Jems201209 dl
- 1. september 2012 Always En Route At
- 2. Choose 11 at www.jems.com/rs
- 4. Choose 13 at www.jems.com/rs
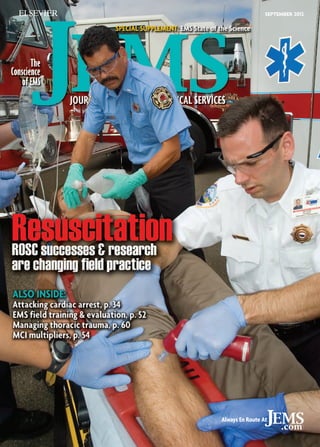
- 5. The Conscience of EMS JOURNAL OF EMERGENCY MEDICAL SERVICES 34 I Attacking Cardiac Arrest pART ii I Feedback-driven team performance impacts survival By Jeffrey M. Goodloe, MD, NREMT-P, FACEP; T.J. Reginald, NREMT-P; David S. Howerton, NREMT-P; Jim O. Winham, RN, BSN, NREMT-P; Tammy Appleby, NREMT-B SEPTEMBER 2012 Vol. 37 No. 9 Contents I 40 40 I Check the Rhythm I Expert safe use of adenosine depends on patient’s cardiac status Corey Slovis, MD, FACEP; Jared McKinney, MD; Jeremy Brywczynski, By MD, FAAEM 46 I gOING oUT ON A lIMB I EMS provider becomes patient By Steve Berry 52 I From the School to the Rig I Enhance EMS preparation using the field training evaluation program model By Skip Kirkwood, MS, JD, NREMT-P, EFO, CEMSO 54 I MCI Magnifiers I Many factors can complicate an incident of any size By A.J. Heightman, MPA, EMT-P 58 I Survive Thrive I Current goals obstacles in cardiac arrest By Brandon Oto Departments columns 7 I Load go I Now on JEMS.com 12 I EMS in Action I Scene of the Month 16 I From the Editor I It’s all about the Pump 60 I Deadly Dozen I Dealing with the 12 types of thoracic injuries By Mark Cipolle, MD, PhD; Michael Rhodes, MD; Glen Tinkoff, MD y A.J. Heightman, MPA, EMT-P B 18 I Letters I In Your Words 22 I Priority Traffic I News You Can Use 26 I lEADERSHIP sECTOR I First Day y Gary Ludwig, MS, EMT-P B 28 I Tricks OF the TRADE I Stealth Mode y Thom Dick B 30 I case of the month I Life Limb y Travis Polk, MD, Carrie Sims, MD B 32 I RESEARCH REVIEW I What Current Studies Mean to EMS y David Page, MS, NREMT-P B 68 71 72 74 I employment Classified Ads I Ad Index I Hands On I Product Reviews from Street Crews I LAST WORD I The Ups Downs of EMS I 30 About theFire Department and American Medical Response work in a systematic, coordiCover Crews from Portland (Ore.) nated manner at all resuscitations. The “pit crew” approach is proving to be a significant factor in improved resuscitation and return of spontaneous circulation results. For more, read “Attacking Cardiac Arrest, Part II,” pp. 34–39. Photo Kent Powlowski Premier Media Partner of the IAFC, the IAFC EMS Section Fire-Rescue Med 005_TOC.indd 5 I 46 www.jems.com SEPTEMBER 2012 JEMS 5 8/28/2012 9:17:07 AM
- 6. Choose 14 at www.jems.com/rs
- 7. LOAD GO log in for EXCLUSIVE CONTENT A Better Way to Learn JEMSCE.com online continuing education program n us o follow This summer, EMS providers across the nation have responded to several mass casualty incidents ranging from the July 20 Aurora, Colo., theater shooting that killed 12 and injured more than 60 to the Aug. 13 College Station, Texas school shooting that killed three near the Texas AM University campus. Our hearts go out to the victims. But equally important is the safety of the providers who respond to these types of potentially unsafe scenes. Check out JEMS.com’s major incidents page for resources on how to be prepared to respond to mass casualty incidents, such as active-shooter calls. s jems.com/major-incidents Photo BanksPhotos/iSToCkPhoTo.Com Show Of Support JEMS.com offers you original content, jobs, products and resources. But we’re much more than that; we keep you in touch with your colleagues through our: Facebook fan page; JEMS Connect site; Twitter account; LinkedIn profile; Product Connect site; and Fire EMS Blogs site. Free online Learning Opportunities! We believe learning is a lifelong commitment. We also think there’s a lot of knowledge to be had in EMS, and we bet most EMS professionals would agree. That’s why we’ve increased the number of free webcasts we’re offering. Make sure to register for one or all of them today. s jems.com/webcasts Sponsored Product Focus FLO2MAX 4-in-1 oxygen mask The FLO2MAX 4-in-1 oxygen mask from BLS Systems Limited was designed to deliver the maximal amount of oxygen to the patient. This mask was designed to eliminate room air dilution using a patented series of valves. Able to convert to a small-volume nebulizer mask, this mask can function as a true “all in one mask” for EMS services. An integrated filter captures all exhaled bacteria and excess medication, protecting equipment surfaces and staff from airborne contamination. s Check out their Hot Product listing on JEMS.com! like us facebook.com /jemsfans follow us twitter.com /jemsconnect get connected linkedin.com/groups? about=gid=113182 Hot DiscussionS polling our Fans Check out which MCIs our Facebook fans felt the most prepared for. Natural disaster 15 Major vehicle collision 73 Terrorist attack 3 Mass shooting 4 Unknown illness affecting many 3 Other 3 TOTAL votes 101 s www.facebook.com/questions/10150986687569794/ What Makes a Good Instructor? National Association of EMS Educators (NAEMSE) session speaker Keith Widmeier, NREMT-P, CCEMT-P, BA, identifies four things that make a good educator. Do you agree? s connect.jems.com/forum/topics/what-makes-agood-instructor Is Gun Violence a Social Disease? Public health experts, in the wake of recent mass shootings, are calling for a fresh look at gun violence as a social disease. What do you think? s www.jems.com/article/news/doctors-consider-gunviolence-social-dis ems news alerts jems.com/enews Check it out jems.com/ems-products best bloggers FireEMSBlogs.com www.jems.com SEPTEMBER 2012 JEMS 7
- 8. Conscience of EMS JOURNAL OF EMERGENCY MEDICAL SERVICES The Conscience of EMS JOURNAL OF EMERGENCY MEDICAL SERVICES Editor-In-Chief I A.J. Heightman, MPA, EMT-P I a.j.heightman@elsevier.com MANAGING Editor I Jennifer Berry I je.berry@elsevier.com associate eDITOR I Lauren Hardcastle I l.hardcastle@elsevier.com assistant eDITOR I Allison Moen I a.moen@elsevier.com assistant eDITOR I Kindra Sclar I k.sclar@elsevier.com online news/blog manager I Bill Carey I bill@goforwardmedia.com Medical Editor I Edward T. Dickinson, MD, NREMT-P, FACEP Technical Editors Travis Kusman, MPH, NREMT-P; Fred W. Wurster III, NREMT-P, AAS Contributing Editor I Bryan Bledsoe, DO, FACEP, FAAEM Editorial Department I 800/266-5367 I editor.jems@elsevier.com art director I Liliana Estep I alildesign@me.com Contributing illustrators Steve Berry, NREMT-P; Paul Combs, NREMT-B Contributing Photographers Vu Banh, Glen Ellman, Craig Jackson, Kevin Link, Courtney McCain, Tom Page, Rick Roach, Steve Silverman, Michael Strauss, Chris Swabb Director of eProducts/Production I Tim Francis I t.francis@elsevier.com Production Coordinator I Matt Leatherman I m.leatherman@elsevier.com advertising director I Judi Leidiger I 619/795-9040 I j.leidiger@jems.com Western Account Representative I Cindi Richardson I 661-297-4027 I c.richardson@jems.com senior Sales coordinator I Elizabeth Zook I e.zook@elsevier.com Sales Administrative Coordinator I Liz Coyle I l.coyle@elsevier.com SENIOR eMedia campaign manager I Lisa Bell I l.bell@elsevier.com advertising department I 800/266-5367 I Fax 619/699-6722 marketing director I Debbie Murray I d.l.murray@elsevier.com Marketing manager I Melanie Dowd I m.dowd@elsevier.com Marketing Conference Program Coordinator I Vanessa Horne I v.horne@elsevier.com Director, Audience Development Sales Support I Mike Shear I m.shear@elsevier.com Audience development coordinator I Marisa Collier I m.collier@elsevier.com SUBSCRIPTION DEPARTMENT I 888/456-5367 REprints, eprints Licensing I Wright’s Media I 877/652-5295 I reprints@jems.com eMedia Strategy I 410/872-9303 I Managing Director I Dave J. Iannone I dave@goforwardmedia.com Director of eMedia Sales I Paul Andrews I paul@goforwardmedia.com Director of eMedia Content I Chris Hebert I chris@goforwardmedia.com elsevier public safety vice president/publisher I Jeff Berend I j.berend@elsevier.com founding editor I Keith Griffiths founding publisher James O. Page (1936–2004) Choose 16 at www.jems.com/rs 15
- 9. Choose 16 at www.jems.com/rs
- 10. JOURNAL OF EMERGENCY MEDICAL SERVICES The Conscience of EMS JOURNAL OF EMERGENCY MEDICAL SERVICES EDITORIAL board William K. Atkinson II, PHD, MPH, MPA, EMT-P President Chief Executive Officer WakeMed Health Hospitals James J. Augustine, MD, FACEP Medical Director, Washington Township (Ohio) Fire Department Associate Medical Director, North Naples (Fla.) Fire Department Director of Clinical Operations, EMP Management Clinical Associate Professor, Department of Emergency Medicine, Wright State University steve berry, NRemt-p Paramedic EMS Cartoonist, Woodland Park, Colo. Bryan E. Bledsoe, DO, FACEP, FAAEM Professor of Emergency Medicine, Director, EMS Fellowship University of Nevada School of Medicine Medical Director, MedicWest Ambulance Criss Brainard, EMT-P Deputy Chief of Operations, San Diego Fire-Rescue Chad Brocato, DHS, REMT-P Assistant Chief of Operations, Deerfield Beach Fire-Rescue Adjunct Professor of Anatomy Physiology, Kaplan University J. Robert (Rob) Brown Jr., EFO Fire Chief, Stafford County, Va., Fire and Rescue Department Executive Board, EMS Section, International Association of Fire Chiefs Jeffrey M. Goodloe, MD, FACEP, NREMT-P Professor EMS Section Chief Emergency Medicine, University of Oklahoma School of Community Medicine Medical Director, EMS System for Metropolitan Oklahoma City Tulsa David E. Persse, MD, FACEP Physician Director, City of Houston Emergency Medical Services Public Health Authority, City of Houston Department. of Health Human Services Associate Professor, Emergency Medicine, University of Texas Health Science Center—Houston Keith Griffiths President, RedFlash Group Founding Editor, JEMS John J. Peruggia Jr., BSHuS, EFO, EMT-P Assistant Chief, Logistics, FDNY Operations Dave Keseg, MD, FACEP Medical Director, Columbus Fire Department Clinical Instructor, Ohio State University W. Ann Maggiore, JD, NREMT-P Associate Attorney, Butt, Thornton Baehr PC Clinical Instructor, University of New Mexico, School of Medicine Connie J. Mattera, MS, RN, EMT-P EMS Administrative Director EMS System Coordinator, Northwest (Ill.) Community Hospital Robin B. Mcfee, DO, MPH, FACPM, FAACT Medical Director, Threat Science Toxicologist Professional Education Coordinator, Long Island Regional Poison Information Center carol a. cunningham, md, FACEP, FAAEM State Medical Director Ohio Department of Public Safety, Division of EMS Mark Meredith, MD Assistant Professor, Emergency Medicine and Pediatrics, Vanderbilt Medical Center Assistant EMS Medical Director for Pediatric Care, Nashville Fire Department Thom Dick, EMT-P Quality Care Coordinator Platte Valley Ambulance Geoffrey T. Miller, EMT-P Director of Simulation Eastern Virginia Medical School, Office of Professional Development Charlie Eisele, BS, NREMT-P Flight Paramedic, State Trooper, EMS Instructor Brent Myers, MD, MPH, FACEP Medical Director, Wake County EMS System Emergency Physician, Wake Emergency Physicians PA Medical Director, WakeMed Health Hospitals Emergency Services Institute Bruce Evans, MPA, EMT-P Deputy Chief, Upper Pine River Bayfield Fire Protection, Colorado District Jay Fitch, PhD President Founding Partner, Fitch Associates Ray Fowler, MD, FACEP Associate Professor, University of Texas Southwestern SOM Chief of EMS, University of Texas Southwestern Medical Center Chief of Medical Operations, Dallas Metropolitan Area BioTel (EMS) System Adam D. Fox, DPM, DO Assistant Professor of Surgery, Division of Trauma Surgery Critical Care, University of Medicine Dentistry of New Jersey Former Advanced EMT-3 (AEMT-3) Gregory R. Frailey, DO, FACOEP, EMT-P Medical Director, Prehospital Services, Susquehanna Health Tactical Physician, Williamsport Bureau of Police Special Response Team 10 JEMS SEPTEMBER 2012 Mary M. Newman President, Sudden Cardiac Arrest Foundation Joseph P. Ornato, MD, FACP, FACC, FACEP Professor Chairman, Department of Emergency Medicine, Virginia Commonwealth University Medical Center Operational Medical Director, Richmond Ambulance Authority Jerry Overton, MPA Chair, International Academies of Emergency Dispatch David Page, MS, NREMT-P Paramedic Instructor, Inver Hills (Minn.) Community College Paramedic, Allina Medical Transportation Member of the Board of Advisors, Prehospital Care Research Forum Paul E. Pepe, MD, MPH, MACP, FACEP, FCCM Professor, Surgery, University of Texas Southwestern Medical Center Head, Emergency Services, Parkland Health Hospital System Head, EMS Medical Direction Team, Dallas Area Biotel (EMS) System Edward M. Racht, MD Chief Medical Officer, American Medical Response Jeffrey P. Salomone, MD, FACS, NREMT-P Associate Professor of Surgery, Emory University School of Medicine Deputy Chief of Surgery, Grady Memorial Hospital Assistant Medical Director, Grady EMS Kathleen S. Schrank, MD Professor of Medicine and Chief, Division of Emergency Medicine, University of Miami School of Medicine Medical Director, City of Miami Fire Rescue Medical Director, Village of Key Biscayne Fire Rescue John Sinclair, EMT-P International Director, IAFC EMS Section Fire Chief Emergency Manager, Kittitas Valley Fire Rescue Corey M. Slovis, MD, FACP, FACEP, FAAEM Professor Chair, Emergency Medicine, Vanderbilt University Medical Center Professor, Medicine, Vanderbilt University Medical Center Medical Director, Metro Nashville Fire Department Medical Director, Nashville International Airport Walt A. Stoy, PhD, EMT-P, CCEMTP Professor Director, Emergency Medicine, University of Pittsburgh Director, Office of Education, Center for Emergency Medicine Richard Vance, EMT-P Captain, Carlsbad Fire Department Jonathan D. Washko, BS-EMSA, NREMT-P, AEMD Assistant Vice President, North Shore-LIJ Center for EMS Co-Chairman, Professional Standards Committee, American Ambulance Association Ad-Hoc Finance Committee Member, NEMSAC keith wesley, MD, facep Medical Director, HealthEast Medical Transportation Katherine H. West, BSN, MED, CIC Infection Control Consultant, Infection Control/Emerging Concepts Inc. Stephen R. Wirth, Esq. Attorney, Page, Wolfberg Wirth LLC. Legal Commissioner Chair, Panel of Commissioners, Commission on Accreditation of Ambulance Services (CAAS) Douglas M. Wolfberg, Esq. Attorney, Page, Wolfberg Wirth LLC Wayne M. Zygowicz, BA, EFO, EMT-P EMS Division Chief, Littleton Fire Rescue
- 11. Choose 17 at www.jems.com/rs
- 12. EMS IN ACTION Scene of the month 12 JEMS SEPTEMBER 2012 Photo Rick McClure
- 13. Precarious Pileup E MS providers from Los Angeles County Fire Department, American Medical Response, Bowers Ambulance Service and MedResponse Ambulance Inc. work together alongside personnel from the Los Angeles County Sheriff’s Department and California Highway Patrol to triage 17 people involved in a major vehicle pileup on the Antelope Valley (14) Freeway. The freeway traverses a mountainous, remote area in northeastern Los Angeles County. The crash happened on June 26 near the town of Agua Dulce. For more details on how providers managed, treated and transported patients in this complex mass casualty event, see “MCI Magnifiers: Many factors can complicate an incident of any size,” pp. 54–57, by A.J. Heightman, MPA, EMT-P. www.jems.com SEPTEMBER 2012 JEMS 13
- 15. Choose 18 at www.jems.com/rs
- 16. from the editor putting issUes into perspective by A.J. HEIGHTMAN, MPA, EMT-P It’s All about the Pump Maintaining the basics is key to effective cardiac resuscitation 16 JEMS SEPTEMBER 2012 Photo A.J. Heightman A t a conference I participated in recently, Jason McMullan, MD, associate medical director for the Cincinnati Fire Department, made a statement during a lecture that I want to pass along because it illustrates the critical importance of consistent, uninterrupted compressions and care delivery to cardiac arrest patients. He pointed out that if his heart were interrupted in its pumping functions for even a few precious seconds, he would experience an interruption in oxygenated blood flow and pass out. He also noted that the longer the heart was allowed to be dormant, the longer the risk was for bad things to occur and the more difficult it would become to return the heart to its essential pumping efficiency and sustain life. So resuscitation is really all about the pump: timing, efficiency and consistency. I think back to my early days as a paramedic and the infrequent cardiac arrest “saves” I had. In almost all my successful resuscitations, someone was performing effective CPR early, a shockable rhythm was present, and I was able to rapidly draw the paddles from my defibrillator and shock the rhythm while it was primed, well oxygenated and “ripe.” In the wild, wild West days, if a gunfighter delayed in getting his gun into action, his chances of winning the battle were less than 50%. The same is true in cardiac arrest resuscitation. You can chuckle about me using those old-fashioned paddles to shock v fib, but I bet I can still get my paddles on a patient’s chest faster than you can dig out, unpackage and deploy your pre-packaged defibrillator pads. The point: Technology can sometimes present delays in care delivery if not performed rapidly and in a consistent, systematic manner. The September issue of JEMS focuses on cardiac issues, from our regular content to the special 32-page EMS State of the Science editorial supplement developed and presented to you and attendees at the bi-annual Emer- As with any task, a continuous supply of a fluid and the initial priming of the pump is key to success. gency Cardiac Care Update (ECCU) Conference in Orlando, Fla.—where the latest information on cardiac care and resuscitation will be discussed. In the supplement, developed in cooperation with the U.S. Metropolitan Municipalities EMS Medical Directors Consortium and multiple sponsors, we feature a host of key articles, backed up by 150 pieces of research, that demonstrate why delivery of resuscitation processes in the field needs to be quickly administered and, most importantly, consistently delivered. In addition to the supplement articles, each of the JEMS articles in this issue presents significant messages that are important for you to read, digest and discuss with your medical director, management team, supervisors, training staff and field crews. Each also emphasizes important processes or procedures that can increase your efficiency and effectiveness in the field, particularly in the resuscitation of cardiac arrest patients and improvements in return of spontaneous circulation (ROSC). In “Attacking Cardiac Arrest,” pp. 34–39, we focus on a systematic approach to resuscitation in the Tulsa and Oklahoma EMS systems. In “Check the Rhythm,” pp. 40–45, we discuss the correct and effective use of adenosine, the drug of choice for paroxysmal supraventricular tachycardia (PSVT) and for differentiating PSVT with aberrancy from v tach in patients with monomorphic wide complex tachycardias. Like many other potent medications designed for a specific effect on the heart, adenosine, if used inappropriately or for the wrong arrhythmia, can prove fatal. A thought-provoking question-andanswer session by EMS blogger and writer Brandon Oto, “Survive and Thrive,” pp. 58–59, rounds out the issue by presenting multiple important procedures that we currently deploy in the field, or may deploy in the future. You’ll read several common elements of cardiac resuscitation in both September JEMS and the editorial supplement. But the real take-home message is that the keys to resuscitation are early initiation of each procedure, limited interruption of compressions and a pre-planned, systematic approach to everything you do on these critical cardiac resuscitation calls. And remember, success is all about the effective use of the pump. JEMS
- 17. Choose 19 at www.jems.com/rs
- 18. LETTERS in your words I work in a dynamic system. Our response times would be faster, no doubt about it, but only if you have the correct number of units available to respond. Without a high level of responders, response times that should take less than six minutes end up taking 20 minutes. Also consider the half-life of your employees. Sitting for 12 hours a day, four days a week in a cramped ambulance isn’t healthy. I’ve seen EMS providers as young as 25 taking blood thinners. Obesity is becoming a real issue, as well as the ability to pack healthy and efficient meals for lunch and dinner, which doesn’t help the dynamic systems cause. In my opinion, dynamic systems increase response times by one or two minutes at most. And that system only works if the provider is staffed correctly. On the other hand, stations increase the time an employee can serve his or her community. The question is: Which is more important? Nathan Brooks Via jems.com I believe that the trend is to cross-train and diversify. I’m a strong supporter of combo units (a mini pumper of sorts) staffed with two firefighters, a police officer and a paramedic personnel. When this has been tried, it has been very successful, but only when the system is designed from scratch. Politics and empires will control change in the traditional departments. This will allow more units to be used and be capable of multitasking. It will end aerial ladder trucks responding to sick patient calls. It will deliver 250 gallons of water with a reel line that can handle most fires if they’re attacked quickly enough. And it will reduce the stagnant periods that so many paramedics normally experience. This means more pay for more skills, more units for quicker response times and more efficient use of resources. Tom Richards Via Jems.com 18 JEMS SEPTEMBER 2012 I was so excited to see the front cover of the July issue of JEMS. I couldn’t wait to read the article. But I was disappointed to see it was more of an opinion piece that didn’t tell us anything new. As far as response times go, they’re never fast enough. From the information I have, the main response time is initiating CPR within four minutes of arrest. Nobody has enough money or the technology to accomplish this through EMS alone. This is up to the bystander who calls in. As far as dynamic vs. static deployment goes, how many people reach the retirement age of 60 with 25–30 years running eight to 12 calls a day in a 12-hour period? If a patient can be transported to a hospital within the same amount of time it takes to do the paperwork required for a refusal, obtain the two required blood pressures, call their doctor or go through an on-call nurse to set up the appropriate treatment plan, the private ambulance service will choose the transport. Even the public EMS will choose this because it’s quicker to get the unit out to handle the call volume of a dynamic system. You start taking more than an hour on a call and you don’t transport the patient, and you need more ambulances on the street to make response times, which costs more money. Will communities really invest in their call-takers and call reporting systems? The catch is that if you don’t dispatch an ambulance right away and the call goes from a low-level to a high-level response, then you get dinged for not making the high-level response time because of the time it takes to go through the entire set of questions. If it takes four to six minutes to go through the whole questionnaire, then the ambulance is almost to the scene by the time the call-taker is finished (at least in the cities). You might as well keep sending ambulances. Bob Farley, EMT-P Author Jonathan D. Washko, BS-EMSA, NREMT-P, EMD, responds: Sorry for your disappointment. Unfortunately, I’m only given so many words and so much space to express concepts and ideas that quite honestly could fill volumes. You’re correct in your observation related to the initiation of CPR and the timeliness associated with starting effective chest compressions and survival. You are also correct that few can afford to provide a fourminute response time standard with first response or transport assets. You may note in my article I discussed the initiation of CPR by a variety of methods, the first being dispatch life-support (DLS). DLS is pre-arrival instructions given by trained emergency medical dispatchers following clinical algorithms that provide lay callers the instructions necessary to get care initiated before EMS arrives. In many communities that embrace this type of system, Hi Guys. No ambulance needed. I’m a paramedic and have cleared my C-spine already. illustration steve berry ‘New’ Methods? The article featured on the July JEMS cover, “Rethinking Delivery Models: EMS Industry May Shift Delivery Methods,” by Jonathan D. Washko, BS-EMSA, NREMT-P, EMD, garnered a great deal of interest from readers. What is ‘the new normal’ of EMS, and how do you embrace it? Also, a JEMS Connect discussion thread about the use of lights and siren at night generated a conversation among Facebook fans regarding this hot topic. Do they do more damage than help?
- 19. Watch Steve Berry and JEMS Editor-in-Chief AJ Heightman tell you why this book is a must-read!
- 20. LETTERS continued from page 18 pre-arrival instructions save countless lives through the immediate (within a minute or so of 9-1-1 activation) initiation of lifesaving treatments. My point is that response times do count in survival and many EMS systems that have improved response times (although they may not have published their findings) have also seen correlated improvements in cardiac arrest return of spontaneous circulation (ROSC) rates. The mechanism by which the response time improves may vary, for example, the use of dispatch life support or system status management or just adding more resources into the EMS system or a combination of these in order to yield improved clinical results. The point is that systems attempting to achieve this with traditional deployment methodologies are financially unsustainable for a variety of reasons. To your next concern regarding human sustainability, I agree. Workloads must be balanced in order to provide not just long-term financial stability but also the stability of our teams. Unfortunately, dynamic deployment (like any other tool) can be used for good or bad. It’s how the tool was used that matters. I know many individuals in balanced high-performance EMS systems that have worked their entire careers in the field and love the work they do. To your third point, regarding whether private entities will embrace the concepts associated with healthcare reform, my answer is that they’ll have no other choice. As I mentioned in the article, once the economic conditions change and population-based payments replace fee-for-service payment methodologies, a shift in how we have to deliver care will take place driven by market force innovation and the dollars available to provide care. As this shift occurs, our mission in EMS will also shift toward keeping patients out of the emergency department and placing them in the proper locus of care. Next, you’re correct in your concerns related to the legal risks associated with triage and care referral systems versus treating and transporting everyone. It is evident that the U.S. healthcare system practices risk avoidance in pretty much everything it does; however, if we’re to overcome these obstacles, we must shift from risk avoidance to risk tolerance, and the government will have to help us accomplish this through reform or some other mechanism. Finally, your point about performance-based contracting is spot on. Regulators will have to also evolve and create penalty and reward systems designed around new goals and objectives. We may also see a shift in the regulators moving from government-based ones toward payer-based or provider-based governance models as their bottom lines. Lastly, this little known excerpt from Jack L. Stout addresses many of my critics and is one of the impetuses that drives me to do what I do every day: “As EMS providers, we invite the public to literally trust us with their lives. We advise the public that, during a medical emergency, they should rely upon our organization, and not any other. We even suggest that it is safer to count on us than the resources of one’s own family and friends. We had better be right. Regardless of actual performance, EMS organizations do not differ significantly in their claimed goals and values. Public and private, nearly all claim dedication to patient care. Efficient or not, most claim an intent to give the community its money’s worth. And whether the money comes from user fees or local tax sources, the claim is the same. Our moral obligation to pursue clinical and response time improvement is widely accepted. But our related obligation to pursue economic efficiency is poorly understood. Many believe these are separate issues. They are not. Economic efficiency is nothing more than the ability to convert dollars into service. If we could do better with the dollars we have available, but we don’t, the responsibility must be ours. In EMS, that respon- sibility is enormous—it is impossible to waste dollars without also wasting lives.” Use of Lights Siren Lights for safety on scene ... but if it’s a residence, we will usually turn them off once we arrive and no sirens at night in town .... we live in a small rural community and traffic is generally not an issue. Leslie Lloyd Via Facebook This issue again ... Sigh. Sadly, we as a profession of caring, are stuck utilizing all emergency signaling devices to be recognized as an emergency operation. Litigation against our fellow professionals has consistently found us at fault when we try to be ‘reasonable’ to the public and run silent to aid a neighbor. Running silent draws the criticism that we don’t take the response seriously. Using the signaling devices wakes everyone up and gets us tagged as hooligans with no regard for the public. It is with a wince that I flip the switches and roll using the signaling devices as the lesser of the evils is not getting you and your department stuck in a lengthy and costly litigation should the untoward take place. David M. Neptune Via Facebook If the nature of the call merits an emergency response it gets one. An emergency response means lights AND sirens, not lights OR sirens. The time of day has nothing to do with it. JEMS Bob Upson Via Facebook Do you have questions, comments or concerns about recent JEMS or JEMS.com articles? We’d love to hear from you. E-mail your letters to editor.jems@ elsevier.com or send to 525 B St. Suite 1800, San Diego, CA 92101, Attn: Allison Moen. interesting FACT ABOUT a photo that ran in our August 2012 issue Photographer Kathy Keatley Garvey took this rare photo that won an international award and has drawn international acclaim on the Internet. It was named one of the top images of 2012 on Huffington Post and also was select as “Picture of the Day” on numerous websites. Garvey captured this image of a bee stinging Cooperative Extension apiculturist Eric Mussen of the University of California, Davis, Department of Entomology in the apiary of the Harry H. Laidlaw Jr. Honey Bee Research Facility, UC Davis. What’s unusual about this photo is that this sting was not a clean break; you can see the abdominal tissue being pulled out as the bee tries to leave. Kathy Keatley Garvey is a communications specialist with the UC Davis Department of Entomology and a former newspaper editor but enjoys taking macro photos of insects in her leisure time. She also writes a daily educational Bug Squad blog on the UC Agriculture and Natural Resources website; the blog, a volunteer blog, has garnered some 3 million hits in three years. 20 JEMS SEPTEMBER 2012
- 21. Choose 20 at www.jems.com/rs
- 22. PRIORITYUSE TRAFFIC NEWS YOU CAN Aurora Active shooter News media prematurely critiques incident AP Photo/Ed Andrieski J ust after midnight on July 21, moviegoers and responders in Aurora, Colo., were subjected to real-life horror and chaos when a heavily armed gunman dressed in full body armor exited and returned via a rigged door during a premiere showing of the latest Batman movie, “The Dark Knight Rises” and fired on the packed audience. The gunman killed 12 people and wounded 58 others. It was a horrific event, complicated by many factors: the early morning time, a dark environment both inside and outside the theater, and the presence of a chemical agent designed to debilitate the victims and make easier, less resistive targets. Not to mention the incident also involved the panicked and chaotic exodus of hundreds of moviegoers— many with serious injuries—who fled, in all directions not only from the fully packed room, but also into other nearby rooms, hallways and concession areas. Many horribly injured victims who fled from a multitude of exits sought help from the first public safety personnel they could find. In many cases, the first person of contact was a police officer. Although EMS and fire resources were on the scene and still responding, the multitude of factors presented above didn’t allow for a standard mass casualty incident (MCI) set up and action plan. A gag order by the judge overseeing the legal aspects of this case has limited the release of information about the incident and ability of responders to tell their side of the story. So it’s frustrating to read newspaper accounts and challenges about the way the Aurora Fire Department and their contracted ambulance provider, Rural/Metro Corporation, responded, treated and transported patients. The local media has been critical of the seemingly short supply of ambulances during the first 30 minutes of the incident. And much has also been written about the police transporting victims rapidly from the scene to definitive care. Any seasoned responder who has arrived on scene at an MCI knows that even under Police officers were thrust into a patient transportation role in Aurora. the best of conditions, a mass exodus of the out to be a key lifesaving effort—as it was injured and uninjured from an incident can when President Ronald Reagan was shot in be difficult to manage. Sorting out the injured Washington, D.C. and rapidly transported to in a dark parking lot and at multiple exit a trauma center in his limousine. JEMS will report on this major incident points is a complex task. The rapid transportation of victims from that scene with criti- when appropriate clearances are received. cal penetrating and exsanguinating gunshot Until then, don’t prejudge our colleagues in wounds in police vehicles may in fact turn Aurora. —A.J. Heightman, MPA, EMT-P Defending Their own The media was critical in initial reports of a slow EMS response of resources to the Aurora shooting, but JEMS Facebook fans quickly jumped to their defense: Michael Torchia: We can train for these situations but no two situations are ever the same, and we’re humans not robots. The press never says, “they did two things wrong but 100 things right.” Suzi Pierce-Green: I saw where our agencies were on the news saying they practice and prepare for such an event, and all I could think is NO MATTER how much you prepare it’s a charlie foxtrot and everyone just does their best. My hat is off to them in the great job they did! KimiAnn Corey: People need to understand we have a system/protocols we have to follow for that stuff. There were on scene within minutes, but they had so many patients in the parking lot bombarding [them] that they couldn’t just bypass. Bobby Dorrell: You’re not helping anyone if you as a responder get hurt. In a situation like that, scene safety is the top priority. Join the conversation at www.facebook.com/jemsfans Audio from Aurora shooting: www.jems.com/video/news/audio-colorado-theater-shooting 22 JEMS SEPTEMBER 2012
- 23. Federal Law Addresses Critical Drug Issues MS providers are patient advocates and voices for the sick, injured, and sometimes, even the deceased. During such events as the unfortunate mass shooting at the movie theater in Aurora, Colo., providers are often tasked with ensuring family members and relief agencies know about the status of the victims. Thankfully, Health Insurance Portability and Accountability Act (HIPAA) makes the sharing of critical patient information a little easier during an MCI. Disaster Relief Entities: HIPAA allows EMS providers to share information about a patient’s location, general condition or death with an agency that’s authorized to assist in disaster relief Pro Bono is written by attorefforts. This information can be shared with neys Doug Wolfberg, Ryan the disaster relief agency for the purposes Stark and Steve Wirth of of notifying a family member, a personal repPage, Wolfberg Wirth LLC, resentative of the patient or another person a national EMS-industry law responsible for the patient’s care. So EMS firm. Visit the firm’s website providers can release patient information at www.pwwemslaw.com for to such entities as the American Red Cross, more EMS law information. a state emergency management agency or another similar type of entity to enable that organization to contact someone who’s responsible for the patient’s care. Family Members and Friends: HIPAA also permits EMS providers to disclose information about a patient’s location, general condition or death to a patient’s family member, relative, close personal friend or any other person who might be involved in the patient’s care. Bystanders, however, are a different story. Even if a bystander is truly concerned about a patient’s welfare, or may have even assisted the patient before you arrived on the scene, you may not share patient information with them, unless the patient agrees. There are two rules that you must follow when providing patient information to relief agencies or family and friends: 1. If the patient is competent and able to make healthcare decisions, you should first obtain the individual’s agreement to share the information, or at least give him/her an opportunity to object. The patient’s verbal agreement is enough. You can also infer from the circumstances that the patient doesn’t object to you sharing the information. For example, if you ask the patient if there’s anyone you can contact and they say “my spouse,” you can infer that the patient is OK with giving information to the spouse. 2. If the patient is incapacitated, which is often the case in MCIs, then providers can disclose patient information if they believe that disclosure is in the best interests of the patient. HIPAA permits providers to use their best judgment here in gauging how much information they should share. Just remember to keep the patient’s Robert Kneschke/Dreamstime.com E Choose 21 at www.jems.com/rs www.jems.com SEPTEMBER 2012 JEMS 23
- 24. continued from page 23 best interests in mind and to not disclose more than the patient’s location, general condition or death. Finally, there’s always the concern about others overhearing discussions between two crew members or radio transmissions. But these types of inevitable disclosures are called “incidental disclosures” under HIPAA and generally don’t pose a HIPAA violation. In addition, if it’s necessary to ask a bystander, police officer, news reporter or other non-medical person to assist you in treating, moving or transporting a patient in a mass casualty situation, you may do so. HIPAA always permits you to share patient information for treatment-related purposes with any party who’s also involved in the treatment of the patient. And it isn’t a HIPAA violation to transport multiple patients in an ambulance or other vehicle. Sometimes, an emergency simply overwhelms the available resources, and HIPAA recognizes that incidental disclosures will occur. All of us at Page, Wolfberg Wirth would like to express our deepest sympathy for the victims and everyone affected by the tragedy in Aurora. We also express utmost gratitude to all of the responders who answered the call on that fateful morning, and those across the U.S. who continue to answer that call every day. We’re honored to represent an industry that’s solely committed to the care of others in need. The authors are all attorneys with Page, Wolfberg Wirth, a national EMS law firm. Visit the firm’s website at www.pwwemslaw.com for more information on a variety of EMS law issues. QUICK TAKE As emergency medicine evolves, the National Institutes of Health (NIH) recently opened an Office of Emergency Care Research (OECR) to bridge research from institute to institute and from academia to institute. At this time it’s composed of an office of two to three people, a working group of 23 and a steering group of five. Walter Koroshetz, MD, is its acting director. “This was the recommendation of a steering committee’s strategic plan to create this office. We want to be sensitive to all of our institutes,” he says. After five years of discussion with the NIH and the emergency medicine community, the creation of the office was announced late in July. The NIH is composed of 27 institutes, such as nursing, neurology and child health. With the new office, the many disciplines of research that fall under the huge tent of emergency medicine have the potential to work together better and become greater than the sum of their parts. “We all do emergency research. The OECR is a convergence point between those institutes,” Koroshetz says. Although still in its infancy, Koroshetz is excited about the prospects and will recruit a permanent director. “The time is right. Research in an emergency setting is more feasible now working with a good set of investigators. —Devin Greaney For more of the latest EMS news, visit JEMS.com/news Choose 22 at www.jems.com/rs 24 JEMS SEPTEMBER 2012
- 25. Choose 23 at www.jems.com/rs
- 26. LEADERSHIP SECTOR presented by the iafc ems section by gary ludwig, ms, emt-p First Day Now what? B ob is a newly promoted EMS manager who has been hired from another state to lead an EMS agency. On his first day, things didn’t go well. He came into the office and greeted only his secretary and next in command. People who wanted to meet him never got the chance because the second-in-command monopolized his time. The second and subsequent days went the same way. Bob never got out of the office. Soon, word trickled to those working in the field that the new boss was an unfriendly, aloof jerk. As could be predicted, everything went downhill from there. EMTs, paramedics, and people who worked in the EMS administrative offices really didn’t like Bob. He could never get everybody on board with the changes he wanted to implement. People within the EMS organization became resistant to him, didn’t like his approach and grumbled about every policy he issued. Within six months, Bob was looking for a new job because he wasn’t happy either. Within a year, the Board of Directors let Bob go. What did Bob do wrong? He had a wonderful track record in his other EMS organization, and he had a fantastic resume. What Bob failed to recognize is that if you’re the new leader of an EMS organization, it isn’t business as usual on the first day you walk through the door. recognized by the boss on the first day. Make sure you meet every employee, acknowledge them and give them a personal greeting— from the janitor all the way up to your secretary or the next in command. When you first enter a new organization as the new boss, you should remain positive. If you’re critical of the organization’s current operation—especially if you’re coming in from the outside—it might not go over well. People will see it as an attack on their organization. Even though you’re a part of the organization, you haven’t been accepted yet. Such statements as, “We did it this way where I just came from” may polarize you and your employees. Next, I recommend not changing any- A QI officer would show up at your station and make you sign the form acknowledging that you missed something. Quite frankly, it really pissed people off when the situation was their 12th trip of the day at 4 a.m. and they failed to check a box on the patient care report. It was one of the major things I heard, and it really seemed to set them off. I failed to see the significance of the form because it seemed to make the QI process punitive with having to sign the form acknowledging you did something wrong. So looking for the “low-hanging fruit” and looking for the chance to set the right positive attitude being the “new guy” coming in from the outside, I immediately got rid of the QI form. The response was overwhelmingly positive and upbeat. The crews were elated with my decision. They felt I was a good selection for the organization and I was going to move the EMS part of the fire department forward. It helped me consolidate support for some of the tough decisions I had to make down the road with changes that were necessary, while maintaining high morale. Make sure you meet everyone, acknowledge them give them a personal greeting. Your First Day I’ve always seen this as a make-or-break point. I’ve seen some good people get run out the door because of the way they came in the door. Everybody’s going to be watching what a new manager does and says, as well as observing how they react to different situations. If you’re a new EMS manager and have come in from the outside, your employees will really be watching you. My first suggestion is to say “hello,” and meet everyone. People want to feel important, and they certainly want to be 26 JEMS SEPTEMBER 2012 thing until you learn the works and the dynamics that make it function. It’s especially important not to change anything that has to do with the culture of the organization. If your first act is to change the patch or the name of the organization, expect a tremendous amount of resistance and trouble. People who are already within the organization have created their identity with the organization. Although some may grumble, they still take pride in the organization they’re associated with. Taking that away from them can only bring you headaches. My Experience When I came to Memphis seven years ago, I got around and talked to most of the firefighter/paramedics about the organization and how EMS operated in the department. One of the biggest complaints I heard was about a quality improvement (QI) form that was issued to everyone from a QI officer if you missed something on the patient care report. Conclusion Being new to an EMS organization is a challenge. If you’ve moved a great distance, there’s added stress with moving and finding housing. There’s no need to add to that stress by taking the wrong approach with your entry into the organization. Stay focused, observe and start slow. If you’re successful with your entrance, you will have an easier time down the road making the changes you think are necessary. JEMS Gary Ludwig, MS, EMT-P, has 35 years of EMS, fire and rescue experience. He currently serves as a deputy fire chief for the Memphis Fire Department. He’s also Chair of the EMS Section for the International Association of Fire Chiefs. He can be reached through his website at GaryLudwig.com.
- 27. Choose 24 at www.jems.com/rs
- 28. TRICKSour patients ourselves OF THE TRADE caring for by Thom Dick, EMT-P Stealth Mode Is all this noise really necessary? 28 JEMS september 2012 Photo Chris Swabb M y state has a law that says if your emergency warning lights are on during a response, your siren needs to be on as well. Always. Most laws here are pretty sensible. But like so many things that stipulate “always” or “never” in this business, this one’s goofy. There are times when the last thing you want to do is advertise your arrival or your intentions in advance. That’s true all the time in some neighborhoods. And it’s fundamental on interstates, where you pretty much have to expect other drivers to do silly things. Just for a moment, Life-Saver, put yourself in the mind of the motorist I’m about to describe. It’s close to dusk. You’re cruising home from work at 65 miles per hour, nodding to your favorite loud music. Suddenly and without warning, you’re overwhelmed by a pair of siren speakers that somehow got within 20 feet of your rear bumper. (Yep, that’s way too close.) In addition, your rearview mirror reveals a big blue, elliptical Ford sign with a few inches of a shiny grille around it, and its silver details reflecting the rhythmic flashers of—ohmigosh—an ambulance. (How’d that get there?) What would you do? Seriously, would you have a seizure? Wet yourself? Pull over quickly and switch places with your frontseat passenger? Slam on the brakes? Speed up and pull to the right without so much as a glance for traffic in the adjoining lane? Lower your window and wave for them to pass? Flip them off? Or turn up the music and drown out that awful woop-woop noise? Even a year of experience should tell you that if those options were actually offered on a driver’s license renewal test as multiplechoice answers, plenty of licensed drivers out there would consider at least a few of them as viable options. See, I don’t think most drivers are accustomed to making emergency decisions. And when they try, they sometimes make errors Ambulances should go into stealth mode during the night instead of flooding cities with unnecessary noise. in judgment. (At 65 miles per hour even the smallest errors can have big consequences, can’t they?) I think of emergency warning equipment as a tool. And I think its applications are generally different on city streets than on interstates. On city streets (at lower speeds), a siren keeps pedestrians on the sidewalk and helps an ambulance get people’s attention from behind so you can ask for the right of way. (Remember it’s ask, not demand.) On interstates, you use it instead to mitigate traffic flow once you’ve gotten past other motorists. But either way, you need the flexibility to choose which kinds of warning equipment to use in any given situation. (That might include no warning equipment at all, even during highpriority calls.) On interstates, the California Highway Patrol (CHP) routinely employs the use of no forward-facing lights and no sirens while they’re en route to interstate calls. The CHP has known for years that most drivers can’t hear a siren at higher speeds until you’re right on top of them. Most drivers also don’t monitor their rearview mirrors, so they tend to not notice those forward-facing lights anyway. Officers concentrate on sneaking through traffic without startling or scaring anybody. They try to use their rear-facing lights to advise drivers in their wake that they’re responding to an incident. That helps them explain their use of the shoulders, lane changes and sometimes speed. As emergency vehicle operators, it’s incumbent on us to think for other drivers. We should be doing no harm, not only medically but also in regard to our emergency driving. And as you know, we can do a lot of harm by causing just one other driver to panic. It’s time to abandon our outdated practice of flooding our cities and interstates with noise every time we respond to an emergency. It’s time for all emergency vehicle operators to consider some sort of stealthmode option as a matter of routine, especially on busy interstates. I also advocate one other thing, and I realize not everyone will agree with it. You can usually tell when your warning equipment is confusing people. When that happens, your safest option is to shut it down and advise your communications center that you’re cutting your “code” response due to traffic. That gives dispatchers the option of selecting a more appropriate unit for your call, or at least it tells them you’re going to be delayed. Delay is an acceptable option to hurting innocent people. Especially our own. JEMS Thom Dick has been involved in EMS for 41 years, 23 of them as a full-time EMT and paramedic in San Diego County. He’s currently the quality care coordinator for Platte Valley Ambulance, a hospital-based 9-1-1 system in Brighton, Colo. Contact him at boxcar414@comcast.net.
- 29. Choose 25 at www.jems.com/rs
- 30. CASE OF THE MONTH DILEMMAS IN DAY-TO-DAY CARE BY Travis Polk, MD, Carrie Sims, MD Life Limb Tourniquet saves man severely injured in vehicle crash I t’s easy for a current and former military physician working in a busy urban trauma center to look around and see the countless advances in trauma care that have been translated from the military to civilian experience. This month’s case highlights just one of the many lessons learned from caring for injured service members. When a 72-year-old male who was driving unrestrained in his sedan along the highway was suddenly struck from behind, he lost control of his vehicle and it rolled. His left arm, which was resting in the open window, was crushed. Philadelphia Fire Rescue medics arrived at the scene and found the patient in a large pool of blood with a severely deformed left arm dangling by what seemed to be a thin connection of soft tissue. There was profound, pulsatile bleeding. Medics applied a tourniquet to the arm above the injury and tightened it until the bleeding stopped. They then immobilized the patient on a spine board, obtained IV access and administered morphine for pain control, splinted his arm with blankets as best they could and transported him to the trauma center at the Hospital of University of Pennsylvania as a “trauma alert,” the highest level of activation. The patient remained hemodynamically stable during the transport. Hospital Course On arrival, the trauma team quickly completed a primary survey, attached the patient to monitors, exposed and rolled the patient, and obtained additional IV access. Initial vital signs were heart rate=126, blood pressure=162/100, respiratory rate=20, temperature of 96.9° F and pulse oximetry of 100%. His Glasgow Coma Scale score was 15. Secondary survey was notable for some spinal tenderness, abrasions on the back and the obvious near amputation/de-gloving deformity of the left forearm. The tourniquet was in place above the elbow, and the bleeding was 30 JEMS SEPTEMBER 2012 Photo Courtesy Travis Polk Prehospital Course This image shows the patient’s arm with a tourniquet shortly after arrival in the emergency department. stopped. A focused assessment with sonography in trauma (FAST) ultrasound exam showed no blood in the abdomen, and a chest X-ray was unremarkable. The tourniquet was carefully released to better examine the arm. This resulted in severe pain for the patient in the area above and surrounding the wound. Pulsatile bleeding appeared to emanate from the vicinity of the radial artery. A limited neurologic exam of the hand with the tourniquet released revealed no evidence of motor or sensory function during this brief interval. Because of the persistent bleeding, the tourniquet was reapplied. The patient remained in extreme pain and became agitated. At this point, since a neurologic exam had been performed and the patient would be going to the operating room (OR), the medical team proceeded with elective endotracheal intubation to provide adequate sedation and analgesia. Following intubation, the patient was brought to the computed tomography (CT) scanner for imaging of his head, C-spine, chest, abdomen and pelvis. No other injuries were identified. The Operating Room The patient was brought to the OR and underwent repair of the radial artery, ligation of the ulnar artery, external fixation of the radius and ulna, extensive irrigation and debridement of devitalized tissue, and wound coverage with cadaveric skin. He was extubated the following morning, and examination of his hand revealed mostly intact sensation and slight movement in his thumb and fingers. Of note, the patient’s medical history was significant for coronary artery disease and deep vein thrombosis. On initial evaluation, he reported taking aspirin, clopidogrel and warfarin. He was treated with vitamin K via IV and transfused with fresh frozen plasma and platelets for presumed drug-induced coagulopathy. His initial hemoglobin was 10.3 gm/ dL with an international normalized ratio of 1.1. Given his history of significant blood loss and ongoing hemorrhage, he was transfused three units of packed blood cells in the OR. His tetanus status was unknown, so he received a tetanus vaccine. He was treated with broad spectrum antibiotics for his open, severely contaminated fracture. At the time of this article, the patient had left the intensive care unit, but he remained in the hospital three weeks. On
- 31. the road to salvation of his limb, the patient had five surgeries, including placement of antibiotic impregnated beads and free-flap tissue transplantation. Exsanguinating hemorrhage from isolated extremity trauma in the civilian setting is rare. Unfortunately, due to mixed messages in much of the civilian medical literature and first aid texts, many providers are hesitant to place a tourniquet for fear of causing further injury or committing the patient to an amputation. The military experience during the past several years, however, has demonstrated how this simple technology can be both lifeand limb- saving. Historically, the mortality rate from exsanguination from extremity trauma on the battlefield has been approximately 9%.1 A retrospective study of special operations personnel deaths in the global war on terror found that 13% of the potentially preventable deaths might have been prevented with a tourniquet.2 Likewise, a large prospective study examining the use of prehospital and emergency department tourniquet use in a combat support hospital in Iraq found that early use of tourniquets not only provided hemorrhage control but also improved mortality. In a series of more than 400 applied tourniquets, no amputations were associated with inappropriate tourniquet use, and few were associated neurologic complications.3 For these reasons, in 2005, the U.S. Army adopted a new standard Tactical Combat Casualty Care guideline that tourniquets should be first-line treatment for any life-threatening extremity trauma while under fire. Although extremity trauma in the civilian setting is rare, studies show that it’s deadly. A similar retrospective study of exsanguinating extremity trauma in the civilian population identified 14 patient deaths during a period of five and a half years at two Level 1 trauma centers in Houston. Of these 14 patients, 57% had wounds that would have been amenable to the placement of a tourniquet, and therefore potentially could have been saved.4 Conclusion Given this information, civilian EMS providers should feel confident that placing a tourniquet for severe extremity hemorrhage that isn’t controlled by other means is safe, appropriate Radiograph Courtesy Travis Polk Discussion This plain radiograph shows the severely comminuted fracture of the patient’s forearm. and life-saving. Studies also show they should be applied early and before the patient is in shock.3 A variety of tourniquets are available for EMS use. EMS units should work with their medical directors to select and train with the device that best suits their needs. As this case illustrates, the use of a tourniquet was lifesaving for this patient and should always be considered in cases of severe extremity trauma. JEMS Travis Polk, MD, is a trauma surgeon on active duty in the U.S. Navy currently stationed at the Naval Medical Center in Portsmouth, Va. He is board certified in general surgery and board eligible in surgical critical care. At the time of this case, he was an instructor in surgery and fellow in traumatology, surgical critical care and emergency surgery at the University of Pennsylvania in Philadelphia. He can be contacted at travis.polk@med.navy.mil. Carrie Sims, MD, is an assistant professor of surgery at the University of Pennsylvania in Philadelphia and is a former U.S. Army Reserve Medical Corps Officer. She is board certified in surgery and surgical critical care and practices as a trauma surgeon and surgical intensivist. She can be contacted at Carrie.sims@uphs.upenn.edu. Disclaimer: The views expressed in this presentation are those of the author and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. government. Dr. Polk is a service member. This work was prepared as part of his official duties. Title 17, USC, §105 provides that “Copyright protection under this title is not available for any work of the U.S. government.” Title 17, USC, §101 defines a U.S. government work as a work prepared by a military service member or employee of the U.S. government as part of that person’s official duties. References 1. Bellamy RF. The causes of death in conventional land warfare: Implications for combat casualty care research. Mil Med. 1984;149(2):55–62. 2. Holcomb JB, McMullin NR, Pearse L, et al. Causes of death in U.S. Special Operations Forces in the global war on terrorism: 2001–2004. Ann Surg. 2007;245(6):986–991. 3. Kragh JF, Walter TJ, Baer DG, et al. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg. 2009;249(1):1–7. 4. Dorlac WC, Debakey ME, Holcomb JB, et al. Mortality from isolated civilian penetrating extremity injury. J Trauma. 2005;59(1):217–222. When placing the tourniquet, providers should remember the following: ighten until all bleeding stops. If the wound is still bleeding, you likely have a venous tourniquet, and it T may need to be tightened further or repositioned in order to occlude all arterial inflow. lace as low on the extremity as possible. P ote the time that the tourniquet is applied. (Paperwork gets lost and people don’t always listen during the N report, so write it on the patient too!) ourniquets are extremely painful; administer some pain medication. T www.jems.com SEPTEMBER 2012 JEMS 31
- 32. RESEARCH REVIEW ems What current studies mean to by David Page, MS, NREMT-P Effective Care Studies measure CO-detection device nausea treatment I CO-Oximetry Effectiveness I Weaver L, Churchill S, Deru K, et al. False positive rate of carbon monoxide saturation by finger probe oximetry of emergency department patients. Respir Care. 2012 Jul 10. [Epub ahead of print] hould you trust your pulse CO-oximeter (SpCO) monitor? During the past few years, there have been conflicting messages about the accuracy of these devices. This Salt Lake City-based emergency department (ED) group attempted to answer that question by comparing Masimo RAD-57 SpCO monitor readings from a finger probe/sensor, to the carboxyhemoglobin (COHb) readings from a simultaneous blood draw. Three lab technicians collected SpCO and COHb samples on 1,363 ED patients receiving blood draws from April to August 2008. This was a non-randomized sample of convenience study conducted at a single hospital. The authors report that 84% of the study’s population was light-skinned and 45% were male. Fifty-two of the people studied were non-smokers. A variety of patient complaints existed, but the SpCO monitor flagged 122 patients, meeting a false positive criteria. A false positive was considered if the SpCO showed a value greater than a 3% point difference than the actual COHb level. Only four patients were actually diagnosed with CO poisoning from the entire sample. In these cases, the SpCO oximetry monitor reading was 4–14% lower than COHb blood levels, which led the authors to conclude that the RAD-57 reports lower numbers than COHb. So far so good, right? Well, three other patients with COHb greater than 10% received a 0% rating on the SpCO monitor. If the SpCO value of 0% had been used as a field triage tool, then these patients may have not received necessary evaluation and treatment at an ED. So what should we conclude? First, the good: Previous studies have followed some flawed methodologies and didn’t adequately describe the details of their methodologies. 32 JEMS SEPTEMBER 2012 Photo david page S Researchers analyzed the false positive rate of carbon monoxide saturation on the RAD-57 monitor. (See a review by Keith Wesley, MD, FACEP, and Marshall Washick, NREMT-P at www. jems.com/article/patient-care/rad-57-pulseoximeter-performa.) The authors of this Salt Lake City hospital study were careful to describe their methods and avoid some of the previous pitfalls of other researchers (e.g., timing of the blood draw). The authors did not report whether the sensors were shielded from excessive ambient light, if patient motion was reduced, or if the various sensor sizes were used, which are each important considerations with the Masimo CO-Oximeter. They did report that the device performed within the margin of the manufacturer’s specifications. And, from a purely statistical and research perspective, the sample of patients with detectible CO levels is simply too small to make any meaningful conclusions. The concern a study like this presents is that, if we are to use this device for prehospital triage of potential CO exposures, then it would be preferable that the device would be sensitive enough to detect any potential exposure, and perhaps err on the side of over-triaging. Sending someone home based on a RAD-57’s “0” or low reading if that patient was actually sick, could be disastrous. Regardless of whether this was an operator or machine error, I worry about the patients with 0% readings who had elevated blood COHb readings. I would feel pretty terrible sending someone home only to find out they had a treatable condition that caused them harm because of my lack of action. The controversy will continue, but this is an important reason never to just base your field triage decisions on any machines. Instead, providers should use these devices in conjunction with other assessment processes and treatment tools, particularly when patients have potentially been exposed to CO or have CO symptoms. I Nausea Cure? I Fullerton L, Weiss S, Forman P, et al. Ondansetron oral dissolving tablets are superior to normal saline alone for prehospital nausea. Prehosp Emerg Care. 2012. [Epub ahead of print.] T his prehospital cohort study compared the use of normal saline bolus with an odansetron orally dissolving tablet (ODT) for the treatment of nausea. Researchers enrolled 274 consecutive patients to receive Bottom Line What we know: The RAD-57 is being used by many systems across the country. The machine has shown great promise and helped identify many CO exposures. Previous research has raised concerns regarding its accuracy. What these studies add: This study provides very weak evidence of a possible 9% false positive rate and confusion about the trustworthiness of a low RAD-57 number based on only five patients. More rigorous study is needed before any conclusions can be made. Providers are encouraged to talk to their medical directors and be sure to receive proper orientation and training before using any medical device.
- 33. normal ODT during a four-month period. As you would have predicted, the ODT group showed significantly decreased nausea symptoms. No amount of normal saline was able to show a significant effect. No adverse events were reported, and the two groups of patients were similar in ages and severity of nausea. This study shows a clear win for odansetron and for ALS care making a difference. Kudos to this group for doing prehospital research. Many of us have seen odansetron work its magic, but having some science to back up its safe and efficacious use makes for a more scientific and professional care standard. JEMS I watch box I Blanchette C, Dalal A, Mapel D, et al. Changes in COPD demographics and costs over 20 years. Journal Med Econ. 2012. [Epub ahead of print.] This cross-sectional, population-based study should pique the curiosity of community paramedic advocates. They report rapidly rising inhospital admission costs and more prevalence of chronic obstructive pulmonary disorder (COPD) in women. This survey of 416 respondents shows a 37% increase in the cost of caring for COPD during the past 20 years. The authors conclude that COPD has become a costly disease, which is now more prevalent in women than men. The authors recommend shifting costs to fund prevention and conducting follow-up efforts to avoid readmission of patients back into the hospital. Perhaps the community paramedic model will play a role in improving this part of the healthcare system. Choose 26 at www.jems.com/rs I glossary I Sample of convenience: A sample of convenience is a grouping of research subjects or values collected because they were easily available. They aren’t randomized or otherwise scientifically selected, and generally they’re not representative of or able to be generalized to an entire population. Visit www.pcrfpodcast.org for audio commentary. David Page, MS, NREMT-P, is an educator at Inver Hills Community College and a paramedic at Allina EMS in Minneapolis/ St. Paul. He’s a member of the Board of Advisors of the Prehospital Care Research Forum. Send him feedback at dpage@ehs.net. Choose 27 at www.jems.com/rs www.jems.com SEPTEMBER 2012 JEMS 33
- 34. Feedback-driven team performance impacts survival By Jeffrey M. Goodloe, MD, NREMT-P, FACEP; T.J. Reginald, NREMT-P; David S. Howerton, NREMT-P; Jim O. Winham, RN, BSN, NREMT-P; Tammy Appleby, NREMT-B 34 JEMS SEPTEMBER 2012
- 35. Photo David Howerton EMS providers go back to the basics in training for cardiac resuscitation. A s EMS professionals, we’re routinely challenged to successfully resuscitate victims of sudden cardiac arrest. Fortunately, our understanding of cardiac arrest pathophysiology continues to grow. More fortunate still, our enthusiasm in translating that understanding to effective therapies has never been greater. In the August 2012 issue of JEMS, we introduced a comprehensive restructuring of the EMS System for Metropolitan Oklahoma City and Tulsa’s cardiac arrest program using a three-part approach: chest compression fundamentals, resuscitation team dynamics and accelerated feedback on resuscitation performance. We discussed the benefit of going “back to the basics” of chest compression fundamentals training, increasing our rate to 120 chest compressions per minute and using metronomes to attain and maintain that rate throughout resuscitations. Now, we share how those fundamentals were incorporated into a Resuscitation Team Playbook and how we use directed feedback to further refine resuscitation performance. For Step 1 and the introduction to this team’s approach to resuscitation, read “Oklahoma EMS System Strives for Higher Cardiac Arrest Survival Rates” at www.jems.com /magazines/2012/august. Step 2: Resuscitation Team Dynamics. Have you ever been a part of an EMS call that was particularly “busy” in activity, yet when the patient was transferred for further care, you started to think, “What did we actually get done?” Us too. In fact, it happens to all of us in www.jems.com SEPTEMBER 2012 JEMS 35
- 36. cardiac Arrest part II continued from page 35 the inherently challenging practice of EMS medicine. We believe what you do with those reflections can make all the difference in the world for future patients. We therefore chose to turn our reflections, and those of our colleagues, into a Resuscitation Team Playbook that channels individual enthusiasms into a carefully orchestrated team performance, often described favorably as “pit crew resuscitation.” Figure 1 shows the positions used in our resuscitations, with roles defined for teams of one to six professionals. In our EMS system, we often start with resuscitation teams of two, three, or four, with subsequently arriving responders building that team to five or six actively contributing members. It’s rare in our system that one EMT or paramedic would be tasked with resuscitating a cardiac arrest patient alone, but it could happen for a brief period if a patient were to collapse at a nearly empty fire station or ambulance headquarters. We wanted to ensure we had all the possibilities covered, including the single rescuer scenario. Let’s review the key contributions provided by each position, so that you’ll be certain to include the care most likely to promote neurologically intact survival, regardless of resuscitation team size. Position 1: Rapidly identifies arrest and initiates continuous chest compressions. lternates minutes of chest compressions with Position 2 A over the course of the resuscitation. When not compressing, assists with bag-valve-mask ventilations (squeezing the bag). inimizes pauses in chest compressions for rhythm deterM mination and/or defibrillation. Position 2: Applies automated external defibrillator or monitor/ manual defibrillator. irror image of Position 1. M Position 3: Provides airway management; avoids hyperventilation. Position 4: Leads scene management. Interface with family/bystanders for events preceding arrest and medical history. upervises positions 1–3 for continuous compressions, S timely defibrillation, and no hyperventilation. Position 5: Provides ALS support. hythm determination and manual defibrillation. R Vascular access. Medication administration. Position 6: Provides ALS support. Patient management leader. The full playbook can be accessed at www.jems.com/patient-care At first, it looks like a lot of instruction—because it is. However, these directives simply expand in detail on the key contributions at each position. You may think this degree of directive is micromanaging hardworking EMS professionals who already know the right things to do in time-sensitive situations. You’re right; it actually is micromanaging, but let’s look at why cardiac Choose 28 at www.jems.com/rs 36 JEMS SEPTEMBER 2012
- 37. arrest calls for no less. Try this exercise, literally. Do 20 jumping jacks. What do you feel? Unless you’re in particularly athletic shape, you likely feel an increase in pulse and in respiratory rate and effort. Why? You’re compensating for an increased activity demand. The human body is amazing in its ability to compensate, even to some degree when severely ill or injured. But spontaneous circulation reflects an unforgiving light switch. When it’s “on,” compensation is at work. When it’s “off,” as in cardiac arrest, there’s complete loss of compensation … except for resuscitative efforts. Thinking back to our understanding of cardiac arrest pathophysiology, we have to be precise in those efforts for our “compensation on loan” to work. The only way to make that happen comes when we use a carefully crafted plan (the playbook) and actively micromanage ourselves in each position (running the play). So in sum, it’s not micromanaging by others, it’s self-micromanaging, and it’s for all the right reasons. Figure 1: Resuscitation Positions Scene Management P4 Airway Management P3 Chest Compressions Set Up AED/Defibrillator Chest Compressions P1 Defibrillation Vascular Access Medication Administration P2 Patient Management P5 P6 We’ve definitely laid out a plan, but how do we know whether it’s the right plan? One quick answer you’ll say is by looking at neurologically intact survival rates—before and after adoption of this plan. In fact, that’s a great answer, but we think it comes up short as the lone answer. In athletics, if a team loses a game, does that mean they played badly? Often, the answer is “not at all;” it may mean the team simply played a better team, or depending on how score is kept, the team may have started with a handicap that’s insurmountable. Ever start a resuscitation feeling that you were working with such a handicap? That’s where Step 3 comes into use in our cardiac arrest program. Step 3: Feedback on Resuscitation Team Performance. Every highperformance professional values feedback designed to “build up” future abilities. Our feedback program channels that philosophy using proprietary software that captures data from the monitor/ Choose 29 at www.jems.com/rs
- 38. cardiac Arrest part II continued from page 37 defibrillator throughout the resuscitation. Many EMS systems are using this type of capability, but the real value lies in merging data with a set of skilled clinical eyes, annotating the basic feedback forms. Credit goes to the Redmond, Wash., Medic One program for helping us see the full potential already in our grasp. Only through annotating a case do specific gaps in compresEMS providers in Oklahoma City and Tulsa maintain a rate of 120 compressions, using metronomes in training. Photo David Howerton Choose 30 at www.jems.com/rs sions, changes in ventilation rates and timings of defibrillation really become clear. No “real world” resuscitation will ever be textbook perfect. Thus, only through analysis by an experienced clinician does variability reliably fall into the “makes sense” or “opportunity to reflect” categories. Without annotation, a “report card” gets generated without showing a valid grade … arguably pointless, right? Our goal is to have an annotated resuscitation team performance feedback report available to the resuscitation team on its next shift after working a cardiac arrest. The report is sent with explanation through annotated comments and without discouraging remarks, even in areas for improvement. Those areas are self-evident, and we believe the best correction can come through team reflection. So how are we doing in achieving our own goal? Currenrtly, just about 5% of the time. But here’s a key point, and one we’ve had to learn with hard experience: If you wait until everything is perfect to start improving, you never start improving. Like 38 Choose 31 at www.jems.com/rs JEMS SEPTEMBER 2012
- 39. most EMS systems, we’re understaffed in comparison with our goals. However, we’re fortunate in being able to hire a new data specialist position that’s dedicated full-time in our Office of the Medical Director. This position will dramatically improve our feedback abilities, both in volume and timeliness. Even with feedback 5% of the time, the results are encouraging. We’re routinely seeing chest compression fractions (CCF) (i.e., time in which chest compressions are actively occurring) above 90%. In fact, many resuscitations are being performed with CCFs above 95%. (To be clear, these cases reflect random analysis, not just review of clear survivors.) These numbers reflect CCF increases 5–15% above our historical baselines. Not surprisingly, return of spontaneous circulation (ROSC) rates have increased since we started resuscitation team dynamics in February. Although we anticipate cardiac arrest survival rates in 2012 to be rewarding, it’s still early, and we don’t want to report on incomplete data. Conclusion (For Now) Our EMS system, just like yours, is committed to attacking cardiac arrest and doing everything we can to help the suddenly dead become alive again. Focusing our energies (with encouragement from friends throughout EMS) on chest compression fundamentals, resuscitation team dynamics and better timely feedback on resuscitation team performance—all in support of patients and the EMS professionals caring for them—makes a lasting influence on cardiac arrest. JEMS Jeffrey M. Goodloe, MD, NREMT-P, FACEP, is professor and chief of the EMS section of the Department of Emergency Medicine at The University of Oklahoma School of Community Medicine in Tulsa. He serves as medical director for the Medical Control Board in the EMS System for Metropolitan Oklahoma City and Tulsa, working with a multitude of agencies, including the Emergency Medical Services Authority (EMSA), the Oklahoma City Fire Department and the Tulsa Fire Department. He started in EMS in 1988 as an EMT-B and has never quit learning. Contact him at jeffrey-goodloe@ouhsc.edu T.J. Reginald, NREMT-P, is director of research and clinical standards development for the Office of the Medical Director in Oklahoma City and Tulsa. He’s a driving force behind the success and continuing advancement of cardiac arrest resuscitation in the major metropolitan areas of Oklahoma. His EMS career spans three decades and includes a multitude of clinical and administrative leadership roles. Contact him at reginald@emsa.net. David S. Howerton, NREMT-P, is director of Clinical Affairs - Western Division for the Office of the Medical Director in Oklahoma City. He’s the medical oversight liaison officer for all metropolitan Oklahoma City agencies working with the Medical Control Board. His EMS career spans nearly three decades and includes a multitude of clinical and administrative leadership roles. Contact him at howertond@emsa.net. Jim O. Winham, RN, BSN, NREMT-P, is the immediate past director of Clinical Affairs - Eastern Division for the Office of the Medical Director in Tulsa. He’s enjoying a new career move as the general manager for Paramedics Plus - Oklahoma. His EMS career spans more than three decades and includes a multitude of operational, clinical and administrative leadership roles. Contact him at winhamj@emsa.net. Tammy Appleby, NREMT-B, is executive assistant to the medical director for the Office of the Medical Director in Oklahoma City and Tulsa. Retired from the U.S. Air Force, she has an accomplished career in medical operation administration and leadership. Contact her at applebyt@emsa.net. Choose 32 at www.jems.com/rs
- 40. Photo Courtesy Portland Fire Department Once adenosine is administered, its effectiveness lasts between five and 10 seconds. 40 JEMS SEPTEMBER 2012
- 41. Expert safe use of adenosine depends on patient’s cardiac status By Corey Slovis, MD, FACEP; Jared McKinney, MD; Jeremy Brywczynski, MD, FAAEM denosine is the drug of choice for paroxysmal supraventricular tachycardia (PSVT) and is once again Advanced Cardiac Life Support-approved for differentiating PSVT with aberrancy from ventricular tachycardia (v tach) in patients with monomorphic wide complex tachycardias.1 Adenosine is a potent and safe antiarrhythmic when used appropriately. However, its use in the wrong patient or rhythm can prove fatal. This article focuses on how to expertly use adenosine and to know when this “safe” antiarrhythmic can be dangerous and contraindicated. Pharmacology Mechanisms of Action Adenosine’s mechanism of action can be thought of as a “temporary paralyzing” of supraventricular tissue. Pharmacologically, adenosine hyperpolarizes the cell by stimulating an inward potassium current and temporarily inhibiting calcium migration.2 In doing so, the pacemaker activity of the sinoatrial (SA) node, spontaneous atrial activity and conduction through the atrioventricular (AV) node are dramatically slowed or temporarily stopped. Adenosine has no effects on accessory pathways, such as those seen in the Wolf-Parkinson White Syndrome (WPW). Mild side effects of adenosine are common. They include a transient sinus pause that usually lasts less than five seconds, chest pressure or tightness, dyspnea, facial flushing and the feeling of impending doom (see Table 1, below).2–4 Rare, benign side effects reported include anxiety and dizziness. In one large prehospital trial, 11% of patients had a minor transient complaint, with chest pain being the most common complaint seen in 4% of patients.4 Chest tightness was induced by adenosine administration in 83% of patients in one large in-emergency department (ED) study.5 to cause prolonged sinus pauses, syncope, seizures and even asystole, although this rare side effect has been described almost solely in older patients with preexisting conduction disease and/or second- or third-degree heart block.7–9 Adenosine is the drug of choice for PSVT in pregnant patients.1 The biggest dangers with adenosine are seen in two groups of patients: 1) those with atrial fibrillation or atrial flutter, and 2) those in sinus tachycardia and not PSVT. Figure 1a, 1b 1c: Regular Wide-Complex Tachycardia Figure 1b Side Effects Side effects from adenosine administration that are serious are extremely rare when used in healthy patients with PSVT (see Table 1, below). Adenosine may cause mild bronchospasm, which is almost always short lived. However, adenosine can also cause severe bronchospasm and should Table 1: Toxicology of Adenosine be given carefully to Minor Major those with a history of asthma or chronic Chest tightness Angina obstructive pulmoShortness of breath Ventricular tachycardia nary disease (COPD).6 Warmth Bronchospasm It shouldn’t be given to patients who are already Diaphoresis Respiratory arrest wheezing. Adenosine Impending doom Cardiac arrest has also been reported Figure 1c To verify true regularity, make marks on a piece of paper that match the peaks of the QRS then moving the QRS-marked paper a few beats over to compare it to three to four new beats on the rhythm strip. If they line up, the rhythm is regular; if they don’t, the rhythm is irregular, and adenosine shouldn’t be used. www.jems.com SEPTEMBER 2012 JEMS 41
- 42. Check the Rhythm continued from page 41 Numerous studies in the literature report serious rhythm degeneration and even death when adenosine has been inadvertently given to patients with either atrial fibrillation or atrial flutter. Adenosine can convert relatively stable atrial flutter with 2:1 conduction and a heart rate of 150 to 1:1 conduction with a heart rate of 300 and cause rapid clinical decompensation.10 Adenosine slows or blocks antegrade (atrial to ventricular) conduction through the AV node but doesn’t affect accessory or bypass tracts like those seen in WPW syndrome. Because of this, adenosine can be dangerous when given to patients with atrial fibrillation, especially if they have a bypass track. Numerous reports show patients degenerating into rapid atrial fibrillation with rates at 250 or greater and becoming hemodynamically unstable.10–13 Thus, an absolute contraindication to adenosine exists in patients who have either atrial flutter or an irregular rhythm in atrial fibrillation. Because rapid atrial fibrillation may seem regular on ECG monitor, paramedics are urged to run a rhythm strip and verify true regularity. We find this easiest by making marks on a piece of paper that match the peaks of the QRS then moving the QRS-marked paper a few beats over to compare it to three to four new beats on the rhythm strip. If they line up, then the rhythm is regular; if they don’t, then the rhythm is irregular (and likely atrial fibrillation), and adenosine shouldn’t be used (see Figures 1a, 1b, 1c, p. 41). The other absolute contraindication to adenosine is in sinus tachycardia. Dehydrated patients, especially the elderly with fever, failure to thrive and/or an infection may appear to be in PSVT when in fact they’re barely compensated with a sinus tachycardia with a rate that may be greater than 150. These patients are at high risk for morbidity and mortality if adenosine is administered, Table 2: When PSVT is not likely PSVT Presentation Reason It Is Not PSVT Heart rate of 150 or less At 150 atrial flutter 1:1; 150 or less usually is sinus tach Irregular rhythm Atrial fibrillation or multifocal atrial tachycardia Transiently slows to vagal stimulation Diagnostic of sinus tachycardia History of atrial fibrillation, atrial flutter or multifocal atrial tachycardia (MAT) Marked increased likelihood of previous arrhythmia and not PSVT History of COPD or CHF Atrial fibrillation or MAT much more likely Choose 33 at www.jems.com/rs 42 JEMS SEPTEMBER 2012 Choose 34 at www.jems.com/rs
- 43. and they have a prolonged sinus pause (see Table 2, below). In cases for which there’s any chance that sinus tachycardia is the etiology of the patient’s elevated heart rate, a rapid fluid bolus of 250 cc should be administered. Any slowing by just a few beats per minute (rather than a dramatic conversion to a normal sinus rhythm) confirms the diagnosis of sinus tachycardia due to volume depletion. This is also true in heat stroke victims with PSVT at rates approaching 180 beats per minute. EMS providers should rapidly hydrate and cool these patients before administering adenosine. If the patient’s pulse begins to fall with therapy, the diagnosis of sinus tachycardia due to heat illness and dehydration is confirmed, and adenosine is contraindicated. Table 2 lists the rhythms, rates and patient types in which the diagnosis of PSVT should be considered unlikely. Administration Dosage Once adenosine is administered, its effectiveness lasts only between five and 10 seconds because it’s rapidly metabolized by cellular uptake. Because of the ability of blood vessel endothelium to metabolize adenosine, it’s imperative for EMS providers to give adenosine by rapid bolus followed by Figure 2: Prolonged Pause Status Post Adenosine Choose 35 at www.jems.com/rs a 10–20 cc rapid flush.2,3 Larger, more proximal IV lines are preferred because small-bore IVs don’t routinely allow fast flow or rapid transit to the heart. The dosage of adenosine should be reduced to 3 mgs if injected into a central line, and it shouldn’t be used in heart transplant patients.1,14 The standard initial recommended dosage of adenosine is 6 mg, followed by a rapid saline flush. If this dose isn’t effective, EMS providers should double the dose to 12 mg, repeat the bolus and rapidly flush the line.1– 15 These recommendations come from the original article that compared adenosine
- 44. Check the Rhythm continued from page 43 Table 3: Dosages Protocol for Adenosine Administration Adenosine Dosing 6–12 mg IV push in large-bore IV Immediately flush with 10–20 cc normal saline solution 12 mgs IV push if not effective in 60 seconds If protocol began with 6 mg IV, consider second dose of 12 mgs IV; push and re-flush line. Contact medical control in the event of refractory cases with verapamil in PSVT and used a variety of adenosine doses. In this article, the investigators found that 6 mg of adenosine converted 62.3% of patients and that 12 mg converted 91.4% of patients without increase in toxicity.15,16 Because there doesn’t appear to be any increased toxicity in a 12 mg initial dose and it’s more effective, others have recommended starting at 12 mg.4,17 Some have recommended doses as high as 18 mg, which can convert 95% of PSVT patients vs. 65% with 6 mg and 90% with 12 mg.18 Thus, paramedics and their medical directors should have pre-established protocols beginning with 6–12 mg. These protocol should conclude that a second 12 mg dose should be attempted if 12 mg is ineffective,. This is because reports show a second repeat dose of 12 mg may convert up to 10–31% of patients.4,5 Treating Wide Complex Tachycardia Adenosine was initially considered useful in helping distinguish wide complex tachycardias due to aberrantly conducted PSVT vs. true v tach. However, based on cases of patients deteriorating, many cautioned against trying this drug in any patient with wide complex tachycardia.14,16 We now know that adenosine is safe and can help distinguish supraventricular arrhythmias from those originating in the ventricle for monomorphic wide complex tachycardias that are regular in rate (and by definition, have the same QRS size and shape).1 In the largest recent study of adenosine in wide complex tachycardias, 197 patients were studied.16 Of these, 116 had SVT and 81 had v tach. Ninety percent of the SVTs responded to escalating doses of adenosine (i.e., administering 6 mg, then 12 mg, then repeating 12 mg if no response, and even administering 18 mgs to one patient). Only 44 JEMS SEPTEMBER 2012 one patient with proven v tach responded to adenosine, and a second patient may have transiently slowed. The authors concluded that adenosine was safe as long as patients had regular monomorphic wide complexes and that adenosine was useful in helping distinguish between PSVT and v tach. In fact, they noted a 36-fold increase in the likelihood of a adenosine are usually mild and transient, lasting just a few seconds. They include chest tightness, shortness of breath and a short sinus pause. Although more serious side effects can occur, such as hypotension, bradycardias and seizures, these side effects are rare in healthy patients with no underlying heart disease. Adenosine is contraindicated in patients who are likely to be harmed by its inappropriate use. Patients with irregular heart rates, especially atrial fibrillation, patients with PSVT mimics such as atrial flutter with 2:1 conduction or sinus tachycardia in a dehydrated or stressed patient should never receive adenosine. Adenosine should never be used in wide irregular tachycardias. Providers who are going to use adenosine must be experts in An absolute contraindication to adenosine is in patients who have either atrial flutter or an irregular rhythm as is seen in atrial fibrillation. supraventricular origin if the wide complex tachycardia converted to sinus with adenosine and a nine-fold increased likelihood of v tach if it didn’t respond to escalating doses of adenosine. Another thing is absolutely clear: Never give adenosine to a wide irregular tachycardia or a polymorphic (multiple different QRS configurations) tachycardia, such as Torsades de Pointes. It’s in these patients that adenosine might be lethal.1,16 Read about a real case of a patient who presented with Torsades de Pointes at www.jems.com/ torsades-de-pointes. Summary, Conclusion Recommendations Adenosine is a safe and effective agent in PSVT. It’s currently the EMS drug of choice for regular tachycardias about 150–160 beats per minute, believed to be PSVT— whether wide or narrow. The side effects of cardiac rhythm interpretation. They also must carefully review a rhythm strip prior to drug administration. Our recommended starting dosage is 12 mgs via IV push followed by a 10–20 cc rapid flush of saline. If the first 12 mg dose isn’t effective after one minute, we recommend repeating 12 mgs a second time. EMS services and their medical directors should decide whether 6 or 12 mgs should be initially used because there’s no national consensus on which is optimal. JEMS Corey Slovis, MD, FACEP, is professor and chair of emergency medicine at Vanderbilt and serves as the medical director for Nashville (Tenn.) Fire Department and Nashville International Airport. Slovis is also a member of the JEMS Editorial Board. Jared McKinney, MD, is director of event medicine for Vanderbilt Medical Center, an assistant professor of emergency medicine at Vanderbilt University Medical Center in Nashville and is an assistant medical director for the Nashville Fire Department. Jeremy Brywczynski, MD, FAAEM, is medical director of Vanderbilt’s aeromedical LifeFlight Program and an assistant professor of emergency medicine at Vanderbilt
- 45. University Medical Center in Nashville and is an assistant medical director the Nashville Fire Department. References 1. Neumar RW, Otto CW, Link MS, et al. Part 8: Adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3): S729–S767. 2. Sampson K Kass R. Anti-Arrhytmic Drugs: Introduction. 12th. ed. Goodman Gilman’s the Pharmacological Basis of Therapeutics 2011. McGraw-Hill: New York. 3. Kowey P Yan G. Antiarrhythmic Drugs. 13th. ed. Hurst’s the Heart 2011. McGraw-Hill: New York. 4. Gausche M, Persse DE, Sugarman T, et al., Adenosine for the prehospital treatment of paroxysmal supraventricular tachycardia. Ann Emerg Med. 1994;24(2):183–189. 5. Riccardi A, Arboscello E, Ghinatti M, et al. Adenosine in the treatment of supraventricular tachycardia: 5 years of experience (2002-2006). Am J Emerg Med. 2008;26(8):879–882. 6. Burkhart KK. Respiratory failure following adenosine administration. Am J Emerg Med. 1993;11(3):249–250. 7. Christopher M, Key CB, Persse DE. Refractory asystole and death following the prehospital administration of adenosine. Prehosp Emerg Care. 2000;4(2):196–198. 8. Reed R, Falk JL O’Brien J. Untoward reaction to adenosine therapy for supraventricular tachycardia. Am J Emerg Med. 1991;9(6):566–570. 9. Webster DP Daar AA. Prolonged bradyasystole and seizures following IV adenosine for supraventricular tachycardia. Am J Emerg Med. 1993;11(2):192–4. 10. Mallet ML. Proarrhythmic effects of adenosine: A review of the literature. Emerg Med J. 2004;21(4): 408–410. 11. Exner DV, Muzyka T, Gillis AM. Proarrhythmia in patients with the Wolff-Parkinson-White syndrome after standard doses of intravenous adenosine. Ann Int Med. 1995;122(5):351–352. 12. Haynes BE. Two deaths after prehospital use of adenosine. J Emerg Med. 2001;21(2):151–154. 13. Shah CP, Gupta AK, Thakur RK, et al. Adenosine-induced ventricular fibrillation. Indian Heart Journal, 2001;53(2):208–210. 14. Delacretaz E. Clinical practice. Supraventricular tachycardia. New Eng J Med. 2006;354(10):1039–1051. 15. DiMarco JP, Miles W, Akhtar M, et al. Adenosine for paroxysmal supraventricular tachycardia: dose ranging and comparison with verapamil. Assessment in placebo-controlled, multicenter trials. The Adenosine for PSVT Study Group. Ann Int Med. 1990;113(2):104–110. 16. Marill KA, Wolfram S, Desouza IS, et al., Adenosine for wide-complex tachycardia: Efficacy and safety. Crit Care Med. 2009;37(9):2512–2518. 17. Slovis CM, Kundencheck PJ, Wayne MA, et al., Prehospital management of acute tachyarrhythmias. Prehosp Emerg Care. 2003;7(1):2–12. 18. Weismuller P, Kattenbeck K, Heinroth KM, et al. [Terminating supraventricular tachycardia with adenosine--comparing the effectiveness of 12 mg and 18 mg]. Dtsch Med Wochenschr. 2000;125(33):961–969. Read a clinical education article about heart rhythms at www.jems.com/article/monitorsrecorders-vital-signs/rhythm-clues Choose 36 at www.jems.com/rs www.jems.com SEPTEMBER 2012 JEMS 45
