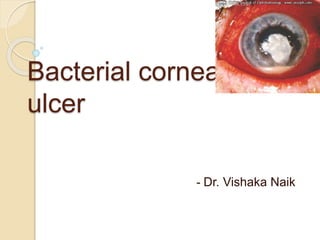
Bacterial corneal ulcer
- 1. Bacterial corneal ulcer - Dr. Vishaka Naik
- 2. Definition defined as discontinuation in normal epithelium of cornea associated with necrosis of surrounding corneal tissue.
- 3. Barriers of microbial infection • Bony orbital rim, eyelids, • Intact corneal & conjunctival epithelium Anatomical • Tear film-mucus layer • Lacrimal systemMechanical • Tear film constitutes-IgA, complement components, and enzymes lysozyme, lactoferrin, betalysins have antibacterial effect • CALT Antimicrobial
- 4. Normal defence system Normal blinking and tear flow mechanically washes out the organisms Tear film contains lysozyme, lactoferrin, betalysin which adversely affect the bacteria IgA binds to the organism and inhibits its adherance to ocular surface Components of complement pathway also help.
- 5. Normal defence system Squamous epithelium of conjunctiva and cornea provides mechanical barrier Keratocytes secrete cytokines that activate immune defences. Langerhans cells are antigen presenting cells in peripheral cornea which activate T cells when foreign antigens are processed. CALT activate T cells and produce IgA
- 6. Risk factors- External Trauma: causing breach in corneal epithelium with concurrent inoculation of organisms. Foreign bodies also can cause bacterial keratitis. Organisms that penetrate intact corneal epithelium include neisseria gonorrhea, meningitidis, c.diptheria, hemophilus aegyptius,listeria species.
- 7. Risk factors- External Contact lens wear: causes corneal hypoxia and increased corneal temperature(1), dereases pH, impaired tear exchange. it can directly traumatise epithelium when eye is rubbed with lens in place. Extended soft contact lens wearers are at 10 to 15 times increased risk than daily lens wearers(2). Aphakic contact lens wearers have 6 to 9 times increased risk due to longer wear intervals, reduced postop defence mechanism of cornea or increased hypoxia(3). 1 contact lens related k ulcers in compliant patients-Amj ohth 2004 2complications in patients with soft daily wear and soft extended wear- CLAO J 1993 3Incidence of k ulcers in aphakic contact lens wearers england- arch ophtalm 1991
- 8. Staphylococcal ulcer in a 70year old using extended wear aphakic contact lens...dense white well demarcated stromal infiltrate with overlying epithelial defect.
- 9. Risk factors- External Smoking coupled with contact lens wear increases corneal hypoxia. Further contact lens case or its solution may be also infected and infection may be occur... biofilm Pseudomonas is the most common organism in contact lens wearers, followed by staphylococcus sp and serratia marcescens. Intraepithelial infiltration of the cornea by Pseudomonas organisms in a contact lens wearer.
- 10. Risk factors- External Eyelid diseases- 1. Blepharitis, MGD 2. Dacryocystitis ( pneumococcus), canaliculitis( actinomyces) 3. Ectropion with exposure 4. Entropion with trichiasis 5. Lagophthalmos
- 11. Risk factors- ocular surface disorder Pre-existing ocular diseases: 1. decreased corneal sensation 2. dry eye due to any cause 3. SJS and ocular burns Lead to a disturbed precorneal tear film thereby increases the chance of adherance of microbes to corneal epithelium.
- 12. Risk factors- bullous keratopathy Corneal endothelial decompensation leads to surface abnormalities and epithelial defects thereby compromising the barrier function. Risk also increases due to prolonged use of local steroids and use of BCL. Ulcerative keratitis developed in 4.7% of patients with bullous keratopathy in a study by Luchs et al.
- 13. Risk factors- topical medication topical steroid , antifungal therapy, contaminated drops, traditional medicines, aesthetics Topical steroids affect the precorneal tear film and local ocular immunity by preventing neutrophilic migration in response to chemokines released by microbes. Also there is impaired opsonization of bacteria. Corneal superinfection has been reported after indiscriminate use of steroids in acute hemorrhagic conjunctivitis.
- 14. Risk factors- ocular surgery Cataract, pterygium surgeries, LASIK, keratoplasty can be complicated with occurrence of keratitis. Mycobacteruim chelonei has been reported after LASIK in sporadic and epidemic form4. 4-Infectious keratitis after LASIK;OPHTHALM2003- KARP CL, TULI SS, YOO SH, HUAN
- 15. Immunocompromised state 1. Diabetes (thickening of lamina densa leading to EDs) 2. AIDS( candida keratitis) 3. Chemotherapy patients 4. SJS, burns patients, comatosed 5. Connective tissue disorders: predispose to corneal melting and causes secondary infectious keratitis. Moraxella lacunata ulcers are associated with alcoholics and debilitated patients.
- 16. Occupational risk factors Farmers (mycotic) Animal handlers( listeria ) Gardeners Welders
- 18. Etiology AEROBES ANAEROBES 1. GRAM POSITIVE COCCI 1. GRAM POSITIVE COCCI A. Staph aureus B. Staph epidermidis C. Strep pneumoniae D. Alpha and beta hemoltyic strep E. Enterococcus A. Peptococcus B. Peptostreptococci 2. GRAM POSITIVE BACILLI 2. GRAM POSITIVE BACILLI A. Bacillus cereus B. Bacillus subtilis C. Corynebacterium D. Listeria monocytogenes A. Actinomyces B. Clostridium
- 19. Etiology AEROBES ANAEROBES 3. GRAM NEGATIVE COCCI A. Neisseria 3. GRAM NEGATIVE COCCI Veillomella 4. GRAM NEGATIVE BACILLI A. Pseudomonas aeruginosa B. Acinetobacter C. Azotebacter D. Enterobacteria- klebsiella , serratia , proteus, escherichia 4. GRAM NEGATIVE BACILLI A. Fusobacterium B. Bacteroides 5. GRAM NEGATIVE DIPLOCOCCI Moraxella Spirochaetales- treponema, leptospira 6. GRAM NEGATIVE COCCOBACILLI Haemophilus 7. Acid fast bacilli- mycobacterium, nocardia
- 20. Etiology 87% of bacterial keratitis have been attributed to staph, strep, pseudomonas and enterobacters. Specific organisms: 1. Staphylococcal organisms: susceptible corneas include prior herpetic infection, dry eye, bullous keratopathy, previous ocular surgery. 2. Streptococcus pneumoniae: cases of chronic dacryocystitis. 3. Pseudomonas species: contact lens users, use of contaminated fluorescein solution, immunocompromised state.
- 21. Etiology 4. Gram positive bacilli- bacillus cereus: keratitis following foreign body injury 5. Moraxella species: immunocompromised states 6. Corynebacterium : C. Diphtherium penetrates intact corneal epithelium. C.xerosis is associated with moraxella infection. 7. Actinomycetes :nocardia are found in soil, seen foll trauma, canaliculitis
- 22. Etiology 8. Spore forming anaerobes: Clostridia found in soil, cause keratitis rarely, may be associated with air bubbles in corneal tissue or AC. 9. Nonsporing anaerobes: foll animal bites, cause extensive tissue necrosis and gas formation. Peptostreptococcus and propionibacterium are common. 10. Non tuberculous mycobacterium: seen after surgeries like laser-in-situ keratomileusis. Mycobac leprae causes involvement of corneal nerves. 11. Listeria monocytogenes causes suppurative keratitis in animal handlers and farmers.
- 23. Parts of the ulcer Base: surface on which the ulcer rests Floor: exposed surface of the ulcer Margin: junction between the normal epithelium and ulcer Edge: is the area between margin and floor
- 24. Stages of corneal ulcer 1. Stage of infiltration: Adherence of organisms to corneal epithelium( facilitated by bacterial pili and glycocalyx envelope in pseudomonas and gonococcus) Organisms produce cytokines and chemokines which cause vasodilation They also produce proteases and disturb extra cellular matrix. Subsequently necrosis begins depending on virulence of org and host defence mechanism If lesion does not involve BM it quickly heals. If it extends beyond BM it progresses.
- 26. 2. Stage of progression: Active ulceration results from necrosis and sloughing of epithelium, BM, stroma due to lytic enzymes released. The corneal lamellae imbibe fluid and project above the surface giving saucer shaped appearance to it. Sides and floor of the ulcer show grey infiltration Vascular congestion of conjunctiva, iris and ciliary body results in hypopyon. Further progression may result in descmetocoele and perforation due to thinning of cornea.
- 28. 3. Stage of regression: Induced by natural host defence mechanism Improvement is seen in clinical signs Line of demarcation forms around the ulcer consisting of leucocytes that phagocytose the offending organism and tissue debris Margin of the ulcer becomes smooth ad floor more transperant Superficial vascularisation increases the cellular and humoral immunity Ulcer begins to heal.
- 29. 4. Stage of cicatrisation: Epithelial regeneration continues- histiocytes and keratocytes convert to fibroblasts Under the epithelium granulation tissue is formed by fibroblastic proliferation. Fibrous tissue is laid down and deposited until curvature of the cornea is achieved. When healing is complete, vessels regress and become ghost vessels. Degree of scarring results in opacities which can be nebula, macula or leucoma. Gross degree of refraction in the area of scar is due to criss cross laying down of fibrous tissue.
- 31. Clinical features Clinical signs and symptoms are variable depends on the virulence of the organism duration of infection, pre-existing corneal conditions immune status of host previous use of local steroids/anti microbials
- 32. Symptoms 1. Pain : superficial ulcers are more painful than deep due to sensory supply. Sudden relief of pain may suggest perforation. 2. Redness and photophobia are associated symptoms. Associated conjunctivitis may cause redness in gonococcal, pneumococcal and hemophilus infections.
- 33. Symptoms 3. Discharge : watery discharge is usually due to a viral ulcer, but a small bacterial ulcer may cause reflex tearing. gonococcus causes mucopurulent discharge. Pseudomonas is asso with greenish yellow discharge. Corynebacterium dipth causes membranous discharge.
- 34. Symptoms 4. Decreased visual acuity: central corneal ulcers esp pseudomonas and staphylococcus have significant loss of visual acuity. Other factors contributing: pupillary membrane, hypopyon, cataract, glaucoma, vitritis. Vision is not decreased in peripheral ulcers like coagulase negative staph.
- 35. Onset of the disease Sudden onset of decrease vision, pain, photophobia is seen in staph, pseudomonas and pneumococcus species. However bacteria like moraxella, coagulase neg staph, nocardia keratitis have gradual onset and indolent course.
- 36. General examination Facial palsy, lagophthalmos VISUAL ACUITY.
- 37. Ocular examination 1. eyelids: Trichiasis Coloboma Entropion, ectropion Proptosis Lagophthalmos Blepharitis Evert and see for foreign body
- 38. Ocular examination 2. lacrimal sac: rule out dacryocystitis. 3. conjunctiva: associated conjunctivitis with gonococcal, pneumococcal and hemophilus may be present. Presence of chemosis amd pseudomembranes to be recorded. Circumciliary flush may be seen in bacterial ulcer. Type of discharge to be noted- mucopurulent in bacterial. Greenish in pseudomonas.
- 39. Conjunctival vs ciliary congestion S. no. Feature Conjunctival congestion Ciliary congestion 1. Site More marked in the fornices More marked around the limbus 2. Colour Bright red Purple or dull red 3. Arrangement of vessels Superficial and branching Deep and radiating from limbus 4. On moving conjunctiva Congested vessels also move Congested vessels do not move 5. On mechanically squeezing out Vessels fill slowly from fornix towards limbus Vessels fill rapidly from limbus towards fornix 6. Blanching, i.e., on putting one drop of 1 in 10000 adrenaline Vessels immediately blanch Do not blanch
- 40. Ocular examination 4. Precorneal tear film: in active keratitis, tear film will have numerous cells and debris. 5. cornea: Corneal ulcer - location, shape, margin, size, epithelial defect, infiltration, sensations Surrounding cornea and vascularisation
- 41. Corneal ulcer 1. location: should be marked schematically on diagram. May be central, paracentral, peripheral or total. Central ulcers have poor vision with poor visual prognosis- usually staphylococcal. Mycobacterium cause peripheral ulcers.
- 43. Corneal ulcer 2. Shape of the ulcer: bacterial are usually punched out ulcers; round or oval in shape 3. margins: vary according to the stage. Healing ulcers have well defined slopy margins. Active ulcers have indistinct/ragged margins.
- 45. Corneal ulcer 4. Size of the ulcer: important for follow up visits and monitor progress. 5. Epithelial defect: Epithelial defect and size of infiltration should be measured separately in two largest meridians. In cases of corneal abscess, epithelium may be intact over the infiltration. Staining may be used ( fluorescein or rose bengal) whenever necessary. Epithelial edema if present should be noted.
- 47. Corneal ulcer 6. infiltration: may be single or multiple, should be measured. 7. Corneal sensations: either with a cotton wisp or esthesiometer.
- 48. Surrounding cornea May be clear or hazy Pseudomonas ulcers – surrounding cornea is edematous and appears like a ground glass. Clearing of surrounding edema may be a sign of healing.
- 50. Corneal vascularisation Superficial or deep.
- 51. Superficial corneal vascularisation Deep corneal vascularisation Vessels can be traced from limbus into conjunctiva Vessels end abruptly at the limbus Vessels are bright red and well defined Vessels have a bluish red blush They branch in arborescent manner Run parallel to each other Make the corneal surface irregular Donot disturb the corneal surface
- 52. Ocular examination 6. Anterior chamber: mild cells, flare or gross hypopyon(measurement) may be present. Mobile hypopyon is seen in bacterial keratitis i.e. Movement of hypopyon with change in head position of the patient. Hypopyon is fluid and settles at 6oclock. Horizontal upper border. Shifts on head tilt. Absorbs readily and recurs
- 53. Ocular examination 7. iris: synechiae, rubeosis iridis, in a perforated ulcer- corneoiridic plug. 8. Pupil and lens: pupil size and reaction; lens if visible for cataractous changes. 9. Scleral involvement: scleral involvement warrants the use of iv antibiotics.
- 56. Grading of corneal ulcer Harrison SM. Grading corneal ulcers. Ann Ophthalmol 1975;7:537-9, 541-2. Features Mild Moderate Severe Size <2mm 2-5mm >5mm Depth of ulcer <20% 20-50% >50% Stromal infiltrate 1.Density 2.Extent Dense Superficial Dense Upto mid- stroma Dense Deep stromal Scleral involvement present
- 57. Ocular examination 10. Posterior segment: vitreous and retina if visible for vitritis. 11. IOP: digital; in cases of descematocoele, never assess digitally.
- 58. Documentation Colour photographs- diffuse as well as slit section . Schematic diagrams: colour coding black- outline limbus, scars, foreign bodies Blue- stromal, epithelial edema, DMFolds Brown- melanin, iron, iris Red- blood vessels; dotted- ghost vessels Yellow- infiltrate, hypopyon, KPs, lipid degeneration
- 59. Special features- staphylococcus 2 types of staphylococci keratitis 1. Accompanies staphblepharitis or conjunctivitis – inflammatory response to toxins produced by organism in lids and conjunctiva, one or more, small, well circumscribed, anterior stromal infiltrates that are free of replicating bacteria. 2. Inflammatory response to staphylococci within cornea. Infiltrate is central, longer, severe.
- 61. Staphylococcal • Hallmark of staphylococci diseases is suppuration Central,oval, opaque Distinct margins. Mild oedema of remaining cornea. Stromal abscess in longstanding cases. Mild to moderate AC reaction. Affects compromised corneas e.g. Bullous keratopathy , dry eyes , atopic diseases.
- 62. Pseudomonas P. aeruginosa, P. flurescens (less frequent) P. aeruginosa is a slender, gram negative rod, synthesize a bluish green phenazine pigment (pyocyanin) therefore the colour green. Known to replicate in any moist area; grows in eye drops, irrigating solutions, cosmetics fluorescein solution. Has hemolysins, lipase and proteases
- 63. Pseudomonas Rapidly spreading. Extends periphery & deep within few days. Stromal necrosis & corneal liquifaction progressing to destruction of stromal descemetocoele and perforation Spreads concentrically and symmetrically to involve whole depth of cornea-Ring ulcer. Greenish-yellow discharge. Hypopyon is present. Untreated corneal melting.
- 64. Streptococcus Pneumonia (pneumococcus) Are encapsulated, gram positive, lancet shaped diplococci, seen as short chains Survive as long as it is extracellular. Once ingested, it is destroyed. Protection against phagocytosis is prevented by capsule. Produces several toxins of which Pneumolysin causes corneal destruction Common if coexistent chronic dacryocystitis present
- 65. Pneumococcal Ulcer serpens is greyish white or yellowish disc shaped ulcer occuring near center of cornea. starts at periphery & spreads towards centre Tendency to creep over the cornea in serpiginous fashion- Ulcus Serpen. Violent iridocyclitis is often associated with it. Hypopyon – always present It has great tendency for PERFORATION.
- 66. Streptococcus viridans Infectious crystalline keratopathytype of stromal keratitis Characteristic: infiltrate with lattice configuration in anterior stroma.
- 67. Infectious Crystalline Keratopathy The arborising profile of the infiltrate is believed to reflect, proliferation of bacterial colonies along lamellar planes of stromal collagen. relative absence of associated inflammatory response. May be associated with ED or not Infiltrates are also described near graft host junction of cornea transplant & after incisional keratotomy in cornea grafts.
- 68. Infectious crystalline keratopathy Risk factors include: a) Suture in situ b) Loose sutures c) Prolonged use of local steroids d) Use of contact lens e) Epikeratophakia f) h/o HZV/HSV g) Abuse of topical anaesthetic agents.
- 69. Infectious Crystalline Keratopathy Stromal involvement is in form of neovascularisation, scarring, ring abscess or combination. Paucity of inflammation is due to local immunosupression Histopathology: colonies of basophilic bacteria in anterior stroma (colonies are insinuated between collagen lamellae with paucity of inflammatory cells)
- 70. BACILLUS Bacillus Cereus keratitis is extremely severe and can progress rapidly to perforation, endophthalmitis. c/f: ring infiltrate is seen in stroma. H/o FB/ trauma is usually present
- 71. CORYNEBACTERIUM Can penetrate intact cornea epithelium Rare due to immunization Small ED with underlying stromal infiltrate Frequently associated with moraxella infections MORAXELLA Seen in immune compromised Ulcer is oval, seen on inferior exposed part of cornea infiltrate spreads deeply into the cornea, forming a stromal abscess The ulcers are ofter, painless, but almost invariably cause a hypopyon and ocassionally a hyphema
- 72. LISTERIA Ocular involvement is rare. Can penetrate intact corneal epithelium Clinically large KPs, elevated iop, dark hypopyon and pigment dispersion noted. Outcome poor. NOCARDIA Seen usually in the immunocompromised Preceeded by minor trauma Associated conjunctivitis may be there Non specific punctate epitheliopathy Stromal involvement is nodular or granular Satellite lesions may be present
- 73. ACTINOMYCES Anaerobe, rare cause of keratitis Chronic granulomatous infection Asso with canaliculitis May also have head face neck involvement Ulcer bed is relatively dry looking, discrete white stromal infiltrates are seen, satellite lesions may be present( mistaken for fungal)
- 74. DEPENDING UPON THE CIRCUMSTANCES, THE COURSE OF THE BACTERIAL ULCER MAY TAKE ONE OF THE 3 FORMS:- A.ULCER MAY HEAL & BECOME LOCALIZED. B.PENETRATE DEEP LEADING TO CORNEAL PERFORATION. C.SPREAD FAST IN THE WHOLE CORNEA AS A SLOUGHING CORNEAL ULCER.
- 75. complications A. Before perforation: 1.Ectatic cicatrix 2.Descematocoele 3.Opacity 4.Glaucoma 5.Uveitis 6.endophthalmitis
- 76. complications B. After perforation: 1.Prolapse iris 2.Corneal fistula 3.Adherant leucoma 4.Anterior staphyloma 5.Cataract 6.endophthalmitis
- 77. Corneal Opacity Nebular cornea opacity : details of iris are seen through the opacity. Macular cornea opacity : more dense details of iris not seen but iris and pupillary margins are visible. Leucoma : dense white opaque cornea. No new of Iris/Pupil. Old central leucomata sometimes show a horizontal pigmented line in palpebral aperture (nature is obscure may be due to deposition of iron from pre corneal tear film)
- 79. Corneal opacity thin diffuse nebula interferes more with vision than dense localized leucoma (not in pupillary area) because leucoma entirely blocks light but nebula refracts light irregularly causing blurring of image. Small central or paracentral opacity does not prevent focusing of image on macular region of retina hence is loss of brightness rather than of definition Some opacity always remains when bowmans membrane is injured but clears considerably in younger individuals.
- 80. Keratectasia/ectatic cicatrix In case of deep ulcers, loss of tissue causes thinning of entire cornea so that it bulges under the normal IOP. as the cicatrix becomes consolidated, the buldging disappears or remains permanently as ectatic cicatrix.
- 81. Descemetocoele Ulcers especially those due to pneumococci extend rapidly in depth so that the whole thickness of cornea except DM may be destroyed. DM offers great resistance to inflammatory process but is unable to support the IOP and hence herniate through the ulcer – Keratocoele this may persist surrounded by a white cicatricial ring or may rupture.
- 82. PERFORATION Causes : sudden exertion by patient like coughing/ straining/ sneezing, causing increased IOP. Rupture of descematocoele escape of aqueous IOP falls to atmosphere level Iris & lens is driven anteriorly to touch cornea Effects of perforation : IOP falls Pain decreases extension of ulcer ceases cicatrization starts rapidly
- 83. Perforation After perforation, iris is drawn into the aperture when aqueous escapes. If perforation is small, iris adheres to the opening, scar tissue is formed over adherant iris – pseudocornea (anterior synechiae) If perforation is large, there occurs prolapse of iris. Colour of iris becomes obscured soon by deposition of grey or yellow exudate on its surface but eventually iris stroma becomes thinned and black pigmentary epithelium becomes visible
- 84. Secondary Glaucoma Exudates clog the trabecular meshwork If prolapse of iris has occurred, exudates covering the prolapse becomes organized and forms thin layer of connective tissue over which the epithelium grows. Contraction of the fibrous tissue tends to flatten the prolapse
- 85. STAPHYLOMA An ectatic cicatrix in which the iris is incarcerated which may be partial or total. Bands of scar tissue vary in breadth & thickness – lobulated appearance often blackened with pigment, hence the name. Histology: iris tissue enmeshed in corneal tissue remnants (hence also called corneoiridic scar)
- 86. Anterior Capsular Cataract If perforation occurs opposite pupil pupillary margin of iris becomes adherent to the edges of cornea ulcer and aperture becomes filled with exudates. Anterior chamber is reformed very slowly, if lens remains in contact with ulcer for long time – anterior capsular cataract may be formed.
- 87. Corneal fistula As the Anterior chamber reforms, the exudate filling the opening is submitted to strain & frequently ruptures if patient is restless. If this process is repeated, opening becomes permanent forming a cornea fistula. When whole cornea sloughs with the exception of narrow rim at the margin, total prolapse of iris occurs. Pupil usually becomes blocked with exudate & a false/pseudocornea is formed consisting of iris covered with exudate.
- 88. Expulsion of lens & Vitreous If perforation takes place suddenly the suspensory ligament of lens is stretched or ruptured, causing subluxation of lens or even anterior dislocation & spontaneous expulsion of lens & vitreous through the perforation.
- 89. Hemorrhage With perforation, sudden reduction of IOP may cause rupture of blood vessels causing intraocular hemorrhage (vitreous/choroidal/choroidal/subretinal/subchoroidal) Expulsive hemorrhage may also occur.
- 90. Others Finally organisms causing the ulceration may gain access to the interior of eye following perforation causing Endophthalmitis Panophthalmitis.
- 91. Ocular Investigation Apart from slit lamp examination, ultrasonography Bscan should be done if endophthalmitis is suspected.
- 92. Systemic Investigations 1. Complete hemogram 2. FBSL; PPBSL & HbAlC in DM 3. RFTes, LFTes 4. Urine analysis 5. Rule out sources of infection Ear, nose, throat Dental focus
- 93. Microbiological Investigations Detection of bacteria, fungi, protozoa Corneal scrapings are to be collected & sent for Gram /KOH staining Culture /sensitivity Contact lens, lens case & solution should be evaluated in lens users.
- 94. Collection of samples Anaesthesia: Under topical anaesthesia Instill 2 drops of 0.5% proparacaine in the lower fornix Proparacaine is least bactericidal as compared to tetracaine & xylocaine. Sedation in children, uncooperative patient
- 95. Collection of sample instruments Kimura’s spatula 26 G needle Bard Parker Blade Hypodermic needle Platinum spatula (rapidly sterilized with a Bunsen Burner) (traditional)
- 96. Corneal scrapings - technique Lid speculum (apply gently) Scraping should ideally be done under slit lamp/operating microscope. Any debris around the ulcer should be cleaned with a sterile swab.
- 97. Corneal scrapings - technique Using kimura’s spatula/23 G needle /Bard Parker knife, the leading edges & base of the ulcer are scrapped. Streptococcus is found at the edge, Moraxella is found at the base Avoid touching eyelids/eyelashes to prevent contamination.
- 98. Corneal Scrapings More recently, Calcium Alginate Swabs moistened with trypticase Soy broth is used for collecting corneal specimens. Studies have demonstrated higher yield of bacteria & fungi when this method was used as compared to platinum spatula. Comparison of techniques for culturing corneal ulcers ophthalm 1992
- 99. Difficulties – Sample collection Insufficient material to inoculate in small ulcers In advanced cases of descematocoeles prior use of antibiotics gives false results In deep stromal keratitis, overlying epithelium is intact, in this case small trephine/microsurgical scissors may be used to obtain the sample
- 100. SMEARS Transfer material from spatula to glass slide & spread over 1cm area Mark the area with wax pencil to obviate the need to search for the area of scrapings. Minimum 2 slides – gram & KOH stain. Additional smear is prepared if indicated for other stains.
- 101. Gram staining – Method 1. Fix smear either by placing slide in methanol for 5-10 minutes & air dry OR pass the slide through flame 2-3 times, allow cooling. 2. Flood the slide with Gentian violet for 1 minute. 3. Rinse with tap water 4. Floor the slide with Gram’s iodine solution for 1 minute 5. Rinse with tap water 6. decolorize with decolorizer solution 7. Rinse with water 8. Flood the slide with counter stain – safranin for 30 seconds 9. Rinse with water 10. Allow to dry.
- 102. RESULTS Identifies 75% of the times Gram positive organisms take up violet iodine complex & stain blue-purple Gram negative bacteria lose the gentian violet iodine complex when decolorized & stain pink with safranin.
- 103. Streptococcus isolated from corneal ulcer
- 104. Pseudomonas isolates
- 105. GIEMSA Staining Romanowsky type stain which uses eosin, methylene blue & ozide dyes It stains the DNA/RNA, cell wall & septations do not take up the stain. Helps differentiate bacteria (blue) from fungi (purple), stains chlamydia inclusion bodies & cysts trophozoites of Acanthamoeba
- 106. KOH wet mount Scraped material is spread out on glass slide One drop of 10% KOH is put on scrapings & covered with cover slip & examined under microscope. KOH helps in loosening stromal lamellae & exposing fungal filaments. Stains filaments light yellow. Identifies fungi & acanthamoeba. 90% sensitive.
- 108. Ziehl Neelson Acid Fast Stain Principle: acid fastness has been ascribed to high content & variety of lipids, fatty acid & higher alcohols found in tubercle bacilli Integrity of cell wall Procedure: Make smears, air dry & heat fix them. Flood smear with carbol fuschin. Keep it for 5 mins with intermittent heating. Wash with water & pour 20% H2SO4 on the smear, keep for 2 mins. Wash again & pour loefflers methylene blue for 30 sec.
- 109. Ziehl Neelson Acid Fast Stain Wash slide & air dry smear. Examine under oil immersion, objective of 100x Appearance of Organisms: Pink rod against blue background (background varies with counter stain used) Interpretation: Smear should be considered negative after examining 100 fields taking about 10mins
- 110. CALCOFLUOR White Stain Calcofluor binds to chitin & cellulose therefore organisms like yeast & filamentous fungi stain bright green white Calcofluor under epifluorescent microscope. Cysts of Acanthamoeba also stain bright green, trophozoites of acanthamoeba stain reddish – orange.
- 111. ACRIDINE ORANGE Chemofluorescent dye – stains fungi & bacteria yellow orange against a green background Identifies gram positive and negative bacteria & yeast as well as hyphal forms of fungi & acanthamoeba.
- 112. Stain Organism Colour Gram Bacteria Gram positive – purple Gram negative – pink Acridine Bacteria fungi Acanthamoeba Yellow orange Yellow orange Calcofluor Fungi Ac. Cysts Ac. Trophozoites Bright green Bright green Reddish orange Acid Fast Mycobacteria pink
- 113. Modified Grocott Gomori Methenamine- Silver Nitrate stain reliability is more than Gram/KOH for fungal infections Specimen should be spread on gelatin coated slides. Fungus cell wall & septa stain black against faint green background.
- 114. Culture Media Media Organisms 1) Blood Agar Aerobic bacteria/fungi 2) Chocolate Agar Aerobes – facultative anaerobes Neisseria Hemophilus Moraxella 3) Thioglycolate broth Aerobic & Anaerobic bacteria 4) Sabouraud’s Dextrose Agar Plate with Antibiotic (*) Fungi Nocardia 5) Brain heart infusion Broth with Antibiotic (*) Fungi Nocardia 6) Cooked meat Broth Anaerobic Bacteria 7) Thayer Martin Blood Agar plate Neisseria 8) Lowenstein Jensen Media Mycobacterium (*)Work at room temperature, (rest work at 35 c)
- 115. Culture media initial procedure should be obtaining culture material from the conjunctiva and lid margins of both eyes the entire lower cul-de-sac should be wiped, The upper and lower tarsal conjunctivae and all of the material obtained is placed directly into culture The upper and lower lid margins also should be cultured and placed on the same plates used for the conjunctival specimens
- 116. TECNIQUE FOR CULTURE Apply topical Anaesthetic Scrape the margin of ulcer with kimura’s spatula. Transfer the isolate directly to the culture plate by making a row of C shaped marks, reversing the edge of spatula with each C, so that all the material from spatula is transferred to the plate. For inoculation into liquid media, the spatula is briefly immersed directly into the culture fluid.
- 117. Micro - ARD Micro – antimicrobial removal device. In cases which have been treated with antibiotics, microARD is used to yield positive cultures. It has sterile RESINS which bind to antibiotics. In a study by osato et al, use of micro ARD increased the isolation of organisms from 88% to 100% in ocular infections.
- 118. Duration of Isolation Usually 48 hours. All plates to be examined daily with the help of microscope & liquid media to be evaluated for presence of turbidity. Growth outside C-streak should be disregarded (implies contamination) Indigenous organisms in tear film may appear-should be distinguished on basis of sparse growth & isolation of the same organism from ipsilateral lids/conjunctiva. Aerobic cultures of corneal of specimens should be kept for 7 days; an aerobic for 7-14 days; Mycobacterial & fungal for 4-6 weeks before being reported as no growth.
- 119. AntiMicrobial Susceptibility Testing Minimal inhibitory concentration (MIC) : lowest concentration of antibiotic that will inhibit visible growth of micro organism after overnight incubation. Other tests:PCR
- 120. CONFOCAL MICROSCOPY Useful when infecting organism is large (>15m) like acanthamoeba, filamentous fungi, microsporidia, Borrelia keratitis. Is shows the cysts & trophozoites of acanthamoeba, enlarged cornea nerves. Filamentous fungi are seen as numerous high contrast lines.
- 121. CORNEAL BIOPSY In case of deep mycotic keratitis/intrastromal abscess – staining & culture comes negative. In such cases, a diagnostic superficial keratectomy or corneal biopsy is necessary. Performed under topical anesthesia under operating microscope. A microtrephine is advanced into the anterior corneal stroma to incorporate both the infected & clinically normal 1mm rim. Avoid visual axis. A crescent blade or bard parker knife is used to undermine the tissue, which may then be cut with microscissors & the tissue excised with fine tooth forceps (do not crush)
- 122. Treatment Aims of Rx: 1. Eliminate viable bacteria from the cornea. 2. Suppression of inflammatory response. Protein binding results in reversible inactivation of antibiotics ( protein bound antibiotic has No or little antibacterial activity. Albumin is present in debris of cornea ulcer, adjacent for nices & in aqueous humor of inflamed eyes. Studies insufficient.
- 123. Routes of Administration Aggressive antibiotic therapy A. Topical B. Periocular C. Systemic D. Others.
- 124. TOPICAL Most effective (produces high concentration locally and lower in systemic) No systemic toxicity Not just antibiotic but also has cleansing effect by washing bacteria, inflammatory cells, destructive enzymes & debris. Until microbiological diagnosis is established, start broad spectrum antibiotics at frequent intervals. Use either commercially available formulations or fortified. Fortified eye drops can be kept at room temperature for week without loss of activity. Initially, antibiotics are to be instilled hourly (every half an hour yields higher corneal drug levels, but compliance is erratic.
- 125. TOPICAL When confronted with a severe ulcer (particular gram negative suspect), antibiotic instillation at 1 minute intervals for 5 doses each hour for the first 6-8 hours is recommended, followed by hourly instillation. (used not more than 8 hours because potential toxicity is not known) PetitTH : Management of cornea ulcers : Symposium on ocular Therapy, volume 8, New York, John Willey & Sons 1976.
- 126. TOPICAL When clinical evidence of improvement seen, treatment is limited to working hours (hourly administration & ointment at night) With additional signs of healing, frequency is decreased to 2 hours then to 3 hours intervals & so forth. With increasing signs of healing, fortified preparation can be substituted by commercially available drops.
- 127. ANTIBIOTICS Recently, commercially available fluoroquinolones are broad spectrum (gram positive, gram negative, penicillinase producing & methicillin resistant Staph) In a study done, they have found that 0.3% ciprofloxacin eye drops given hourly causes mean corneal tissue levels exceed the minimal inhibitory concentration for most corneal pathogen. Superior penetration of cornea by ofloxacin is offset by greater potency of ciprofloxacin.
- 128. TOPICAL ANTIBIOTICS 2 multi centric studies have shown that a single topically administered fluoroquinolone is as effective as 2 fortified antibiotic preparations. Commercially available preparation have advantages : a) No frequent preparation b) Superior stability at room temperature c) Fewer potential toxic side effects.
- 129. PERIOCULAR INJECTION Either subconjunctival or subtenons produce higher corneal drug levels than topical lesser risk of systemic toxicity than systemic form. Side effects include greater patient apprehension, more pain, inadvertent intraocular administration. Comparative evaluation of periocular versus topical difficult because: a) Different quantity of drugs b) Arbitary selection of frequency c) Variable status of corneal epithelium in ulcer
- 130. PERIOCULAR ANTIBIOTICS Can be used when Confronted with a gram negative extensive cornea ulcer not responding to topical therapy. Infiltrates extending beyond limbus involving sclera. Periocular therapy is always in addition to topical & never sole source of treatment. Discontinue when signs of improvement come & continue topical. Periocular injection is very powerful in a already inflamed eye. Hence 5 topical doses of 0.5% proparacaine at 2 minutes interval is recommended before the injection OR 0.2 ml of 2% lidocaine can be given subconjunctivally in the same quadrant as antibiotic will be given. Give upto 1ml of injection, ballooning the bulbar conjunctiva adjacent to the limbus in the meridian closest to the ulcer.
- 131. SYSTEMIC ADMINISTRATION Risk of generalized toxicity higher. Concentration of drug reaching aqueous humor following systemic administration is less than that resulting from local therapy. consider it only in cases of a) Scleral involment; b) Suspected endophthalmitis.
- 132. OTHER MODES: Of historical interest continuous antibiotic lavage either via a catheter passed through upper lid or infusion contact lens device. Corneal Collagen Shield:- originally developed as a therapeutic bandage lens, in shape of contact lens from purified porcine scleral tissue or bovine corium & stored in dehydrated state. If rehydrated in a solution containing antibiotic, collagen shield absorbs variable quantity of the drug. Following application to the eye, proteases degrade the collagen & the device fragment dissolves. Dissolution time : 12-72 hours (varies with manufacturing process)
- 133. CORNEAL COLLAGEN SHIELD Studies show it is equal in efficacy to topical therapy. Best used as a supplement of enhancing cornea drug levels in irresponsive cases.
- 134. TRANSCORNEAL IONTOPHORESIS Direct current to drive an ionized drug through the cornea epithelium into the stroma & aqueous. A cylindrical eye cup containing the drug is placed on the eye & circumscribes the limbus. An electrode with the same charge as the drug contacts the drug in the eye cup, a 2nd electrode of opposite charge is connected to the ear. A milliampere direct current maintained for 1-10 minutes overcomes surface resistance of cornea epithelium & drives the drug into stroma & aqueous. Experimental.
- 135. SPECIFIC ANTIBIOTICS Ideally selection should be based on culture sensitivity If no bacteria are seen or staining, decision to be taken between 2 most common bacteria that is Staphylococcus & Pseudomonas In case of Staphylococcus, use a drug that is effective against Penicillinase producing Staphylococcus. Routine coverage of Pseudomonas is advised because of its prevalence & also because of the rapidity with which it destroys cornea. Negative gram staining in case of clinically diagnosed bacterial ulcer, we begin with gram positive cover (5% cephazolin) & gram negative cover (1.4% Tobramycin or Gentamicin)
- 136. Cefazolin :- 50mg/ ml Powder form: 500mg from 10ml artificial tears, take 5cc & solubilize the powdered contents. Transfer 5cc of this to the bottle of artificial tears making it 500mg/10ml. Excellent activity against staphylococcus & streptococcus.
- 137. BACITRACIN Can replace cefazolin if patient is sensitive to peicillins Bacterial resistance is low since it less commonly used. Causes discomfort when instilled. Concentration : 10,000 units/ml Preparation : take 15ml bottle of artificial tears, remove 9ml of artificial tears & add to each of three vials of sterile bacitracin powder (50,000 u/vial). Return the 9ml of solubilized bacitracin to artificial tear Bottle. This will give 1,50,000 units/15ml.
- 138. VANCOMYCIN Agent of choice for treatment of gram positive organisms that do not respond to cefazolin/bacitracin. Concentration 50 mg/ml Preparation: Remove 3ml from 15ml artificial tear bottle & discard. Vial of vancomycin : 500mg Solubilize 2 vials with 2cc of sterile water each: (total 4cc). Add 3ml (1 & half vial) into the artificial tear bottle to make 750 mg/15ml. Not for routine use to prevent resistance.
- 139. FLUOROQUINOLONES Commercially available (ciprofloxacin/ Ofloxacin /2nd gen), Levofloxacin – 3rd gen, Gatifloxacin/moxifloxacin – 4th gen Clinical studies have proven efficacy equal to that of use of 2 drugs.
- 140. Organism Recommended Alternative No organism Cetazolins + Tobramycin OR fluoroquinolone Bacitracin + Gentamicin Gram Positive Cocci Cefazolin Bacitracin Vancomycin Gram Negative Cocci Cefazolin Fluoroquinolone Fortified Ceftriaxone (+systemic therapy) Gram negative diplobacilli Cefazolin or fluoroquinolone Fortified Ceftriaxone Gram negative bacilli Tobramycin or fluoroquinolone Gentamicin
- 141. SPECIFIC ANTIBIOTIC After culture sensitivity report comes in 48 hours therapy can be modified. If lab report indicates that the treatment in progress will not be effective, yet the ulcer is responding well, disregard the report & observe. As a conservative guideline antibiotics can be discontinued safely 7-10 days after the corneal infiltrate has cleaned & epithelial continuity has been restored. In cases of Pseudomonas, small numbers of viable bacteria may persist in the cornea, & recommence has been described despite effective antibiotic therapy for appropriate length of time therefore continue them for 3- 4 weeks or even after the infiltrate tears.
- 143. CORTICOSTERIOIDS Termination of bacteria does not result in cessation of inflammation. PMNL cause stromal destruction. Topical steroids have to be considered when inflammation involves central or paracentral cornea. Risk: steroids impair phagocytosis & inhibit killing of bacteria therefore balance to be struck between desirable & undesirable effects of steroids.
- 144. STEROIDS Study: effect if topical steroids on antibiotic treated bacterial ulcer : Arch ophthalm 98: 1980 proved that addition of topical steroids to an EFFECTIVE BACTERICIDAL drug does not enhance bacterial replication if steroid is not instilled more frequently than antibiotic. In practice however, bacterial keratitis is treated solely with antibiotics. Only when positive Therapeutic response is seen, steroids can be added. Commonly used : 1% Prednisolone acetate suspension with lesser frequency than antibiotics & tapered.
- 145. CYCLOPLEGICS Long acting Parasympatholytic Mydriatic Cycloplegic Atropine 1% Homatropine 1% Dose: TDS or QID Action – defers formation of posterior synechiae and reduces discomfort caused by Ciliary muscle spasm. IOP to be treated with antiGlaucoma (0.5% Timolol or Acetazolamide) NSAIDS are best avoided as they may cause increased chances of corneal melting ARTIFICIAL TEARS
- 146. CONTACT LENS When stromal necrosis results in substantial tissue loss with thinning the diseased cornea is subjected to trauma by li margins from blinking & to desiccation due to abnormal tear distribution due to irregular surface. Both factors can increase inflammation & lead to perforation. Soft contact lens over the cornea can interrupt this cycle. It also facilitates reepitheliazation & promotes fibroblastic proliferation. But is may act as a physical barrier to the topical drugs, hence dose of antibiotics should be increased.
- 147. CONTACT LENS In most severe cases, when entire thickness of cornea stroma has become Necrotic & slough & only DM is intact, hydrophilic contact lens is useful. Provides structural reinforcement of DM. No well documented evidence for use of collagenase inhibitors in treatment of bacterial keratitis.
- 148. OTHERS trimming to be done in all cases. If chromic dacryocystitis is present, DCT needs to be done. If chronic marginal Blepharitis treat MG dysfunction.
- 149. Monitoring Slit lamp examination to be held every 12 hours during early phase. once clinical response is established, once a day. Signs of healing a) Decrease/clearing of hypopyon b) Decrease conjunctival discharge/debris c) Decrease in AC reaction d) Sloping edges/healing of ED e) Increased response of pupil to mydriatic f) Vascularisation occurs. Resolution of corneal edema/infiltrates takes time. Never patch an eye with cornea ulcer: closure of lids increases temperature is cul-de-sac & discharge accumulates helping bacterial replication.
- 150. Surgical Management Removal of necrotic material may be hastened by repeated scraping of the ulcer floor with spatula. Cauterization: pure carbolic acid (100%) or trichloracetic acid (10-20%) Carbolic acid penetrates little deeper when applied thus acting more widely (caustic & antiseptic) Contraindicated in ulcers with extensive thinning or perforated ulcers. Acid must not touch the conjunctiva lest adhesions form between lids & globe. Povidone – Iodine 5% can be alternative.
- 151. Surgical Management Intravitreal injection of antibiotics vitreous tap if endophthalmitis is proven or Bscan Treatment of Perforated Ulcer: A. In case of small perforation over the iris, adherant leucoma is formed & anterior chamber reforms no special treatment required. B. If perforation fails to heal & AC remains flat with hypotony: a) Less than 2mm in size, use of tissue adhesive like N-butyl 2- ethyl cyanoacrylate monomer or fibrin glue is used to seal it.
- 152. Cyanoacrylate glue Applied to the area of perforation after careful debridement. The surface is dried with a sponge & a small drop of tissue adhesive from the undersurface of a bent iris repositer or a hypodermic needle is placed immediately over the perforation. Drying takes 5- 10 minutes after which anterior chamber reforms. Following this, continuous wear soft contact lens may be applied. Advantage: good tensile strength Drawback: it may form a solid, impermeable mass in situ and may require removal.
- 153. Fibrin glue Blood derived product that is absorbable, easy to use and can be kept at room temperature or refrigerator. Can be prepared at a blood bank, or from patients own blood or commercially available preparation. Advantage: forms a smooth seal along the perforation, less postop discomfort.
- 154. Technique of Glue Application Part preparation (paint and drapes), application of topical anesthetics and speculum Debridement of necrotic tissue from ulcer crater As tissue adhesive glue adheres best to basement membrane, 1-2 mm of normal epithelium should be debride to allow the glue to properly adhere Dry the site by methyl cellulose spear As application in small amount to seal the perforation Tissue adhesive solidify in few minutes via polymerization Send this material for culture and sensitivity A large heaped up mound is not required
- 155. Check the evidence Check for anterior chamber Apply bandage of leakage by Seidel’s test maintenance (Air bubble contact lens can also be used) Tissue adhesive remains in place for weeks to months until the perforation seals, it can be removed or dislodges of its own
- 156. Tissue adhesives- complications Iridolenticular adhesion Cataract formation Rise in iop Giant papillary conjunctivitis
- 157. Surgical Management a) If perforation is larger than 2mm (up to 4mm) corneal patch graft can be applied. b) If perforation is peripheral, tenoplasty may be done. c) >4mm perforation, tectonic keratoplasty is required.
- 158. Therapeutic keratoplasty Indications: 1. Conditions refractory to maximal medical therapy 2. Carry a chance of scleral extension 3. Impending or already perforated ulcer Goals: 1. Primary is to completely remove the infective innoculum 2. Secondary is visual outcome
- 159. Therapeutic keratoplasty Types 1. Lamellar thickness 2. Full thickness Ideally fresh donor tissue is used, if not available glycerine preserved corneal tissue may be also used. Gamma irradiated sterile corneas have longer shelf life with low risk of infections. Sometimes partial thickness scleral flaps may be dissected with base at limbus, reflected onto cornea and sutured for small peripheral perforations, but these are cosmetically less acceptable.
- 160. Lamellar keratoplasty Advantages: 1. Because endothelium is not transplanted visually devastating immune rejections are rare 2. Quality of donor endothelium is not a issue( deemed unsuitable for pk) Contraindications: deep stromal keratitis; impending perforations
- 161. Amniotic membrane patch graft Amniotic membrane is folded in multiple layers to fill the defect and then all layers are sutured to the edges of corneal defect with 10-0 monofilament suture. It acts as a scaffold for epithelium to grow and gets incorporated into the stroma. Disadv: scar is dense and causes cosmetic blemish.
- 162. Collagen cross-linking Photoactivated corneal collagen cross linking is developed recently to increase the biomechanical strength of cornea. In vitro studies have shown its beneficial effect against few bacteria but not successful against fungi, acanthamoeba. Mechanism of action: 1. Interferes with enzymatic digestion caused by PMNL 2. Antimicrobial effect –destroys microbial cell wall through free radical production
- 163. Collagen cross-linking Cornea contains riboflavin but in a concentration insufficient to have antimicrobial effect. In Cxl, epithelium debridement is done, cornea is soaked in riboflavin solution and then exposed to UV-A irradiation. By products of riboflavin ( oxygen and hydroxyl radicals) damage the nucleic acids of bacteria. It has been a valuable treatment option where there is resistance to antimicrobials; helps in delaying keratoplasty.
- 164. MANAGEMENT OF CORNEAL SCAR Attempted when cicatrization is complete & irritative signs have passed. Dense corneal scars in eyes with visual potential are treated with corneal grafts Lamellar keratoplasty may be advised for superficial scars. When scar is full of thickness, penetrating full thicknning keratoplasty is used. In eyes with cornea with no visual potential, cosmetic contact lens to hide the blemish. Tattooing scars in otherwise blind eyes with Indian Ink or impregnation with inks after stromal puncture are other methods.
- 165. Flow Chart 2 Treatment Modalities MEDICAL SURGICAL 1. Topical broad spectrum preservative free eye drops. 2. Cycloplegics 3. Frequent lubrication with preservative – free eye drops. 4. Oral and systemic antimicrobial agents as per requirement. 5. Topical/systemic Steroids in cases of PUK 1. Perforation less than 2mm: bandage contact lens (BCL) 2. Size 2-3 mm: Application of tissues adhesive with BCL 3. Size > 3 mm: Corneal patch graft / multi-layered amniotic membrane graft 4. Therapeutic penetrating keratoplasty 5. Tarsorrhaphy: if lagophthalmos present. 6. Punctal occlusion: if dry eyes is associated.
Editor's Notes
- CALT- conjunctiva associated lymphoid tissue.