounding cellulitis and a further area of necrotic skin in the flank.
- 13. The cellulitis has resolved and the ulcerated area is filled with black necrotic tissue.
- 14. There is little pain There may be a foul smelling discharge from the wound. In clostridial anaerobic cellulitis the discharge is thin and dishwater-like In non-clostridial infection it is thicker and darker in colour. Radiology may show gas in the tissues. Exploration of the wound should be performed to ensure that there is no myonecrosis.
- 15. Considerable amount of gas (G) in the tissues of the thigh of a patient with anaerobic infection following intravenous drug abuse.
- 16. Treatment consists of surgical debridement and parenteral antibiotic therapy.
- 17. Clostridial cellulitis, following a compound fracture of the tibia. Crepitus was noted on examination and the presence of gas was confirmed radiologically.
- 18. Gas gangrene (clostridial myonecrosis) is a fulminant life-threatening infection of skeletal muscle caused by Clostridium perfringens. C. perfringens produces a number of powerful toxins it is the a-toxin which is associated with the severe toxicity, haemolysis and myositis of gas gangrene.
- 19. Histology showing typical “box-car” appearance of C. perfringens in necrotic tissue. Spores are rarely seen in clinical specimens. Gram’s stain.
- 20. The incubation period is 1-4 days the earliest symptom is severe pain at the site of the wound. skin is pale and then assumes a bronze discolouration, followed by the appearance of haemorrhagic bullae. There is often a distinctive, sweetish odour to the serosanguinous discharge.
- 21. Amputation stump with discoloration of skin and hemorrhagic bullae typical of gas gangrene.
- 22. Tachycardia and apprehension are prominent there may be haemolysis and renal failure. In suspected cases it is imperative to examine the muscles for myonecrosis
- 23. A Gram stain of the exudate or the muscle will show numerous gram-positive bacteria, but this finding does not determine the need for treatment. Affected muscles initially are pale and fail to bleed or contract on electrical stimulation later they become beefy red and then gangrenous and friable.
- 24. There is a serosanguinous discharge from the lower end of the surgical wound and the affected muscles show pallor and failure to bleed.
- 25. If myonecrosis is present then immediate, extensive surgical debridement of involved muscles and fasciotomy to decompress the oedema is the only hope. Penicillin, chloramphenicol or metronidazole, gas gangrene antitoxin and hyperbaric oxygen are of help but must be regarded as of secondary importance to emergency surgery.
- 26. Animal bites Bites from domestic dogs and cats are frequent and range from the trivial to the life-threatening. Infections are caused by the animals' oral bacterial flora. The most important organism in both dog and cat bites is Pasteurella multocida, a small gram- negative coccobacillus.
- 27. Staphylococci, streptococci and anaerobic bacteria are the other common pathogens. An infected animal bite usually presents with a localized cellulitis, a malodorous wound exudate and a low-grade fever . Many bites occur close to bones or joints and septic arthritis, tendonitis and osteomyelitis sometimes occur.
- 28. Infected wound of finger following bite of domestic cat. Pasteurella multocida was isolated from the wound.
- 29. Penicillin or ampicillin is very suitable but erythromycin and the penicillinase-resistant penicillins are less effective. Amoxicillin/clavulanic acid will cover all the likely pathogens and tetracycline can be used in the penicillin-allergic individual. Tetanus and/or rabies prophylaxis should also be considered.
- 30. Human bites The normal human oral flora is capable of causing severe infections, either as a result of bites or in clenched fist injuries
- 31. The organisms responsible are a-haemolytic streptococci and various anaerobes including Fusobacterium spp. Bacteroides spp. and Eikenella corrodens. The latter is particularly important as it often produces an indolent infection and is resistant to clindamycin, metronidazole, penicillinase-resistant penicillins and some cephalosporins.
- 32. managed with primary closure require irrigation, debridement, immobilization, elevation and close observation. Penicillin plus a penicillinase-resistant penicillin or amoxicillin/clavulanic acid are the drugs of choice.
- 33. Etiologic agent: Neisseria meningitidis - Human are the only natural hosts - Nasopharynx is the portal of entry - Fulminant meningococcemia is more severe, with high fever, and hemorrhagic rash; there may be disseminated intravascular coagulation and circulatory collapse (Waterhouse-Friderichsen syndrome)
- 34. Meningococcaemia The rash of meningococcal septicaemia varies a good deal in distribution and extent, as well as in the character of the individual lesions. The lesions of acute meningococcaemia are mixed petechial and maculopapular rash most prevalent on the extremities and extensor surfaces.
- 35. *meningitis – is the most common complication of meningococcemia - Usually begins suddenly, with intense headache, vomiting, and stiff neck, and progress to coma within few hours
- 36. Acute meningococcemia. Note the variable size of the lesions and their peripheral distributions. Some of the lesions are obviously purpuric, others macular or papular.
- 37. Purpuric lesions of variable size on buttocks and thighs.
- 38. The rash starts as erythematous macules that are at first not purpuric, then becomes brown-stained appearance. Purpuric lesions vary in size between petechiae and ecchymoses of up to several centrimetres in diameter with an irregular edge. Petechiae may also be seen in the conjunctivae.
- 39. Petechiae on the ankle of a young child with meningococcemia
- 40. Large ecchymoses of variable size and with an irregular edge.
- 41. Petechia on bulbar conjunctiva.
- 42. Clinical meningitis is common and the organism is often seen in the cerebrospinal fluid deposit. Gram-negative diplococci can occasionally be seen on smears obtained from the skin lesions of acute meningococcaemia.
- 43. Ecchymoses have undergone central ulceration in the aftermath of the acute illness with subsequent skin necrosis. Skin grafting was required.
- 44. In the most severe form of meningococcal septicaemia, accompanied by hypotension disseminated intravascular coagulation peripheral gangrene purpura fulminans
- 45. Gangrene of the extremities following a near-fatal illness with hypotension.
- 46. Gangrene of both legs in a black man with acute meningococcal infection. Bilateral below-knee amputations were later required.
- 47. Chronic meningococcaemia is an infrequent syndrome of recurrent episodes of fever, arthralgia and rash occurring over a few weeks. The lesions may be maculopapular, petechial, vesicular or pustular paralysis and cardiac toxicity are rare.
- 48. Chronic meningococcemia. Maculopapular lesions over the dorsum of the foot of a young woman with recurrent arthralgia and fever. Neisseria miningitidis was isolated from blood culture.
- 49. Vesiculopustular lesions on the leg of a hemosexual man with N. meningitidis bactaeremia. The lesion is similar to that seen in gonococcal septicemia, which was the initial clinical diagnosis in this man.
- 50. Erythema nodosum This condition consists of red, raised, painful, tender, discrete yet ill-defined nodules (Fig 10.105), usually occurring on the shins (Fig 10.106), but less commonly on the upper limbs and face. The lesions are usually symmetrical. They progress over days or weeks to a more indolent purple-brown appearance before gradually subsiding.
- 51. Close-up of purple-red nodular lesions on shins.
- 52. Lesions are typically symmetrical over lower legs.
- 53. Fever, malaise and painful swelling of the ankles are common accompaniments. Erythema nodosum is a form of cutaneous vasculitis that represents a hypersensitivity reaction with numerous clinical associations.
- 54. The most frequent are sarcoidosis, primary tuberculosis, b-haemolytic streptococcal infections, leprosy, yersiniosis, coccidioidomycosis and histoplasmosis. It may also be precipitated by drugs, inflammatory bowel disease and certain collagen diseases. Rarely, the following infections have also been associated with erythema nodosum:cat- scratch disease, psittacosis, other chlamydial infections and measles.
- 55. Therapy should be directed at eliminating the underlying cause. Symptoms are treated with aspirin or anti-inflammatory therapy.
- 56. Erythema multiforme Erythema multiforme is a hypersensitivity reaction that develops in response to an infection or to drugs or other chemicals. The skin lesions appear suddenly over any body area, including the palms and soles.
- 57. As its name implies, the lesions of erythema multiforme vary greatly; maculopapular, petechial and vesicular elements may all be seen, but the characteristic element is the target lesion, in which the initial lesion spreads in an annular fashion, followed by the development of a new spot in the middle of the ring.
- 58. Typical target lesions on the palm.
- 60. Purpuric lesions over the foot. Although these lesions are not as typical as those shown above, the target-like configuration of some of these lesions can still be discerned.
- 61. Usually only the skin is affected but inflammation and sometimes ulceration of the oral, ocular and genital mucosal surfaces may also occur: it is then termed the Stevens- Johnson syndrome.
- 62. Stevens-Johnson syndrome. Lesions of erythema multiforme can be seen on the face, together with involvement of the mouth.
- 63. Stevens-Johnson syndrome. Severe illness with marked cutaneous and mucous membrane lesions of erythema multiforme.
- 64. The best established infective associations of erythema multiforme are herpes simplex and Mycoplasma pneumoniae; others include histoplasmosis, coccidioidomycosis and infections caused by coxsackie virus B5, adenoviruses, Salmonella, Yersinia and Mycobacterium species. The other well established association is drug exposure, notably to sulphonamides and phenylbutazone.
- 65. protozoal and helminth infection
- 66. Trichinosis Trichinosis is a ubiquitous disease of man and animals acquired by eating raw or undercooked meat containing encysted larvae of the roundworm, Trichinella spiralis. In most cases the meat is pork or wild boar, but recently a number of cases have been traced to bear or walrus meat and even (occasionally) horsemeat.
- 67. Following ingestion, the cyst walls are digested in the stomach and the viable larvae pass into the small intestine. They attach to the mucosal lining and develop into adult worms. Each fertilized female releases several hundred larvae over a period of about two weeks before she dies. The newborn larvae burrow into the intestinal lymphatics, then move via the thoracic duct to the general circulation, by which means they are distributed throughout the body.
- 68. In most tissues they are killed by the inflammatory response which they elicit, but in skeletal muscle (particularly in the diaphragm, chest wall, biceps and gastrocnemius) they become encysted and remain viable and infectious. After many years they die and the lesions eventually calcify.
- 69. Early stage of infection showing larva of Trichinella spiralis in skeletal muscle before encystment.
- 70. Coiled encysted larva of T. spiralis (L) in muscle of tongue.
- 71. High powered view of coiled larva of T. spiralis in fully formed cyst within striated muscle of tongue, showing hyaline capsule of the cyst. H & E stain.
- 72. Coiled encysted larva of T. spiralis (L) in striated muscle showing intense inflammatory reaction around cyst. Trichrome stain.
- 73. Most infections are asymptomatic but heavy exposure may cause diarrhoea or an illness characterized by fever, muscle pain, and periorbital oedema. Diarrhoea and abdominal pain is caused by the adult worms in the intestine and is usually seen only in the first few days after ingestion. The other symptoms are associated with the burden of larvae in the muscles.
- 74. Occasionally conjunctivitis and haemorrhages in the conjunctivae and nail beds are present. In extremely heavy infections a fatal myocarditis or encephalitis may occur. The systemic symptoms are usually maximal after 2-3 weeks and then subside slowly.
- 75. Splinter haemorrhages in the nail beds.
- 76. Cysticercosis Infection with the larvae of Taenia solium (cysticercosis) most often produces symptoms referable to the central nervous system but the larvae may also develop in skeletal muscle. After a few years the organism dies and the wall of the cyst eventually calcifies.
- 77. The condition is usually clinically silent and is generally only recognised when soft tissue x-rays are taken in asymptomatic patients with other conditions and the characteristic calcified cysts are seen.
- 78. Radiograph of leg showing characteristic elongated calcified cysts of T. solium. At this site they produce no symptoms.
- 80. Tinea versicolor Tinea (or pityriasis) versicolor is a superficial dermatomycosis caused by the lipophilic yeast, Malassezia furfur. is a normal commensal of skin and what triggers transformation into hyphal forms and infection is not clear. most common in teenagers and young adults and is more likely in hot weather. The asymptomatic lesions are irregular, hypo- or hyper-pigmented, and may be circumscribed or diffuse.
- 81. Brownish-red diffuse lesions over the trunk and arms of a young man.
- 82. Superficial, brownish-red lesions over the back of a young man.
- 83. They have a dust-like scale but are not itchy. They usually occur on the trunk or proximal aspects of the limbs, but occasionally affect other areas of the skin. stained with methylene blue (the so called `spaghetti and meatballs' appearance).
- 84. Sticky tape strip showing typical cluster of round budding cells and mycelial elements of Malassezia furfur. Methylene blue stain.
- 85. Treatment for several weeks with local application of selenium sulphide suspension or a topical azole antifungal cream is effective.
- 86. Candida organisms are small budding yeasts that cause various conditions in humans. are normal commensals of humans but are capable of causing infections whenever the normal defense mechanisms are interrupted. For the prevention of cutaneous candida infection, the most important defense mechanism is an intact integument. Any factor that causes maceration of the skin predisposes to candida invasion, as does diabetes mellitus.
- 87. The most common form of cutaneous candidiasis is spread of vaginal infection to the perineum. The vulva and labia are red and intensely pruritic and there are usually irregular patches of affected skin, often with much scaling and spread to adjacent areas.
- 88. Candidiasis of the perinium. Large areas of denuded skin with rather well-defined edges and some scaling. Satelite lesions are visible beyond the edges. This is often associated with candidiasis.
- 89. In infants, the wearing of wet nappies (diapers) causes maceration of the skin: candida infection produceas a similar appearance termed napkin (diaper) rash (Fig 11.99). The perianal skin is another site (Fig 11.100) and candidal intertrigo is often seen in moist sites where skin surfaces are adjacent, as under the breasts or in the groin.
- 90. Candida napkin rash. Inflammation affecting the napkin areas, including the scrotum with prominent satellite pustules.
- 91. Perineal candidiasis. A common distribution spreading from the perianal area along the perineum.
- 92. Candida is a common cause of paronychia. The acute phase of inflammation is followed by discolouration, ridging and thickening of the nail. Paronychia are more common in those whose hands are frequently immersed in water and, as for many of the other manifestations of cutaneous candidiasis, in diabetic patients.
- 93. Candida paroncyhia. Ridged nails with indolent inflammatory tissue lateral to the nails.
- 94. Generalized acute cutaneous candidiasis. Rounded, slightly raised erythematous patches of various size developing as a generalized eruption following a napkin (diaper) rash.
- 95. All the above mild or moderate forms of cutaneous candidiasis are treatable topically with nystatin or imidazoles such as clotrimazole or miconazole.
- 96. Chronic mucocutaneous candidiasis is a persistent infection of the mucous membranes, skin, hair and nails associated with a number of immune defects, mainly of T-cell function. Some patients also have associated endocrine disorders, especially hyperparathyroidism or Addison's disease.
- 97. The clinical illness usually begins in childhood with oral candidiasis but subsequent syndromes vary greatly from mild but chronic infections, for example, candidal paronychia and angular stomatitis, to severe disfiguring granulomatous lesions.
- 98. Chronic mucocutaneous candidiasis. Chronic angular stomatitis and onychomycosis due to candida in a 12-year old child with impaired T-cell response to candida antigens.
- 99. Chronic disfiguring candida infection of the scalp in a child.
- 100. Treatment with a variety of immunostimulants has been of limited success and the treatment of choice now appears to be long term ketoconazole or fluconazole.
- 101. Disseminated candidiasis, which tends to occur in the immunocompromised or those with candida endocarditis, can be associated with cutaneous lesions. These are typically pink to red macronodules, up to 1cm in diameter, and can be single or multiple.
- 102. Disseminated candidiasis. The typical skin lesions are pinkish- red nodules, here seen on the ankle of a patient with acute leukemia. Candida can be visualized in punch biopsies.
- 103. This chronic infection is caused by Sporothrix schenckii a widely distributed saprophytic fungus. Most cases of infection in man are the result of minor trauma and inoculation of the organism through the skin.
- 104. Histological section showing small yeast-like organism of Sporothrix schenki. Gomori-methenamine silver stain.
- 105. At the site of entry (often on the hands) a small, painless, pink or purple, verrucous, nodular or ulcerative cutaneous lesion develops anything from 1 week to several months later. In 75% of cases the chronic primary inoculation lesion is associated with multiple painless nodules distributed along the lymphatic vessels draining the primary lesion.
- 106. Lympocutaneous sporotrichosis. A large verrucous and ulcerative lesion on the dorsal surface of the fourth finger. A single satellite lesion is present on the dorsum of the hand, probably along a lymphatic vessel draining the primary lesion.
- 107. A chronic crusting primary lesion involving the nail bed of the third finger, with multiple painless nodules along the lymphatic channels draining the lesions.
- 108. Sometimes these lesions ulcerate. No constitutional symptoms develop unless secondary bacterial infection develops. The organism is readily cultured from purulent exudate or biopsy material placed on Sabouraud's medium, but is rarely seen on direct examination of the tissue. The histopathological response to sporotrichosis involves granulomas and microabscesses.
- 109. Pseudoepitheliomatous hyperplasia may be present. Lymphocutaneous and cutaneous sporotrichosis usually responds to oral therapy with potassium iodide (3-4ml every 8 hours until the skin lesions disappear), but occasional cases require systemic treatment with amphotericin B, especially when deeper tissues are involved. Preliminary reports suggest that itraconazole may also be effective. Relapse is very rare.
- 110. are a group of fungal infections of the skin caused by organisms (the dermatophytes) which invade only the superficial stratum corneum of the skin and other keratinized tissues such as hair and nails.
- 111. Tinea corporis (ringworm of the body) - is most often seen in children and is caused by various species of the genera Trichophyton, Epidermophyton and Microsporum. - Some of these species, such as T. rubrum, are exclusively human pathogens, transmitted through infected skin squames, and some, such as M. canis, are transmitted to humans from animals (in this case cats or dogs).
- 112. Spiral hyphae of Trichophyton mentagrophytes.
- 113. The lesions are often found on the trunk or legs and usually have a prominent edge with a central scaly area - tinea circinata - although granulomata involving deeper layers may also be seen.
- 114. Typical lesions of tinea circinata, with margins more inflamed than the centres.
- 115. Tinea corporis. Annular erythematous lesion due to Microsporum species showing an advancing active periphery and scaling in the central area.
- 116. Inflammatory infection due to the zoophilic fungus T. mentagrophytes in a farmer.
- 117. Tinea barbae (barber's itch) is a chronic infection of the beard area of the face and neck, with both superficial lesions and deeper lesions involving the hair follicles. Tinea pedis (athlete's foot) is a chronic fungus infection of the feet, involving particularly the toes, toe webs, and soles usually caused by T. rubrum or E. floccosum. The intertriginous areas of the toe web usually show the most severe involvement with cracking and severe maceration of the skin. The major symptom is itching.
- 118. Tinea barbae (barber’s itch). Dermatophytic infection of beard area.
- 119. Tinea pedis (athelete’s foot). Scaling erythematous pruritic patches in the characteristics location involving the toes, toe webs and sole of the foot.
- 120. Treatment involves careful drying of the feet after bathing, followed by application of various topical antifungal agents. The same two dermatophytes are the usual cause of infection in the groin (tinea cruris) and similar symptoms occur. Unlike candidal groin infection, dermatophytes tend to spare the scrotum. Dermatophytes can be diagnosed by the examination of KOH preparations of skin scrapings.
- 121. Tinea cruris. Scaling rash over the thighs. Unlike candida infection the scrotum is usually spared.
- 122. The laboratory diagnosis can be made by softening skin scrapings in 10-20% KOH and examining under the microscope for fungal hyphae.
- 123. Most cases of dermatophyte infections respond readily to topical agents, either keratolytic agents such as salicylic and benzoic acid compound (Whitfield's ointment) or antifungal agents such as the imidazoles, given for 2-4 weeks. Very occasionally, chronic dermatophyte infections can cause scarring with keloid formation.
- 124. Keloid scarring on the thigh as a result of chronic tinea corporis in a South American man.
- 125. Tinea capitis (ringworm of the scalp) is chiefly a disease of children and is also caused by Trichophyton or Microsporum species. It causes scaly erythematous scalp lesions with loss of hair. Different species may produce arthrospores within the hair shaft (endothrix infections) or on the outside of the hair shaft (ectothrix infections). There are variable degrees of inflammation present: cases acquired from cattle and due to T. verrucosum often are very inflammatory and form large pustular lesions called kerions.
- 126. Tinea capitis. Scaling of the scalp and hair loss due to infection with Microsporum canis.
- 127. Infected hair shaft showing many arthrospores of Trichophyton tonsurans.
- 128. Keroin. In some forms of tinea capitis there is severe inflammation causing a pustular lesion with an exudative crust.
- 129. Infection due to T. schoenleinii causes a condition called favus. Here the hairs are infected but not structurally damaged or shed until late into the disease. This produces a marked inflammatory crust with matted hairs over the scalp.
- 130. Favus. An inflammatory response develops around individual hairs and the scalp appears to be covered with a thick crust. This is caused by T. schoenleinii.
- 131. Diagnosis of Microsporum infection may be suspected by demonstration of green fluorescent hairs under Wood's light, but hairs infected by T. tonsurans do not exhibit fluorescence. Fungus can be detected by microscopic examination of the hair (preferably a broken stub) in KOH preparations. Scalp infections do not respond to topical therapy and are usually treated with 6-12 weeks of oral griseofulvin.
- 132. Onychomycosis (tinea unguium) is a chronic fungal infection of the nails, usually associated with infection of the adjacent skin due to T. rubrum (Fig 11.95). There is thickening of the nail which becomes white, brown or yellow.
- 133. The presence of heaped-up debris containing the organism under the nail differentiates onychomycosis due to dermatophytes from that due to chronic candida infection of the nails (Fig 11.96).
- 134. Deformity and ridging of nails due to candida infection.
- 135. Onychomycosis. Chronic infection with Trichophyton rubrum in a diabetic patient, showing brittle, discoloured, nail with separation of nail bed by fungus- containing debris.
- 136. Treatment involves the removal of as much of the infected nail as possible and long term (6-12 months) systemic therapy with griseofulvin, but the infection is extremely difficult to eradicate and more than 50% relapse.
