Therapeutic antibodies for autoimmunity and inflammation
- 1. Antibodies have rapidly become a clinically important drug class: more than 25 antibodies are approved for humantherapyandmorethan240antibodiesarecurrently in clinical development worldwide for a wide range of dis- eases, including autoimmunity and inflammation (the focus of this Review), cancer (the focus of the Review by Weiner and colleagues in this issue,REF. 165), organ trans- plantation, cardiovascular disease, infectious diseases and ophthalmological diseases1 . The clinical success of anti- bodies has led to a major commercial impact, with rapidly growing annual sales that exceeded US$27 billion in 2007, including 8 of the 20 top-selling biotechnology drugs2 . This modern era of therapeutic antibodies originated with the invention of hybridoma technology to gener- ate mouse monoclonal antibodies in 1975 (REF. 3). Major limitations of mouse antibodies as therapeutic agents — immunogenicity, lack of effector functions and short serum half-life — were subsequently identified and largely overcome by the advent of antibody chimerization and, later, humanization4 technologies in the mid-1980s. Many antibody drugs, including those for autoimmunity and inflammation (TABLE 1), are chimeric or humanized versions of rodent antibodies. Several approved antibody drugs and an increasing proportion of antibodies entering clinical trials are of human origin5 . These human antibodies are typically derived from large phage display libraries expressing human antibody fragments or transgenic mice engi- neered with human immunoglobulin genes6 . Human antibodies from transgenic mice are commonly devel- oped as therapeutic agents without prior optimization6 . By contrast, phage-derived antibodies may require improvements in binding affinity for antigen or biological potency that are routinely obtained by additional selec- tion for desired phenotypes from phage display librar- ies7 . Evolving technologies, including yeast, ribosome, mRNA, mammalian and Escherichia coli display librar- ies, as well as the direct cloning of human antibodies from human blood or bone marrow-derived cells, might also contribute to future therapeutic antibodies7 . Beyond improved generation and optimization technologies, the development of antibody drugs has benefited from better choices and matching of target, antibody and patients8 , as well as advances in the industrialization of recombinant antibody production and purification processes9 . Current therapeutic antibodies provide much expe- rience to guide future antibody drug development — strengths on which to build, limitations to overcome and new opportunities to seize (BOX 1). The quest for bet- ter therapeutic antibodies has gained great momentum in recent years, motivated by a convergence of clinical, scientific, technological and commercial factors10 . First, there is a strong desire to improve on the clinical benefits for patients that were achieved by first-generation thera- peutic antibodies. Second, there is a growing understand- ing of the mechanisms of action of antibody-based drugs and, in some cases, their limitations, including mecha- nisms of resistance. Third, technological advances are available to optimize and overcome existing biophysical, functional and immunogenic limitations of antibodies, as well as to confer antibodies with new activities10–12 . Fourth, the major commercial success of antibodies2 has fuelled strong competition between companies that will probably intensify as many approved and developing *Department of Immunology, Genentech, Inc.,1 DNA Way, South San Francisco, California 94080, USA. ‡ Department of Antibody Engineering, Genentech, Inc., 1 DNA Way, South San Francisco, California 94080, USA. e-mails: acc@gene.com; pjc@gene.com doi:10.1038/nri2761 Effector functions Fc-mediated antibody properties that are involved in target cell destruction: antibody-dependent cell-mediated cytotoxicity (ADCC), antibody- dependent cellular phagocytosis (ADCP) and complement-dependent cytotoxicity (CDC). Half-life The time taken for the plasma concentration of a drug to fall to half of its original value. Initial half-life and terminal half-life refer to the first (distribution) and second (elimination) phase for bi-exponential pharmacokinetics, respectively. Therapeutic antibodies for autoimmunity and inflammation Andrew C. Chan* and Paul J. Carter‡ Abstract | The development of therapeutic antibodies has evolved over the past decade into a mainstay of therapeutic options for patients with autoimmune and inflammatory diseases. Substantial advances in understanding the biology of human diseases have been made and tremendous benefit to patients has been gained with the first generation of therapeutic antibodies. The lessons learnt from these antibodies have provided the foundation for the discovery and development of future therapeutic antibodies. Here we review how key insights obtained from the development of therapeutic antibodies complemented by newer antibody engineering technologies are delivering a second generation of therapeutic antibodies with promise for greater clinical efficacy and safety. REVIEWS NATURE REviEWS | Immunology volUME 10 | MAy 2010 | 301 focus on THERAPEuTIc AnTIBoDIEs © 20 Macmillan Publishers Limited. All rights reserved 10
- 2. Table 1 | Monoclonal antibodies and Fc fusion proteins for autoimmunity and inflammation* generic name (trade name; sponsoring companies) Format Targets Development stages Diseases Proposed mechanisms of action Natalizumab (Tysabri; Biogen Idec/Elan) Humanized IgG4 α4 subunit of α4β1 and α4β7 integrins Approved MS and Crohn’s disease Receptor binding and antagonism; inhibits leukocyte adhesion to their counter receptor (or receptors) Vedolizumab (MLN2; Millennium Pharmaceuticals/ Takeda) Humanized IgG1 α4β7 integrin Phase III UC and Crohn’s disease Receptor binding and antagonism; inhibits leukocyte adhesion to their counter receptor (or receptors) Belimumab (Benlysta; Human Genome Sciences/ GlaxoSmithKline) Human (phage-produced) IgG1 BAFF Phase III SLE Ligand binding and neutralization Atacicept (TACI–Ig; Merck/Serono) TACI ECD–Fc (IgG1) fusion protein, modified Fc to eliminate effector functions BAFF and APRIL Phase II/III SLE Ligand binding and neutralization; blocks activation of TACI Alefacept (Amevive; Astellas) LFA3 ECD–Fc (IgG1) fusion protein CD2 Approved Plaque psoriasis Inhibits LFA3–CD2 interaction and blocks lymphocyte activation Phase III GVHD Otelixizumab (TRX4; Tolerx/ GlaxoSmithKline) Chimeric light chain, humanized heavy chain, IgG1 aglycosyl Fc CD3 Phase III T1D Modulates T cell function Teplizumab (MGA031; MacroGenics/Eli Lilly) Humanized IgG1with mutated Fc CD3 Phase III T1D Modulates T cell function Rituximab (Rituxan/ Mabthera; Genentech/ Roche/Biogen Idec) Chimeric IgG1 CD20 Approved Non-Hodgkin’s lymphoma, RA (in patients with inadequate responses to TNF blockade) and CLL Sensitizes cells to chemotherapy; induces apoptosis, ADCC and CDC Ofatumumab (Arzerra; Genmab/ GlaxoSmithKline) Human (mouse-produced) IgG1 CD20 Approved CLL CDC and ADCC Phase III RA Ocrelizumab (2H7; Genentech/Roche/ Biogen Idec) Humanized IgG1 CD20 Phase III RA and SLE ADCC and CDC Epratuzumab (hLL2; Immunomedics/UCB) Humanized IgG1 CD22 Phase III SLE and non-Hodgkin’s lymphoma ADCC and downregulation of B cell receptor Alemtuzumab (Campath/ MabCampath; Genzyme/Bayer) Humanized IgG1 CD52 Approved CLL ADCC Phase III MS Abatacept (Orencia; Bristol-Myers Squibb) CTLA4 ECD–Fc, mutated IgG1 Fc CD80 and CD86 Approved RA and JIA Inhibits T cell activation by binding to CD80 and CD86, thereby blocking interaction with CD28 Phase III UC and Crohn’s disease Phase II/III SLE Eculizumab (Soliris; Alexion pharmaceuticals) Humanized IgG2 and IgG4 C5 complement protein Approved Paroxysmal nocturnal haemoglobinuria Binds C5, inhibiting its cleavage to C5a and C5b and preventing the generation of the terminal membrane attack complex C5b–C9 Omalizumab (Xolair; Genentech/Roche/ Novartis) Humanized IgG1 IgE Approved Moderate to severe persistent allergic asthma Ligand binding and receptor antagonism, reduces release of allergic response mediators from mast cells and basophils Canakinumab (Ilaris; Novartis) Human (mice) IgG1 IL-1β Approved Cryopyrin-associated periodic syndromes Ligand binding and receptor antagonism Phase III SystemicJIA,neonatal- onsetmultisystem inflammatorydisease andacutegout REVIEWs 302 | MAy 2010 | volUME 10 www.nature.com/reviews/immunol REVIEWs © 20 Macmillan Publishers Limited. All rights reserved 10
- 3. Phage display Technology for displaying a protein, such as an antibody fragment, on the surface of a bacteriophage that contains the gene (or genes) encoding the displayed protein (or proteins), thereby physically linking the genotype and phenotype. Binding affinity For two interacting molecules this is the ratio of their association (ka ) and dissociation (kd ) rate constants: Kd = kd ÷ka . drugs target the same antigen and/or diseases. Together, these major factors of target biology modulated by anti- body properties can greatly affect the degree of clinical efficacy achieved and the ultimate successful adoption and use of a drug. The main functions of igG are determined by their interaction with four classes of naturally occurring binding partners: antigen, Fc receptors for igG (FcγRs), complement and the neonatal FcR (FcRn) (FIG. 1). Highly selective antigen binding is a signature and functionally crucial property of antibodies that is mediated by their variable domains. Several igG functions are dependent on interaction of the Fc region with other proteins: FcγRs for antibody-dependent cell-mediated cytotoxicity (ADCC) and antibody-dependent cellular phagocytosis (ADCP), complement components for complement-dependent cytotoxicity (CDC) and FcRn for long serum persist- ence. Here, we first discuss the diverse mechanisms by which therapeutic antibodies modulate the functions of their target antigens to affect their biological behaviours and therapeutic profile. These include binding of soluble cytokines and growth factors, receptor blockade, cellular depletion through ADCC, ADCP, CDC and induction of apoptosis, receptor modulation and/or receptor signal- ling. Thereafter, we discuss the strategies that are being applied to create the next generation of antibody drugs. Mechanisms of therapeutic antibody action Cytokine and growth factor blockade. The first thera- peutic antibody for the treatment of inflammatory diseases was infliximab (Remicade; Centocor/Merck), in 1998, for the treatment of Crohn’s disease. infliximab, Table 1 (cont.) | Monoclonal antibodies and Fc fusion proteins for autoimmunity and inflammation* generic name (trade name; sponsoring companies) Format Targets Development stages Diseases Proposed mechanisms of action Mepolizumab (Bosatria; GlaxoSmithKline) Humanized IgG1 IL-5 Phase III Hyper-eosinophilic syndrome Ligand binding and receptor antagonism Reslizumab (SCH55700; Ception Therapeutics) Humanized IgG4 IL-5 Phase III Eosinophilic oesophagitis Ligand binding and receptor antagonism Tocilizumab (Actemra/ RoActemra; Chugai/ Roche) Humanized IgG1 IL-6R Approved RA Receptor binding and ligand blockade Phase III JIA Ustekinumab (Stelara; Centocor) Human (mice) IgG1 IL-12 and IL-23 Approved Plaque psoriasis Ligand binding and receptor antagonism Phase III Psoriatic arthritis Phase II/III Crohn’s disease Briakinumab (ABT-874; Abbott) Human (phage-produced) IgG1 IL-12 and IL-23 Phase III Psoriasis and plaque psoriasis Ligand binding and receptor antagonism Etanercept (Enbrel; Amgen/Pfizer) TNFR2 ECD–Fc (IgG1) fusion protein TNF Approved RA, JIA, psoriatic arthritis, AS and plaque psoriasis Neutralizes TNF activity by binding soluble and transmembrane TNF and inhibiting binding to TNFRs Infliximab (Remicade; Centocor/Merck) Chimeric IgG1 TNF Approved Crohn’s disease, RA, psoriatic arthritis, UC, AS and plaque psoriasis Neutralizes TNF activity by binding soluble and transmembrane TNF and inhibiting binding to TNFRs; induction of activated T cell and macrophage apoptosis Adalimumab (Humira/ Trudexa; Abbott) Human (phage-produced) IgG1 TNF Approved RA, JIA, psoriatic arthritis, Crohn’s disease, AS and plaque psoriasis Neutralizes TNF activity by binding soluble and transmembrane TNF and inhibiting binding to TNFRs; lyses TNF-expressing cells by CDC; induction of activated T cell and macrophage apoptosis Certolizumab pegol (Cimzia; UCB) Humanized Fab, PEG conjugate TNF Approved Crohn’s disease and RA Neutralizes TNF activity by binding soluble and transmembrane and inhibiting binding to TNFRs Golimumab (Simponi; Centocor) Human (mouse-produced) IgG1 TNF Approved RA, psoriatic arthritis and AS Neutralizes TNF activity by binding soluble and transmembrane TNF and inhibiting binding to TNFRs ADCC, antibody-dependent cellular cytotoxicity; APRIL, a proliferation-inducing ligand; AS, ankylosing spondylitis; BAFF, B cell activating factor; CDC, complement- dependent cytotoxicity; CLL, chronic lymphocytic leukaemia; CTLA4, cytotoxic T lymphocyte antigen 4; ECD, extracellular domain; GVHD, graft-versus-host disease; IL, interleukin; JIA, juvenile idiopathic arthritis; LFA3, lymphocyte function-associated antigen 3; MS, multiple sclerosis; PEG, polyethylene glycol; R, receptor; RA, rheumatoid arthritis; TACI, transmembrane activator and calcium-modulating cyclophilin ligand interactor; SLE, systemic lupus erythematosus; T1D, type 1 diabetes; TNF, tumour necrosis factor; UC, ulcerative colitis. *Data sources include drug prescribing information, www.ClinicalTrials.gov, REF.1, REF. 163 and company web sites. Antibodies and Fc fusion proteins that have reached at least Phase II or III clinical trials are included, many are in less advanced stages for additional indications. The αL integrin-specific antibody efalizumab (Raptiva/Xanelim; Genentech/Roche/Merck–Serono) was voluntarily withdrawn from the market by its manufacturers in April 2009 because of its association with an increased risk of progressive multifocal leukoencephalopathy, a rare and usually fatal disease of the central nervous system. REVIEWs NATURE REviEWS | Immunology volUME 10 | MAy 2010 | 303 focus on THERAPEuTIc AnTIBoDIEs © 20 Macmillan Publishers Limited. All rights reserved 10
- 4. Neonatal FcR (FcRn). An Fc receptor that is structually related to MHC class I molecules and protects IgG from degradation, resulting in long serum half-life. Additionally, FcRn mediates IgG transfer from a mother to her fetus, thereby providing passive immunity. Immunoadhesin A fusion protein that combines the functional domain of a binding protein, such as a receptor or ligand, with an immunoglobulin Fc domain. Such Fc fusion proteins can endow binding proteins with antibody-like properties including long serum half-life and effector functions. a chimeric antibody with mouse variable domains and human constant domains, binds both soluble and membrane-associated tumour necrosis factor (TNF)13 . over the past 12 years, four additional TNF antagonists have been approved by the US Food and Drug Administration (FDA) for human use, each with distinguishing features14 . These include etanercept (Enbrel; Amgen/Pfizer), a TNF receptor ii (TNFRii) immunoadhesin fused to the Fc domains of human igG1 that neutralizes both TNF and lymphotoxin-α (also known as TNFβ); adalimumab (Humira/Trudexa; Abbott), a fully human igG1κ antibody derived from phage display technology that inhibits TNF; certolizu- mab pegol (Cimzia; UCB), a humanized Fabʹ frag- ment, chemically conjugated to polyethylene glycol (PEGylated), that neutralizes both membrane-associated and soluble human TNF; and golimumab (Simponi; Centocor), a fully human igG1κ TNF-specific antibody created using genetically engineered mice (FIG. 2). The TNF antagonists are presently the most successful class of biological drug for inflammatory diseases, with total worldwide sales of $16.4 billion in 2008, and they are approved not only for the treatment of Crohn’s disease but also for the treatment of rheumatoid arthritis, juve- nile rheumatoid arthritis, psoriatic arthritis, ulcerative colitis, ankylosing spondylitis and plaque psoriasis (see http://www.pipelinereview.com). These five TNF antag- onists show the evolution of antibody technologies over the past two decades, beginning with the initial chal- lenges of producing industrial quantities of the chimeric antibody infliximab and the immunoadhesin etanercept followed by the introduction of humanization proto- cols, phage display technologies, use of genetically modified mice expressing human immunoglobulins and application of PEGylation to increase the half-life of antibody fragments. Box 1 | Strengths, limitations and future opportunities of therapeutic antibodies Strengths • The availability of several well-established and broadly applicable methods for antibody generation and optimization. • A growing repertoire of technologies to redesign antibodies with modified or new properties to enhance their clinical potential; for example, pharmacokinetic properties such as terminal half-life can be tuned from minutes up to several weeks10–12 . • A high success rate compared to other drugs: 17% for humanized antibodies from the first human trial to regulatory approval5 . • Well-established and broadly applicable production technologies9 . • Often, but not invariably, well tolerated by patients. • Broad experience and expanding knowledge of antibody drug development facilitates the generation of future therapeutic antibodies. limitations • Expensive, reflecting high production costs and commonly large doses9 , potentially limiting patient access or clinical applications. • Clinical applications currently limited to cell surface or extracellular targets. • Cannot be orally administered. • The large size, particularly of the IgG format (~150 kDa), may limit tissue penetration. • There is limited penetration of the central nervous system by IgG owing to inefficient penetration of the blood–brain barrier. Future opportunities • Greater efficacy. • Higher affinity or potency. • Enhanced effector functions — antibody-dependent cell-mediated cytotoxicity (ADCC), antibody-dependent cellular phagocytosis (ADCP), complement-dependent cytotoxicity (CDC). • Target multiple disease mediators from distinct signalling pathways or that have redundant roles in the same pathway using bispecific antibodies. • Greater safety. • Reduced effector functions. • More ready reversibility of antibody action; for example, shorter half-life. • Greater selectivity for target. • Avoid activation of the target. • Improved delivery. • Lower or less frequent dosing using antibodies that are more potent or have a longer serum half-life. • Increased bioavailability. • Ability to cross the blood–brain barrier to reach the central nervous system. • More facile ocular delivery, including sustained release, ocular penetration and half-life. • Oral delivery. REVIEWs 304 | MAy 2010 | volUME 10 www.nature.com/reviews/immunol REVIEWs © 20 Macmillan Publishers Limited. All rights reserved 10
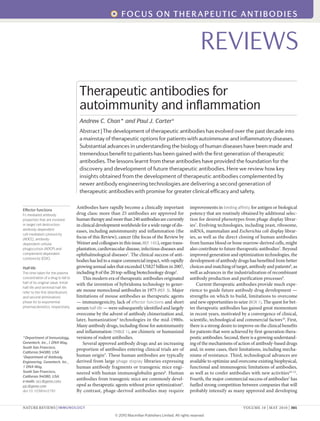
- 5. Nature Reviews | Immunology FcγR FcRn IgG binding partner Protein strategies for modifying interactions Potential impact of modifying interaction Antigen Mutate V domain sequences using display libraries and/or rationale design Mutate Fc sequence using display libraries and/or rationale design; select IgG isotype Mutate Fc sequence using display libraries and/or rationale design Antibody fragment lacking Fc Glycosylation strategies for modifying FcγR and complement interactions Aglycosylation Non-fucosylation Bisecting N-acetylglucosamine ↑ or ↓ ADCC ↑ or ↓ ADCP ↑ or ↓ CDC ↑ ADCC ↑ ADCC ↑ or ↓ half-life ↓ Half-life, ↓ CDC, ↓ ADCC and ↓ ADCP ↓ ADCC, ↓ ADCP and ↓ CDC Altered binding affinity or specificity VL CL VH CH1 CH2 CH3 Fc region Fab Bisecting N-acetylglucosamine N-acetylglucosamine Galactose Sialic acid Fucose Asn297 Mannose Core Variable Glycosylation Complement Human anti-chimeric antibodies (HACAs). The immune system can develop an antibody response to chimeric antibodies. Binding of HACAs to chimeric antibodies forms immune complexes that can shorten the half-life of the therapeutic antibodies and compromise clinical effectiveness. Additionally these immune complexes can deposit in organs such as skin and kidney causing adverse events, including rashes and glomerulonephritis. Human anti-human antibodies (HAHAs). The immune system can also develop an immune response to human therapeutic antibodies. HAHAs tend to be less common and less severe than HACAs. Evolution of these technologies partially solved one of the historic obstacles of antibodies — immunogenic- ity. Patients with Crohn’s disease treated with inflixi- mab develop human anti-chimeric antibodies (HACAs) in 8–61% of patients15,16 . These HACAs can bind to the therapeutic antibody limiting its half-life and clinical effectiveness, as well as causing infusion-related ana- phylaxis in some patients15,17 . The incidence of HACA development can be attenuated by co-administration of immunosuppressive agents in patients with Crohn’s disease or with rheumatoid arthritis15,18 . The advent of humanization protocols and develop- ment of human antibodies have minimized this immuno- genicity. However, patients treated with humanized or human antibodies still develop human anti-human antibodies (HAHAs). Adalimumab, a phage-derived human antibody, has an incidence of 12% neutralizing HAHAs in patients with rheumatoid arthritis receiving monotherapy that is decreased to ~1% in patients also treated with the immunosuppressant methotrexate19 . in a prospective observational cohort of 121 patients with rheumatoid arthritis treated with adalimumab, HAHAs were detected in 34% of non-responders compared with 5% of responders20 . Similarly, 6.3% of patients with early onset rheumatoid arthritis treated with golimumab, a human antibody derived from mice expressing human immunoglobulin genes, developed neutralizing HAHAs with the incidence of HAHAs higher in non-methotrexate-treated (13.5%) than methotrexate-treated patients (1.9–3.7%)21 . Figure 1 | Engineering Igg structure and function. IgGs are ~150 kDa tetramers comprising pairs of identical heavy and light chains linked by disulphide bonds (yellow bars). The heavy chains contain a variable domain, VH , and three constant domains, CH 1, CH 2 and CH 3, whereas the light chains contain a variable domain, VL , linked to a single constant domain, CL . A signature property of antibodies is highly selective antigen binding mediated by their variable domains. Human IgG, particularly IgG1 and IgG3, bound to an antigen on a target cell surface can interact with Fc receptors for IgG (FcγRs) on effector cells and may support the destruction of target cells by antibody-dependent cell-mediated cytotoxicity (ADCC) or antibody-dependent cellular phagocytosis (ADCP), whereas interaction with the complement component C1q may support killing by complement-dependent cytotoxicity (CDC). IgG antibodies, like other circulating proteins, are taken up by vascular endothelial cells and other cells by pinocytosis. Subsequently, IgG can interact with the salvage receptor, neonatal FcR (FcRn), in a pH-dependent manner with binding occurring in endosomes at pH 6.0–6.5, followed by recycling and release at the cell surface at pH 7.0–7.4. Fc interaction with FcRn is mainly responsible for the long serum half-life of IgG108 . Engineering of IgG variable domain sequences provides the means to tailor their antigen-binding affinity or specificity10 . Fc amino acid sequence modification allows modulation of effector functions (ADCC, ADCP and CDC) and/or half-life10–12,71 . Effector functions can be also be tuned by modifying Fc glycosylation. For example, mutating the conserved aspargine, Asn297, prevents glycosylation to generate aglycosylated antibodies lacking effector functions. ADCC can be enhanced by increasing the bisecting N-acetylglucosamine in the Fc carbohydrate or by eliminating fucose11 . This figure is modified from Nature Reviews Immunology REF. 10. REVIEWs NATURE REviEWS | Immunology volUME 10 | MAy 2010 | 305 focus on THERAPEuTIc AnTIBoDIEs © 20 Macmillan Publishers Limited. All rights reserved 10
- 6. IL-6 Nature Reviews | Immunology TNF TNF Ligand blockade Receptor blockade Receptor downregulation Depletion Signalling induction Infliximab* Adalimumab* Golimumab Certolizumab pegol Canakinumab Briakinumab Ustekinumab Omalizumab* Tocilizumab Efalizumab* Natalizumab Vedolizumab Abatacept‡ Efalizumab* Omalizumab* Otelixizumab* Teplizumab* Epratuzumab* Otelixizumab* Teplizumab* Muromonab* GA101* Infliximab* Adalimumab* Rituximab* Rituximab* Ofatumumab Ocrelizumab GA101* Alemtuzumab Muromonab* Epratuzumab* IL-6R Soluble IL-6R TNFRI TNFRI Therapeutic antibody Fab fragment gp130 gp130 CD20 TCR–CD3 complex αLβ2 integrin Immunoadhesin Therapeutic antibody FcγR MAC Lysis Complement components Effector cell Belimumab Eculizumab Mepolizumab Reslizumab Etanercept‡ Atacicept‡ Alefacept‡ Half-lives of each of the TNF-specific antibodies also define dosing schedules and modes of delivery. infliximab has the shortest half-life (~8–10 days) among the TNF-specific antibodies and is administered intra- venously every 4–8 weeks. By contrast, adalimumab and golimumab, both with half-lives of ~2 weeks, are admin- istered subcutaneously every 2–4 weeks, respectively. Subcutaneous administration is more convenient for patients, particularly those with chronic diseases requir- ing long-term therapy, as intravenous administration requires visits to physicians’ offices or infusion centres. Finally, the different formats of TNF-specific anti- bodies have also revealed some interesting aspects con- cerning the therapeutic mechanism (or mechanisms) of efficacy. A proposed mechanism by which inflixi- mab, and not etanercept, was thought to be efficacious in Crohn’s disease was the ability of infliximab to bind membrane-associated TNF and induce apoptosis of acti- vated T cells and macrophages22–24 . However, the thera- peutic success of certolizumab pegol and the preliminary clinical efficacy of golimumab in Crohn’s disease, agents that do not induce apoptosis of activated T cells or mac- rophages, suggest that other mechanisms probably con- tribute to the efficacy of TNF-specific agents in Crohn’s disease14,25–27 . The lessons learnt from the development of TNF- neutralizing therapeutic agents are rapidly being applied to other classes of therapeutic antibodies. Canakinumab (ilaris; Novartis), an interleukin-1β (il-1β)-specific anti- body approved for the treatment of cryopyrin-associ- ated periodic syndrome (CAPS), builds on the clinical experience of anakinra (Kineret; Amgen/Biovitrum), a recombinant non-glycosylated form of the human il-1 receptor antagonist (il-1Ra) approved for the treatment of rheumatoid arthritis28,29 . The long half-life of cana- kinumab (~26 days) allows subcutaneous dosing every 8 weeks for children with CAPS. By contrast, anakinra has a half-life of only 4 to 6 hours, necessitating daily subcutaneous injections for patients with rheumatoid arthritis. Ustekinumab (Stelara; Centocor), a human igG1κ antibody that binds the p40 subunits of il-12 and il-23, which has been approved for the treatment of moderate to severe plaque psoriasis, has a median half- life of ~21.6 days30,31 . Administration of ustekinumab to patients with psoriasis requires only quarterly sub- cutaneous injections following an initial loading dose. interestingly, more frequent dosing seems to be required for patients with Crohn’s disease and may reflect differ- ences in the biology of il-12 and il-23 in these two immunologically and genetically related diseases32 . Receptor blockade and receptor modulation. in addi- tion to ligand blockade, therapeutic antibodies can also block ligand–receptor interactions by targeting the receptor (FIG. 2). These include antibodies that target the il-6 receptor (tocilizumab (Actemra/RoActemra; Chugai/Roche)), αl integrin (also known as CD11a and lFA1) (efalizumab (Raptiva/Xanelim; Genentech/ Roche/Merck–Serono)), the α4 subunit of α4β1 and α4β7 integrins (natalizumab (Tysabri; Biogenidec/Elan)) and α4β7 integrin (vedolizumab (MlN2; Millennium Figure 2 | mechanisms of action of therapeutic antibodies. Five non-overlapping mechanisms of action are depicted. Examples of therapeutic antibodies are listed for each mechanism of action depicted. Ligand blockade with full length IgG therapeutic antibodies (for example, infliximab, adalimumab or golimumab), antibody fragments (forexample, certolizumab pegol) or receptor immunoadhesins (for example, etanercept and those indicated with ‡ ) can prevent ligands from activating their cognate receptors. Binding of ligands (for example, interleukin-6 (IL-6)) to receptors (for example, IL-6R) can also be blocked by antibodies directed to their cognate receptors and inhibit receptor activation or function. Binding of cell surface receptors by antibodies can also result in their internalization and downregulation to limit cell surface receptors that can be activated by the ligand. Note that binding of cell surface receptors by antibodies (for example, αL integrin by efalizumab) or binding of a ligand (for example, free serum IgE by omalizumab) can indirectly also result in downregulation of cell surface receptors available for cellular activation. Binding of cell surface receptors can result in depletion of antigen-bearing cells through complement-mediated lysis and opsonization, as well as Fc receptor for IgG (FcγR)-mediated clearance. Therapeutic antibodies can also induce active signals that alter cellular fates. Binding of the T cell receptor (TCR)–CD3 complex by teplizumab can induce TCR-mediated signals and alter T cell functions and differentiation. MAC, membrane attack complex; TNF, tumour necrosis factor; TNFRI; TNF receptor I. *Antibodies with several mechanisms of action. REVIEWs 306 | MAy 2010 | volUME 10 www.nature.com/reviews/immunol REVIEWs © 20 Macmillan Publishers Limited. All rights reserved 10
- 7. Pharmaceuticals/Takeda)). Targeting of receptors adds a secondary level of mechanistic activity as a subset of these therapeutic antibodies not only blocks ligand binding but also downregulates the cell surface expression of the tar- geted receptors. However, this antibody-induced inter- nalization of the target also results in antigen-induced clearance of the therapeutic antibody and decreases its serum half-life. For example, efalizumab not only binds αl integrin to block interactions between αl integrin and intercellular adhesion molecule 1 (iCAM1) but also downregulates αl integrin expression by T cells, a crucial co-receptor for T cell activation, as well as the expression of other T cell co-stimulatory molecules. Hence, efalizu- mab interferes with both T cell homing by interrupting αl integrin–iCAM1 interactions and T cell activation by downregulating co-stimulatory molecule expression33 . Downmodulation of cell surface receptor expression can also be achieved indirectly through ligand target- ing. omalizumab (Xolair; Genentech/Roche/Novartis), which is approved for the treatment of moderate and severe allergic asthma, binds and prevents the secreted form of igE from occupying the high affinity receptor for igE (FcεRi) on mast cells and basophils34 . Whereas binding sequesters allergic igE from allergen-mediated activation of mast cells and basophils, the unoccupied surface FcεRi undergoes internalization and results in a decrease in cell surface FcεRi expression on dendritic cells, mast cells and basophils35–37 . Hence, binding of igE by omalizumab probably operates through two distinct mechanisms: sequestration of the allergic igE and indi- rect downregulation of cell surface FcεRs on mast cells and basophils38 . Receptor downregulation might serve as the basis for the efficacy of omalizumab in the treat- ment of chronic idiopathic urticaria and angioedema (CiU)39–41 . Approximately 40% of patients with CiU have autoantibodies that recognize and can crosslink the FcεRi α-subunit, triggering mast cell and basophil activation42,43 . Downregulation of cell surface FcεRs by omalizumab in these patients may attenuate the ability of these autoantibodies to activate mast cells and basophils to provide clinical improvement. A theoretical concern for targeting cell surface recep- tors, as opposed to their corresponding soluble ligands, is a greater potential for inducing an immunogenic response. Therapeutic antibodies that induce antigen- dependent internalization through the endocytic path- way can theoretically be processed as foreign antigens and presented on MHC class ii molecules to initiate a CD4+ T cell-dependent humoral response. However, although this is possible, we are not aware of any data that support this target class differential in immuno- genicity of therapeutic antibodies. ongoing develop- ment of therapeutic antibodies that target dendritic cell surface antigens (such as DEC205; also known as ly75) may be informative in this regard. Depleting and signalling antibodies. Another class of therapeutic antibodies binds to cell surface antigens — for example, CD20, CD22 and CD52 — and depletes antigen-bearingcells(FIG. 2).Rituximab(Rituxan/Mabthera; Genentech/Roche/Biogen idec) and alemtuzumab (Campath/MabCampath; Genzyme/Bayer), approved first for the treatment of cancer, were subsequently tested in autoimmune and inflammatory conditions. Rituximab, a chimeric CD20-specific antibody, was approved in 2005forthetreatmentofpatientswithrheumatoidarthritis who had inadequate responses to TNF blockade44 ; rituxi- mab and alemtuzumab (a humanized CD52-specific anti- body)haveshownclinicalactivityinPhaseiiclinicaltrials of the relapsing–remitting form of multiple sclerosis45,46 . ocrelizumab (2H7; Genentech/Roche/Biogen idec), which is a humanized CD20-specific antibody, is being studiedinPhaseiiiclinicaltrialsofrheumatoidarthritis47 , and epratuzumab (hll2; immunomedics/UCB), which is a humanized CD22-specific antibody, is being studied in Phase iii clinical trials of systemic lupus erythemato- sus48 . This class of therapeutic antibodies operates mainly through FcγR-mediated clearance of antigen-bearing cells; although CDC can also contribute to their thera- peutic effect under certain circumstances49–52 . Patients with non-Hodgkin’s lymphoma treated with rituximab have better prognosis if they express the FcγRiiiA val158 encoding allele, which has high affinity for igG1, than patients expressing the FcγRiiiA Phe158 encoding allele, which has lower affinity for igG1(REFS 53,54). Similarly, in a small study of patients with SlE treated with rituximab, B cell depletion was superior in patients with FcγRiiiA val158 than those with FcγRiiiA Phe158 (REF. 55). Hence, FcγR-mediated functions have an important role for this class of therapeutic antibody and offer an opportunity to design more efficacious therapies. in addition to effector functions, the nature of the antigen also contributes to the depleting potential of a therapeutic antibody. Although antibodies such as efal- izumab and natalizumab bind to αl and α4 integrins expressed by T cells, these antibodies do not deplete T cells. Many antigen-related factors, including cell sur- face density, probably contribute to the depleting poten- tial of a therapeutic antibody. CD20 is highly expressed (~90,000 molecules) on normal B cells, but its expres- sion level is highly variable in B cell malignancies56,57 . lower levels of CD20 expression can inhibit the ability of CD20-specific antibodies to mediate CDC58 . in addition, expression of complement regulatory proteins (such as CD59, CD46 and CD55) on the target cell can com- promise complement-mediated killing of target cells59 ; however, the expression of these complement regula- tory proteins does not predict clinical outcome follow- ing rituximab treatment in patients with non-Hodgkin’s lymphoma60 . Finally, antibody-mediated internalization can also decrease the number of accessible cell surface antibody–antigen complexes to affect both CDC- and ADCC-mediated depletion of target cells. These mecha- nistic data provide clues for the generation of future ther- apeutic antibodies with improved effector function. Astheclearanceofcellsismediated,inpart,bymobili- zation of cells from organs into the blood and clearance of antibody-bound targets by myeloid-derived cells (such as Kupffer cells in the liver), non-circulating antigen-bear- ing cells saturated with the therapeutic antibody seem to be more resistant to antibody-mediated clearance50 . Biopsies of the synovium of patients with rheumatoid REVIEWs NATURE REviEWS | Immunology volUME 10 | MAy 2010 | 307 focus on THERAPEuTIc AnTIBoDIEs © 20 Macmillan Publishers Limited. All rights reserved 10
- 8. Bispecific antibodies Antibodies capable of binding to two different antigens or two distinct epitiopes on the same antigen are known as bispecific. arthritis following treatment with rituximab contain residual CD20-bearing B cells61,62 . in FvB mice, marginal zone B cells in the spleen are not completely depleted by CD20-specific antibody therapy50 . However, these mar- ginal zone B cells are not intrinsically resistant to CD20- specific antibody killing as forced mobilization of these cells into the blood with blockade of αl integrin and α4 integrin renders them sensitive to depletion mediated by CD20-specific antibody. Hence, strategies to mobilize cells from their microenvironments may enhance the depleting potential of therapeutic antibodies. Therapeutic antibodies that bind cell surface anti- gens can also transmit intracellular signals required for clinical efficacy and/or contribute to adverse events63 . The mouse CD3-specific antibody muromonab-CD3 (oKT3; Janssen-Cilag), the first FDA-approved thera- peutic antibody for the treatment of acute allograft rejection in renal transplantation64 , crosslinks the T cell receptor (TCR)–CD3 complex to induce transient cytokine release, resulting in an acute and severe flu-like syndrome and T cell depletion64 . Muromonab-CD3 has an additional limitation in that ~50% of patients develop neutralizing antibodies that diminish its therapeutic effect65 . The beneficial activities of muromonab-CD3 are mediated by its variable domains, whereas the undesir- able mitogenic activity — stimulation of T cell prolif- eration and cytokine production — requires interaction between the muromonab-CD3 Fc region and FcγRs66 . A second generation of CD3-specific antibodies (teplizumab (MGA031; MacroGenics/Eli lilly) and otelixizumab (TRX4; Tolerx/GlaxoSmithKline)) that are under evaluation for the treatment of type 1 diabetes are humanized antibodies with mutations that impair inter- action with FcγRs (FIG. 2). These non-mitogenic antibod- ies do not induce the same degree of T cell activation and adverse events as observed with muromonab-CD3. However, both these antibodies still activate T cells, althoughtheirmechanisticeffectsarecomplex.First,these antibodies seem to downregulate the level of cell surface TCR–CD3 complexes. Although the TCR–CD3 complex is continually internalized and recycled, internalization of even unbound TCR–CD3 increases ~10-fold in the presence of otelixizumab without change in the exocytic rate67 . Second, in vitro crosslinking of T cells with teplizu- mab induces TCR-mediated increases in free cytoplasmic Ca2+ andanalteredpatternofcytokineproductionfavour- ing il-10 rather than interferon-γ expression68 . Patients treated with teplizumab developed increased numbers of il-10-producing CD4+ T cells and an even greater expan- sion of CD8+ CD25+ CTlA4+ FoXP3+ regulatory T cells69 . Hence, this class of antibody seems to modulate T cell function by altering T cells from an activating phenotype to potentially a tolerizing or regulatory phenotype. Next-generation therapeutic antibodies Strategies for new antibody generation can be broadly classified as modification of existing antibody properties or the endowment of antibodies with new capabilities (FIG. 1). Here we discuss examples of these two distinct categories — modulation of Fc-mediated functions and the generation of bispecific antibodies (FIG. 3) for dual disease mediator blockade — that seem particularly promising for the generation of antibody drugs for autoimmunity and inflammation. We focus on igG as the format most widely adopted for therapeutic antibodies. Antibody fragments are also discussed as they are widely used in engineering antibody properties, they provide the building blocks to construct many new formats (including bispecific antibodies) and they are becoming important therapeutic agents in their own right70 . Optimization of Fc-mediated antibody functions. Modification of Fc-mediated activities is emerging as one of the most promising ways to further increase the clinical potential of antibodies10–12 . Modulation of effec- tor functions (ADCC, ADCP and CDC) and pharmaco- kinetic half-life are reviewed here in the context of antibody development for autoimmunity and inflam- mation. Engineering igG–binding partner interactions is routinely accomplished through amino acid sequence alterations in the antibody identified by selection from display libraries of antibody fragments and/or structure- guided design. Tailoring Fc glycosylation offers a pow- erful additional method to modify some igG functions, particularly enhancement of ADCC11 . Fc binding to anotherligand,namelyproteinA,isubiquitouslyexploited for chromatographic purification of antibodies, including for therapeutic use9 . Effector function minimization. For some antibody therapies, antigen binding may be sufficient for achiev- ing efficacy, and effector functions may be unnecessary and a potential source of adverse events in patients. Moreover, monovalent target binding may be necessary to avoid unwanted activation of the target. Several dif- ferent strategies are available to generate antibodies that have minimal or no effector functions and, if need be, that are also non-activating71 . indeed many antibody drugs are designed with minimal effector functions, as exemplified below with antibodies that have reached Phase iii clinical trials or beyond in autoimmunity and inflammatory diseases (TABLE 1). As discussed previously, the clinical potential of CD3-specific antibodies has been greatly improved by Fc engineering to attenuate FcγR interactions and over- come mitogenic activity and the development of a flu-like syndrome, in conjunction with humanization to reduce immunogenicity. indeed, two such humanized CD3- specific antibodies — teplizumab and otelixizumab — have advanced to Phase iii clinical trials (TABLE 1). These CD3-specific antibodies use different means to mini- mize FcγR binding: igG1 isotype with leu234Ala and leu235Alamutationsforteplizumab72,73 andaglycosylated igG1 with an Asn297Ala mutation for otelixizumab74 . The igG4 isotype has also been selected for a few therapeutic antibodies for which effector functions are not desired75 , including natalizumab and reslizumab (SCH55700; Ception Therapeutics) (TABLE 1). igG4 molecules are prone to exchange Fabʹ arms in vivo to become functionally monovalent76 . However, this seem- ingly undesirable attribute of igG4 for antibody drugs can be readily prevented by mutation of the hinge REVIEWs 308 | MAy 2010 | volUME 10 www.nature.com/reviews/immunol REVIEWs © 20 Macmillan Publishers Limited. All rights reserved 10
- 9. Nature Reviews | Immunology a Antigen-binding building blocks b Bispecific antibody fragments c IgG-based bispecific antibodies VL VL Fv scFv Diabody Diabody scDiabody–Fc scDiabody–CH3 scDiabody IgG–scFv scFv–IgG VH VH VL VH VL VL VH VH VL VH VL VH VL VH VL VH Antigen 1 Two variable domain binding sites Single variable domain binding sites Antigen 2 Tandem scFv F(ab′)2 Hybrid hybridoma Two-in-one IgG (Fab′scFv)2 Fab–scFv Tandem scFv–Fc scFv–Fc knobs-into-holes Knobs-into-holes with common light chain scFv–Fc–scFv Dual V domain IgG VL CL VH CH1 VL VH IgG–V V–IgG Figure 3 | modular Igg architecture supports numerous bispecific antibody formats. a|Fvfragments,comprisinga VL andVH domainpair,arethemostcommonantigen-binding buildingblockinIgG.Fvfragmentsareroutinelyengineered intoasingle-chain(sc)formatusingashortpeptidelinker(~15 residues)toconnectvariabledomainsineitherVH –VL orVL –VH topology156,157 .ConstructionofscFvfragmentswithshorter linkers(typically1–10residues)allowsinter-chain,butnot intra-chain,domainpairingtoformadimer—thediabody158 . Singlevariabledomainantigen-bindingsitesarefoundinsome IgGmoleculesfromcamelidsandcertainsharkspecies,andthis formatisnowbeingusedforconstructingtherapeutics159 . b|Antigen-bindingbuildingblocks,particularlyscFvand diabodies,havebeenextensivelypermutatedwithother antibodydomainsandproteindomains(notshown)tocreate anincreasingrepertoireofalternativebispecificantibody fragmentformats.Fcregionsareincludedincasesinwhich specificeffectorfunctionsand/orlongserumhalf-lifeare desired.Bycontrast,CH 3domainshavebeenusedfor dimerizationincasesinwhichFc-mediatedfunctionsarenot needed. c|Hybridhybridomatechnologiesprovidedthefirst directroutetobispecificIgGbyco-expressionoftwodifferent IgGspecificities160 ,albeitcommonlywithlowyieldandpurity as,beyondthedesiredbispecificIgG,co-expressionoftwo differentantibodyheavyandlightchainscangiverisetoupto nineunwantedantibodymolecules(notshown)161 .Efficient constructionofbispecifichumanIgGwasachievedusing phage-derivedantibodieswithacommonlightchain,to circumventlightchainmispairing,andknobs-into-holes engineering,todirecttheassemblyoftwodifferentheavy chains162 .Phagedisplaytechnologyhasendoweda monospecificantibodywiththeabilitytobindasecond antigenwhilemaintaininghighaffinityforthefirstantigen— ‘two-in-one’IgG141 .Thebindingsitesarepartiallyoverlapping sotheycanbindonlyoneantigenatatime.Severalbispecific antibodyformatsarebothbispecificandbivalentforeach antigen.Forexample,thedualvariabledomainIgGformatwas createdbyappendingVL andVH domainswithsimilardomains ofasecondantigen-bindingspecificity147,148 .Bispecific antibodieshavealsobeengeneratedbyappendingeitherthe aminoorcarboxylterminusofanIgGheavyorlightchainwitha scFvorsinglevariable(V)domainofasecondbindingspecificity. REVIEWs NATURE REviEWS | Immunology volUME 10 | MAy 2010 | 309 focus on THERAPEuTIc AnTIBoDIEs © 20 Macmillan Publishers Limited. All rights reserved 10
- 10. sequence (Cys-Pro-Ser-Cys to Cys-Pro-Pro-Cys) or the CH 3 domain76 . igG4 can bind to some FcγRs, includ- ing FcγRi77,78 — an interaction that can be weakened by point mutations to abolish ADCC activity79 . Antibodies lacking effector functions can also be created with hybrid isotype igG molecules that mimic the desired attributes of their component isotypes. For example, the complement component C5-specific anti- body eculizumab (Soliris; Alexion pharmaceuticals) (TABLE 1) uses a hybrid igG2–igG4 constant region that includes the CH 1 domain and hinge region of a human igG2 fused to the CH 2 and CH 3 domains of a human igG4. Eculizumab lacks the ability to bind FcγRs and activate complement, which are common attributes for human igG2 and igG4, respectively80 . Strategies to eliminate effector functions are readily extended to Fc fusion proteins. For example, the cyto- toxic T lymphocyte antigen 4 (CTlA4)–Fc fusion pro- tein abatacept (orencia; Bristol-Myers Squibb) has five mutations compared with human igG1: lys215Gln, Cys220Ser, Cys226Ser, Cys229Ser and Pro238Ser81 (Eu numbering82 ). Multiple functional consequences of these mutations include improved protein production, elimination of inter-chain disulphide bonds and O-linked glycosylation by virtue of the mutated hinge (Cys-Pro- Ser-Cys to Ser-Pro-Pro-Cys), inefficient binding to FcγRs and lack of ADCC and CDC activity12,81 . A seemingly small risk in making Fc mutations to ablate effector functions is that they might lead to del- eterious structural perturbations. introducing the triple mutation lys234Phe:lys235Glu:Pro331Ser (‘FES’) into an igG1 molecule caused a substantial decrease in bind- ing to FcγRs and the complement component C1q164 . The structure of FES Fc is similar to other human Fc structures164 . Thus the FES mutations designed to ablate effector functions probably do so without causing undue structural perturbation of the Fc domain. Many different engineered antibody fragments have been developed including several that have entered clini- cal development70 . Many antibody fragments lack the igG Fcregionanditsassociatedproperties—effectorfunctions and extended half-life. As discussed previously, certolizu- mab pegol, a humanized TNF-specific Fabʹ fragment, is PEGylated to extend its pharmacokinetic half-life and is the first FDA-approved PEGylated antibody fragment for clinical use (TABLE 1). Whereas Fab fragments have a ter- minal half-life of ~20 minutes, certolizumab pegol has a half-life of ~14 days in patients, similar to its parent igG83 . Enhancing effector functions. For some antibodies, potent effector functions, as described previously for rituximab, may be required for optimal clinical activ- ity. Antibodies with efficient effector functions can be identified directly by screening panels of antibodies84 , engineering to improve the activities of existing antibod- ies10–12 or a combination of both of these approaches. Potential benefits from enhancing effector functions include greater therapeutic efficacy, lower or less fre- quent dosing and decreased cost of goods. Potential risks from enhanced effector functions include more frequent or severe adverse events in patients. ADCC activity can be enhanced by engineering the Fc protein sequence or tailoring the Fc carbohydrates to strengthen binding to FcγRs, most importantly FcγRiiiA11,12 . Detailed mutational analysis of igG1 iden- tified the functionally important Fc residues for bind- ing to the different FcγRs (FcγRi, FcγRiiA, FcγRiiB and FcγRiiiA) and FcRn, as well as igG1 mutants with increased binding to FcγRiiiA and increased ADCC activity85 .ADCC-enhancingmutantshavealsobeeniden- tified from yeast display libraries86 . Computational design based on the structures of Fc–FcγR complexes together with functional screening has identified several mutants with up to ~100-fold higher affinity binding for FcγRiiiA. one such mutant, Ser239Asp:Glu330leu:ile332Glu, gave a ~100-fold increase in ADCC potency, with greater maximal target cell killing in some cases87 . Fc protein engineering to enhance ADCC is broadly applicable as shown with variants of several therapeutically relevant antibodies: trastuzumab (Herceptin; Genentech/Roche), cetuximab (Erbitux; imClone Systems), rituximab and alemtuzumab87 . ADCC-enhancing antibodies can kill cells expressing lower levels of antigen, as shown with trastuzumab variants87 — a potential benefit for improved efficacy, albeit with unknown risk of killing non-target cells expressing low levels of antigen. ADCP activity can also be enhanced through Fc pro- tein engineering. For example, a Gly236Ala mutation increases igG1 affinity for FcγRiiA 70-fold, and it has a 15-fold improvement in the selectivity of binding to this activating receptor over the related inhibitory receptor FcγRiiB88 . The Gly236Ala mutation enhances phago- cytosis of antibody-coated target cells by macrophages. ADCPandADCCweresimultaneouslyenhancedbycom- bining Gly236Ala and Ser239Asp:ile332Glu mutations that enhance ADCP and ADCC, respectively88 . Aglycosylated igG molecules bind poorly to FcγRs and do not support ADCC. By contrast, bacterial dis- play selection was used to identify a double mutant, Glu382val:Met428ile, that endows aglycosylated igG1 with the ability to bind FcγRi with high (nanomolar) affinity and support ADCC89 . Moreover, the binding was remarkably selective for FcγRi with no detectable binding to the other FcγRs. The Glu382val:Met428ile mutations did not affect FcRn binding in vitro or serum persistence in vivo. Thus, aglycosylated igG can be engi- neered with selectivity profiles for FcγRs that are distinct from those of glycosylated igG89 . Asecondwidelyapplicableandcomparablysuccessful method for increasing the igG ADCC activity is through tailoring of Fc glycosylation11,90 . Antibody production in a Chinese hamster ovary (CHo) cell line transfected to overexpress N-acetylglucosaminyltransferaseiii resulted in antibodies linked to carbohydrate with a bisect- ing N-acetylglucosamine and more potent ADCC91 . Decreasing the fucose content of the carbohydrates in the Fc region can also enhance ADCC92,93 . Production of antibodies devoid of fucose is readily achieved using CHo cells that lack expression of fucosyltransferase 8 (REF. 94). Total elimination of fucosylated antibodies is important to avoid competition with, and reduction of, the activity of the more potent non-fucosylated REVIEWs 310 | MAy 2010 | volUME 10 www.nature.com/reviews/immunol REVIEWs © 20 Macmillan Publishers Limited. All rights reserved 10
- 11. Exposure In the pharmacokinetic sense, the area under the curve for a plot of drug concentration versus time. antibodies95 . other host organisms are used to pro- duce non-fucosylated antibodies, including extensively engineered strains of Pichia pastoris96 . Most licensed therapeutic antibodies are exten- sively fucosylated11 , and their in vitro ADCC activity is decreased by the presence of serum, presumably because of competition for FcγRiiiA with high concentrations of irrelevant igG. By contrast, non-fucosylated variants of rituximab and trastuzumab have increased affinity for FcγRiiiA and ~100-fold more potent ADCC activity that is minimally affected by serum igG95 . The increases in ADCC potency achieved from Fc mutations87 and non-fucosylation95 seem to be similar as judged by corresponding variants of trastuzumab and rituximab. The binding site on human igG1 for complement component C1q has been identified by mutational analy- sis97 .Thisledtothegenerationofarituximabvariantwith improved complement binding97 and ~twofold greater CDC activity, albeit with slightly impaired ADCC activ- ity98 . Enhancement of antibody CDC activity has also been achieved using hinge-region mutations99 . increased CDC activity has recently been achieved by creating a hybrid isotype igG in which some igG1 residues were replaced with corresponding igG3 sequences100 . A few additional igG1 residues were required to restore effi- cient binding to protein A to allow purification100 . An antibody enhanced in both CDC and ADCC activities was created by combining Fc protein mutations with non-fucosylation100 . The efficacy and safety of antibodies with enhanced effector functions are challenging to assess preclinically because of species differences between the immune sys- tems of mice and humans. CD20-specific antibodies with high ADCC activity have been evaluated in cynomolgus macaques using B cell depletion as a surrogate for effi- cacy87,101 .Severalantibodieswithpotenteffectorfunctions have progressed into clinical development. For example, human CD20-specific antibodies were obtained from transgenic mice with potent CDC activity even against tumour cell lines expressing high levels of complement regulatory proteins, CD55 and CD59, that are resistant to CDC by rituximab84 . one of these human CD20- specific antibodies, ofatumumab (Arzerra; Genmab/ GlaxoSmithKline), is now licensed for the treatment of chronic lymphocytic leukaemia and is under clinical evaluation for rheumatoid arthritis, multiple sclerosis and other cancers (TABLE 1). Another CD20-specific antibody, ocrelizumab (2H7; Genentech/Roche/Biogen idec), has in vitro ADCC and CDC activities that are higher and lower than rituximab, respectively102 . ocrelizumab has advanced to Phase iii clinical trials for rheumatoid arthritis and systemic lupus erythematosus (TABLE 1). At least eight effector function-enhanced antibodies have progressed into clinical development. For example, GA-101 (Roche/GlycArt) is a humanized type ii CD20- specific antibody that is glyco-engineered (bisected and non-fucosylated) to enhance ADCC and is in Phase ii clinical trials for non-Hodgkin’s lymphoma103 . other clinical stage glyco-engineered antibodies include a non-fucosylated humanized il-5R-specific antibody MEDi-563 (BioWa/Medimmune). A single intravenous dose of MEDi-563 of only 30 μg/kg — much lower than for most antibody drugs — was well tolerated and induced robust and reversible blood eosinopenia in all six mildly asthmatic patients treated11,104 . ADCC- improved antibodies containing Fc mutations have also entered clinical development, including the humanized CD30-specific antibody Xmab2513 (Xencor) that is in a Phase i clinical trial for Hodgkin’s and anaplastic large cell lymphomas. A distinct mode of depleting CD20-specific antibod- ies has emerged for the treatment of B cell malignancies that has implications potentially for future depleting therapies in autoimmune and inflammatory diseases. CD20-specific antibodies can be defined as either type i (exemplified by rituximab) or type ii (such as tositu- momab (Bexxar; Corixa/GlaxoSmithKline))105 . Type ii, but not type i, CD20-specific antibodies induce an actin- dependenthomotypicadhesionandaggregationofCD20- bearing cells106 . Through an unknown mechanism, type ii antibodies trigger lysosome destabilization and release of lysosomal contents to mediate a caspase- and B cell lymphoma 2 (BCl-2)-independent form of cell death. Should these mechanisms prove effective in human malignancies, they offer a distinct therapeutic option to deplete all CD20-bearing cellular niches. Pharmacokinetic half-life extension. The terminal half-life for chimeric, humanized and human antibody drugs in the circulation varies widely (~3–27 days)107 . Engineering antibodies to increase their serum half- life and exposure offers the potential benefits of greater efficacy, lower or less frequent dosing, lower cost and enhanced localization to the target. The interaction between the Fc region of igG and the recycling receptor FcRn has a key role in igG homeostasis and is largely responsible for the long half-life of igG108 : ~21 days in humans for igG1 (REF. 109). igG, like other circulating proteins, is taken up by vascular endothelial cells and other cells by pinocytosis. Subsequently,igG can interact with the FcRn, in a pH-dependent manner with binding occurring in endosomes at pH 6.0–6.5, followed by recycling and release at the cell surface at pH 7.0–7.4. Fc engineering to modulate the FcRn interaction and extend igG half-life is discussed briefly here and in greater depth elsewhere10,12 . An important early milestone was the identification of Fc mutations from phage display libraries that strengthen Fc binding to FcRn and prolong the half-life of mouse igG in mice110 . Subsequently, Fc mutations (Thr250Gln:Met428leu; ‘Ql’) were identified that increase the binding affinity of a human igG2 for human FcRn at pH 6.0 but not at pH 7.4 (REF. 111). These Ql mutations confer a similar pH-dependent increase in binding of a human igG2 to rhesus FcRn and a ~twofold increase in serum half-life in rhesus macaques111 . The Ql mutations had a similar effect in extending the half-life of a human igG1 in rhesus macaques112 . The Ql muta- tions also increased the binding affinity of a TNF-specific igG1 to FcRn from cynomolgus macaques, albeit without extending half-life for unknown reasons113 . Alternative mutations have been identified that extend the half-life of antibodies in non-human primates. For example, the REVIEWs NATURE REviEWS | Immunology volUME 10 | MAy 2010 | 311 focus on THERAPEuTIc AnTIBoDIEs © 20 Macmillan Publishers Limited. All rights reserved 10
- 12. triple Fc mutation, Met252Tyr:Ser254Thr:Thr256Glu (‘yTE’) increases the half-life of a humanized respira- tory syncytial virus (RSv)-specific igG1 in cynomolgus macaques by three–fourfold114 . The X-ray crystallo- graphic structure of the yTE Fc is similar to other Fc structures, strongly suggesting that the yTE mutations do not significantly perturb the Fc structure115 . Fc mutations that extend pharmacokinetic half- life can also enhance in vivo efficacy, which has been recently shown for the first time116 . The double muta- tion Met428leu:Asn434Ser (‘lS’) engineered into the vascular endothelial growth factor (vEGF)-specific antibody bevacizumab (Avastin; Genentech) extended serum half-life by ~threefold in cynomolgus mon- keys and by ~fourfold in engineered mice expressing human, but not mouse, FcRn116 . Moreover, the lS muta- tions increased the antitumour activity of bevacizumab in a xenograft study in mice. in addition, a humanized version of the chimeric epidermal growth factor receptor (EGFR)-specific antibody cetuximab engineered with the lS mutations out-performed cetuximab in vivo, extended half-lifeincynomolgusmonkeys(~threefold)andinengi- neered mice (~fivefold), and had superior antitumour activity in mice. Studies in primates with engineered antibodies (see above) support the feasibility of extending the plasma half-life of therapeutic antibodies by tailoring the interac- tionofFcwithFcRn.indeed,thehumanizedRSv-specific igG1 with yTE mutations (MEDi-557) is currently in Phase i clinical trials to explore this possibility. The half- life-extending yTE mutations have also been successfully combined with mutations that enhance ADCC as judged by potent in vitro activity in cytotoxicity assays114 . Species differences in FcRn–Fc interactions between mice and humans add much complexity to the preclini- cal analysis of antibodies engineered for extended half- life117 . Transgenic mice expressing human FcRn may offer a partial solution to this challenge118 . An engineered igG that binds to FcRn at both neutral and slightly acidic pH is more rapidly cleared than wild-type igG119 . Thus, maintaining the strict pH dependence of Fc binding to FcRn is apparently crucial for supporting the long half- life of igG. An igG engineered to bind FcRn with higher affinity and reduced pH dependence potently inhibits the interaction of FcRn with endogenous igG and rapidly lowers the concentration of circulating igG in mice120 . These FcRn-blocking antibodies known as ‘Abdegs’ may have therapeutic potential for reducing pathogenic igG levels in antibody-mediated autoimmune diseases120 . Pharmacokinetic half-life reduction. For some therapeu- tic antibodies, it may be advantageous to decrease their terminal half-life to decrease exposure, improve safety or, in the case of some imaging applications, improve the target/non-target localization ratios. A large reduc- tion in antibody half-life — from weeks to hours or less — is readily achieved by using small antibody frag- ments susceptible to renal elimination and that lack a functional Fc region to preclude recycling by FcRn. indeed, two unmodified Fab fragments are licensed for human therapy: the integrin-specific Fab abciximab (ReoPro; Eli lilly) for the prevention of platelet-mediated clot in coronary angioplasty and the vEGF-specific Fab ranibizumab (lucentis; Genentech) for the treatment of neovascular (wet) age-related macular degeneration. it may be desirable to tune the pharmacokinetic properties of some antibody drugs to achieve half-lives that are intermediate between small antibody fragments and igG. This can be accomplished by Fc mutations that attenuate the interaction with FcRn and decrease anti- body half-life, as shown by pharmacokinetic optimiza- tion of single-chain (sc)Fv–Fc antibody fragments for tumour imaging121 . Antibody fragments with a wide range of terminal half-lives — from a few hours to days — can be generated through site-specific PEGylation122 . Several PEGylated proteins are licensed for human therapy123 including one PEGylated antibody fragment, certolizumab pegol, that has igG-like pharmacokinetic behaviour. The pharmacokinetic properties of PEGylated proteins can be tuned by varying the size and extent of branching of the PEG molecules, sites of attachment and number of PEG molecules attached per protein123 . Several alternative strategies have been developed to extend the half-lives of antibody fragments and other proteins including genetic fusion to albumin124 , igG Fc125 or an unstructured recombinant polypeptide (XTEN)126 , engineering them with the ability to bind long-circulating proteins such as albumin127 or igG128 , or by creating new glycosylation sites129 . Fc mutations that impair interaction with FcRn can decrease antibody half-life as exemplified by pharmacokinetic optimization of scFv–Fc antibody fragments for tumour imaging121 . Optimization of antigen-binding domains Engineering of antibody variable domains to increase the binding affinity for antigen or tune the binding spe- cificity has been extensively reviewed elsewhere10 and is not discussed further here. Two major strategies gaining momentum for endowing antibodies with new activities are antibody–drug conjugates130 and bispecific antibod- ies131,132 , which are mainly used for targeting cytotoxic drugs and effector cells, respectively, to kill tumour cells. Bispecific antibodies have additional potential applica- tions including dual blockade of disease mediators133 , as discussed here. Bispecific antibodies. The concept of bispecific antibod- ies was first suggested nearly 50 years ago134 , and it is finally coming of age for the generation of therapeutic agents131,132 . Historically, a major obstacle to developing bispecific antibodies as therapeutic agents has been the difficulty in designing these complex molecules with favourable drug-like properties and producing them in sufficient quantity and quality to support drug develop- ment.Bispecificantibodiesaspotentialtherapeuticagents have undergone a renaissance in recent years, facilitated by the advent of numerous alternative formats and improved methods for their more efficient generation, optimization and production132,133,135 (FIG. 3). Moreover, greater understanding of disease pathogenesis is leading to better choices of target antigen and antibody pairs. Here we propose ideal attributes of bispecific antibodies REVIEWs 312 | MAy 2010 | volUME 10 www.nature.com/reviews/immunol REVIEWs © 20 Macmillan Publishers Limited. All rights reserved 10
- 13. Valency For antibodies, including bispecific antibodies, the number of binding sites for each cognate antigen. for drug development based on experience with antibod- ies and other biological drugs. Additionally, advances in selected technologies for generating bispecific antibodies for therapeutic applications are presented (FIG. 3). The most successful clinical application of bispecific antibodies to date has been in oncology by redirect- ing cytotoxic T cells to kill tumour cells. This concept was originally proposed in 1985 (REF. 136) and has been explored in the context of several different bispecific anti- body formats. The most successful format identified to date for this application is a tandem scFv (FIG. 3) known as a ‘BiTE’ (bispecific T cell engager). Blinatumomab (MT103; Micromet/Medimmune), a BiTE specific for CD19 and CD3, has been used to treat patients with non- Hodgkin’s lymphoma137 . Complete and partial responses were observed with blinatumomab administered at doses as low as 0.15 μg per m2 per day137 , that is, doses at least 10,000 times lower than those typically used for thera- peutic igG1 antibodies for targeting tumours. BiTEs are rapidly cleared, necessitating administration by a port- able mini-pump; however a possible benefit is fine dos- ing control. Adverse events with blinatumomab include neurologicalsymptomsthatareseeminglyreversible.This early clinical success with BiTEs has encouraged further pursuit of this format, including targeting of many differ- ent tumour antigens131 . Several additional applications of bispecificantibodieshavebeeninvestigated133,135 ,including blockade of several disease mediators as discussed here. Designing bispecific antibodies as therapeutic agents. An ideal bispecific antibody format for therapeutic appli- cations would be broadly applicable to different combi- nations of target antigens without requiring extensive customizationforindividualantibodypairs.Routinehigh- level expression (gram per litre) of bispecific antibody will probably be needed to support manufacturing for clini- cal development, preferably in well established and widely available host production systems such as CHo cells or E. coli. Bispecific antibodies should preserve the antigen- binding affinity and beneficial biological activities of their component monospecific antibodies. Bispecific antibody design preferably facilitates purification to homogene- ity and recovery in high yield. Simultaneous binding of both antigens to the bispecific antibody is desirable and may be essential depending on the application. Selection of the bispecific antibody format to match the valency of each component antibody to the biology of the target antigens may be necessary, and is readily achievable from the many alternative formats (FIG. 3). Bispecific antibodies need favourable physicochemical properties such as high solubility and stability plus low propensity to aggregate, as suggested by successful biological drugs. Bispecific antibodies have pharmacokinetic properties that are suit- able for their intended clinical application — long serum half-life in many cases. Dual blockade of disease mediators with bispecific antibodies. The pathogenesis of many human diseases involves several mediators that function in distinct sig- nalling pathways or that have redundant roles in the same pathway. Simultaneous blockade of several different disease mediators may lead to greater therapeutic effi- cacy and/or benefit more patients than targeting indi- vidual disease mediators133 . This dual targeting concept was initially explored in oncology with bispecific anti- bodies that bind vEGFR1 and vEGFR2 (REF. 138), EGFR and insulin-like growth factor receptor 1 (iGFR1)139,140 . More recently the human epidermal growth factor receptor 2 (HER2)-specific antibody trastuzumab was engineered using phage display technology to create a ‘two-in-one’ antibody (FIG. 3c) that can bind either HER2 or vEGF with high affinity; it was shown to inhibit both HER2- and vEGF-mediated cell proliferation in vitro and tumour progression in mouse models141 . Although this combinatorial strategy is currently being pursued in many cancers, combinatorial therapy has been limited, to date, by significant safety issues when used in inflammatory diseases. Combination of il-1β and TNF blockade by anakinra and etanercept, respec- tively, as well as dual targeting of TNF (by etanercept) and CD80 and CD86 (by abatacept (orencia; Bristol- Myers Squibb)) did not result in any significant additive or synergistic clinical effects, but rather in a substantial increase in infectious complications142,143 . Nonetheless, dual targeting of more appropriate pathways may pro- vide greater efficacy without significantly increased toxicities. in turn, bispecific antibodies seem preferable in these cases, as opposed to developing two unapproved therapeutic antibodies, for reasons that include lower costs, simpler clinical drug development schemes and more traditional regulatory pathways. The pro-inflammatory cytokines il-1α and il-1β have key and seemingly redundant roles in the patho- genesis of various diseases144 . indeed, blockade of both il-1α and il-1β in a mouse model of collagen-induced arthritis using a combination of monospecific neutraliz- ing antibodies was more efficacious than either individual antibody145,146 . These antibody combination studies pro- vide a strong rationale for developing therapeutic agents thatneutralizeboth il-1αandil-1β,ideallywithoutinter- fering with endogenous il-1Ra147,148 . identifying a single antibody that binds to both il-1α and il-1β has proved elusive, as these cytokines share only ~20% identity. By contrast, a new bispecific tetravalent igG-like molecule known as dual variable domain igG (DvD-igG; FIG. 3c) was generated that neutralizes both mouse il-1α and il-1β and has similar in vivo potency to a combination of the two monospecific igGs from which it was derived148 . ADvD-igGbindinghumanil-1αandil-1βwasthencre- ated, allowing clinical evaluation147 . A further DvD-igG, comprising il-12-specific and il-18-specific antibodies, suggests that this format may be broadly applicable148 . DvD-igG can match or at least approach the bind- ing affinity of the parent antibodies, although some optimization may be required; for example, antibody selection, order of antigen-binding variable domains and design of linkers connecting variable domains147,148 . DvD-igG can be generated with many attributes condu- cive to drug development, including robust expression in mammalian cells and facile purification by protein A chromatography, as well as favourable physicochemical and pharmacokinetic properties147,148 . REVIEWs NATURE REviEWS | Immunology volUME 10 | MAy 2010 | 313 focus on THERAPEuTIc AnTIBoDIEs © 20 Macmillan Publishers Limited. All rights reserved 10
- 14. Functional blockade of additional cytokine pairs has been achieved with several different bispecific antibody formats. T helper 17 (TH 17) cells may be associated with the pathogenesis of some allergic diseases such as allergic contact dermatitis, atopic dermatitis and asthma149 . Dual targeting of il-23, a TH 17 cell growth and survival factor, and il-17A, a pro-inflammatory cytokine produced by TH 17 cells, may be more effective than blockade of either il-23 or il-17A alone in inflammatory diseases involv- ing TH 17 cells150 . Selection from phage display libraries was used to generate and optimize stable and high affin- ity scFv neutralizing either il-17A or il-23. Bispecific antibodies binding to both il-17A and il-23 were then generated by incorporating these monospecific scFv into a several previously described bispecific antibody formats150 : tandem scFv–Fc151 , scFv–Fc–scFv152 and igG– scFv153 (FIG. 3). Bispecific antibodies were identified that potently neutralize both il-17A and il-23 with good stability and pharmacokinetic properties. These findings support the design principle of constructing bispecific antibodies from stable monomeric building blocks154 . Concluding remarks Much has been learnt from the clinical experiences of the first generation of therapeutic antibodies. We have reviewed here some of the insights derived from the first decade of therapeutic antibodies in autoimmunity and inflammation as well as a subset of the technologi- cal advances that will enhance the capabilities of thera- peutic antibodies. The experiences from this second generation of therapeutic antibodies will undoubtedly inform our next generation of therapeutic antibodies. Although not discussed in this Review, there is much to be learnt about how antibody delivery, as well as other factors, can alter the distribution of antibody in the body. These include oral delivery of antibodies, development of sustained release platforms that can be used in the eye to avoid frequent intravitreous injections and improved access of therapeutic antibodies into the brain. Although rituximab and alemtuzumab have shown preliminary evidence of efficacy in the relapsing–remitting form of multiple sclerosis, steady state cerebrospinal fluid levels of rituximab in relapsing–remitting multiple sclerosis are low (<0.25 to <0.1% of serum levels)155 . A better under- standing of the factors that regulate the dynamics of antibody circulation between the systemic and central nervous system compartments may allow the design of therapeutic antibodies with improved access to cerebral spinal fluid and application of therapeutic antibodies in a wide range of neurological diseases. We are merely at the dawn of antibody-based therapy and have much to look forward to as we begin this exciting journey. 1. Reichert, J. M. Antibodies to watch in 2010. mAbs 2, 28–45 (2010). An excellent overview of therapeutic antibodies in Phase III clinical trials and beyond. 2. Scolnik, P. A. mAbs a business perspective. mAbs 1, 179–184 (2009). 3. Köhler, G. & Milstein, C. Continuous cultures of fused cells secreting antibody of predefined specificity. Nature 256, 495–497 (1975). 4. Almagro, J. C. & Fransson, J. Humanization of antibodies. Front. Biosci. 13, 1619–1633 (2008). 5. Reichert, J. M. Monoclonal antibodies as innovative therapeutics. Curr. Pharm. Biotechnol. 9, 423–430 (2008). 6. Lonberg, N. Fully human antibodies from transgenic mouse and phage display platforms. Curr. Opin. Immunol. 20, 450–459 (2008). 7. Mondon, P., Dubreuil, O., Bouayadi, K. & Kharrat, H. Human antibody libraries: a race to engineer and explore a larger diversity. Front. Biosci. 13, 1117–1129 (2008). 8. Parren, P. W. & van de Winkel, J. G. An integrated science-based approach to drug development. Curr. Opin. Immunol. 20, 426–430 (2008). 9. Kelley, B. Industralization of mAb production technology. The bioprocess industry at a crossroads. mAbs 1, 443–452 (2009). 10. Carter, P. J. Potent antibody therapeutics by design. Nature Rev. Immunol. 6, 343–357 (2006). 11. Kubota, T. et al. Engineered therapeutic antibodies with improved effector functions. Cancer Sci. 100, 1566–1572 (2009). 12. Presta, L. G. Molecular engineering and design of therapeutic antibodies. Curr. Opin. Immunol. 20, 460–470 (2008). References 11 and 12 provide a detailed summary of Fc engineering to enhance ADCC and CDC activity of IgG, as well as to extend serum half-life. 13. Targan, S. R. et al. A short-term study of chimeric monoclonal antibody cA2 to tumor necrosis factor α for Crohn’s disease. Crohn’s Disease cA2 Study Group. N. Engl. J. Med. 337, 1029–1035 (1997). 14. Tracey, D., Klareskog, L., Sasso, E. H., Salfeld, J. G. & Tak, P. P. Tumor necrosis factor antagonist mechanisms of action: a comprehensive review. Pharmacol. Ther. 117, 244–279 (2008). 15. Baert, F. et al. Influence of immunogenicity on the long-term efficacy of infliximab in Crohn’s disease. N. Engl. J. Med. 348, 601–608 (2003). 16. Hanauer, S. B. et al. Maintenance infliximab for Crohn’s disease: the ACCENT I randomised trial. Lancet 359, 1541–1549 (2002). 17. Vultaggio, A. et al. Anti-infliximab IgE and non-IgE antibodies and induction of infusion-related severe anaphylactic reactions. Allergy 27 Nov 2009 (doi: 10.1111/j.1398-9995.2009.02280.x). 18. Radstake, T. R. et al. Formation of antibodies against infliximab and adalimumab strongly correlates with functional drug levels and clinical responses in rheumatoid arthritis. Ann. Rheum. Dis. 68, 1739–1745 (2009). 19. Weinblatt, M. E. et al. Adalimumab, a fully human anti-tumor necrosis factor α monoclonal antibody, for the treatment of rheumatoid arthritis in patients taking concomitant methotrexate: the ARMADA trial. Arthritis Rheum. 48, 35–45 (2003). 20. Bartelds, G. M. et al. Clinical response to adalimumab: relationship to anti-adalimumab antibodies and serum adalimumab concentrations in rheumatoid arthritis. Ann. Rheum. Dis. 66, 921–926 (2007). 21. Emery, P. et al. Golimumab, a human anti-tumor necrosis factor α monoclonal antibody, injected subcutaneously every four weeks in methotrexate- naive patients with active rheumatoid arthritis: twenty-four-week results of a phase III, multicenter, randomized, double-blind, placebo-controlled study of golimumab before methotrexate as first-line therapy for early-onset rheumatoid arthritis. Arthritis Rheum. 60, 2272–2283 (2009). 22. Lugering, A. et al. Infliximab induces apoptosis in monocytes from patients with chronic active Crohn’s disease by using a caspase-dependent pathway. Gastroenterol. 121, 1145–1157 (2001). 23. Scallon, B. J., Moore, M. A., Trinh, H., Knight, D. M. & Ghrayeb, J. Chimeric anti-TNF-α momoclonal cA2 binds recombinant transmembrane TNF-α and activates immune effector functions. Cytokine 7, 251–259 (1995). 24. Van den Brande, J. M. et al. Infliximab but not etanercept induces apoptosis in lamina propria T-lymphocytes from patients with Crohn’s disease. Gastroenterol. 124, 1774–1785 (2003). 25. Fossati, G. & Nesbitt, A. M. Effect of the anti-TNF agents, adalimumab, etanercept, infliximab, and certolizumab PEGOL (CDP870) on the induction of apoptosis in activated peripheral blood lymphocytes and monocytes. Am. J. Gastroenterol. 100, S298–S299 (2005). 26. Sandborn, W. J. et al. Certolizumab pegol for the treatment of Crohn’s disease. N. Engl. J. Med. 357, 228–238 (2007). 27. Schreiber, S. et al. Maintenance therapy with certolizumab pegol for Crohn’s disease. N. Engl. J. Med. 357, 239–250 (2007). 28. Hawkins, P. N., Lachmann, H. J., Aganna, E. & McDermott, M. F. Spectrum of clinical features in Muckle-Wells syndrome and response to anakinra. Arthritis Rheum. 50, 607–612 (2004). 29. Lachmann, H. J. et al. In vivo regulation of interleukin 1β in patients with cryopyrin-associated periodic syndromes. J. Exp. Med. 206, 1029–1036 (2009). 30. Leonardi, C. L. et al. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 76-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 1). Lancet 371, 1665–1674 (2008). 31. Papp, K. A. et al. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 52-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 2). Lancet 371, 1675–1684 (2008). 32. Sandborn, W. J. et al. A randomized trial of Ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with moderate-to-severe Crohn’s disease. Gastroenterol. 135, 1130–1141 (2008). 33. Guttman-Yassky, E. et al. Blockade of CD11a by efalizumab in psoriasis patients induces a unique state of T-cell hyporesponsiveness. J. Invest. Dermatol. 128, 1182–1191 (2008). 34. Bousquet, J. et al. The effect of treatment with omalizumab, an anti-IgE antibody, on asthma exacerbations and emergency medical visits in patients with severe persistent asthma. Allergy 60, 302–308 (2005). 35. Beck, L. A., Marcotte, G. V., MacGlashan, D., Togias, A. & Saini, S. Omalizumab-induced reductions in mast cell Fcε RI expression and function. J. Allergy Clin. Immunol. 114, 527–530 (2004). 36. MacGlashan D. W. Jr et al. Down-regulation of FcεRI expression on human basophils during in vivo treatment of atopic patients with anti-IgE antibody. J. Immunol. 158, 1438–1445 (1997). 37. Prussin, C. et al. Omalizumab treatment downregulates dendritic cell FcεRI expression. J. Allergy Clin. Immunol. 112, 1147–1154 (2003). 38. MacGlashan, D. W. Jr. Endocytosis, recycling, and degradation of unoccupied FcεRI in human basophils. J. Leukoc. Biol. 82, 1003–1010 (2007). REVIEWs 314 | MAy 2010 | volUME 10 www.nature.com/reviews/immunol REVIEWs © 20 Macmillan Publishers Limited. All rights reserved 10
- 15. 39. Blume, J. W., Kiratseavee, S. & Sands, M. F. Resolution of angioedema with omalizumab. J. Allergy Clin. Immunol. 119, S274 (2007). 40. Gober, L. M., Sterba, P. M., Eckman, J. A. & Saini, S. S. Effect of anti-IgE (omalizumab) in chronic idiopathic urticaria (CIU) patients. J. Allergy Clin. Immunol. 121, S147 (2008). 41. Shapiro, C. A., Kapatanos, N. S. & Sarmiento, E. Successful treatment of chronic idiopathic urticaria and angioedema (CIU) with Xolair (omalizumab). J. Allergy Clin. Immunol. 119, S274 (2007). 42. Eckman, J. A., Hamilton, R. G., Gober, L. M., Sterba, P. M. & Saini, S. S. Basophil phenotypes in chronic idiopathic urticaria in relation to disease activity and autoantibodies. J. Investig. Dermatol. 128, 1956–1963 (2008). 43. Ferrer, M., Kinet, J. P. & Kaplan, A. P. Comparative studies of functional and binding assays for IgG anti- FcεR1α (α-subunit) in chronic urticaria. J. Allergy Clin. Immunol. 101, 672–676 (1998). 44. Cohen, S. B. et al. Rituximab for rheumatoid arthritis refractory to anti-tumor necrosis factor therapy: results of a multicenter, randomized, double-blind, placebo- controlled, phase III trial evaluating primary efficacy and safety at twenty-four weeks. Arthritis Rheum. 54, 2793–2806 (2006). 45. Hauser, S. L. et al. B-cell depletion with rituximab in relapsing-remitting multiple sclerosis. N. Engl. J. Med. 358, 676–688 (2008). 46. Coles, A. J. et al. Alemtuzumab vs. interferon β-1a in early multiple sclerosis. N. Engl. J. Med. 359, 1786–1801 (2008). 47. Genovese, M. C. et al. Ocrelizumab, a humanized anti-CD20 monoclonal antibody, in the treatment of patients with rheumatoid arthritis: A phase I/II randomized, blinded, placebo-controlled, dose-ranging study. Arthritis Rheum. 58, 2652–2661 (2008). 48. Jacobi, A. M. et al. Differential effects of epratuzumab on peripheral blood B cells of patients with systemic lupus erythematosus versus normal controls. Ann. Rheum. Dis. 67, 450–457 (2008). 49. Golay, J. et al. CD20 levels determine the in vitro susceptibility to rituximab and complement of B-cell chronic lymphocytic leukemia: further regulation by CD55 and CD59. Blood 98, 3383–3389 (2001). 50. Gong, Q. et al. Importance of cellular microenvironment and circulatory dynamics in B cell immunotherapy. J. Immunol. 174, 817–826 (2005). 51. Minard-Colin, V. et al. Lymphoma depletion during CD20 immunotherapy in mice is mediated by macrophage FcγRI, FcγRIII, and FcγRIV. Blood 112, 1205–1213 (2008). 52. Natsume, A., Shimizu-Yokoyama, Y., Satoh, M., Shitara, K. & Niwa, R. Engineered anti-CD20 antibodies with enhanced complement-activating capacity mediate potent anti-lymphoma activity. Cancer Sci. 100, 2411–2418 (2009). 53. Cartron, G. et al. Therapeutic activity of humanized anti-CD20 monoclonal antibody and polymorphism in IgG Fc receptor FcγRIIIa gene. Blood 99, 754–758 (2002). This paper was the first to show an association between responsiveness to antibody therapy and a polymorphism in the gene encoding FcγRIII in patients, which strongly implicates an Fc or FcγR-mediated mechanism, such as ADCC, in the antitumour activity of rituximab. 54. Weng, W. K. & Levy, R. Two immunoglobulin G fragment C receptor polymorphisms independently predict response to rituximab in patients with follicular lymphoma. J. Clin. Oncol. 21, 3940–3947 (2003). 55. Anolik, J. H. et al. The relationship of FcγRIIIa genotype to degree of B cell depletion by rituximab in the treatment of systemic lupus erythematosus. Arthritis Rheum. 48, 455–459 (2003). 56. Johnson, N. A. et al. Diffuse large B-cell lymphoma: reduced CD20 expression is associated with an inferior survival. Blood 113, 3773–3780 (2009). 57. Olejniczak, S. H., Stewart, C. C., Donohue, K. & Czuczman, M. S. A quantitative exploration of surface antigen expression in common B-cell malignancies using flow cytometry. Immunol. Invest. 35, 93–114 (2006). 58. van Meerten, T., van Rijn, R. S., Hol, S., Hagenbeek, A. & Ebeling, S. B. Complement-induced cell death by rituximab depends on CD20 expression level and acts complementary to antibody-dependent cellular cytotoxicity. Clin. Cancer Res. 12, 4027–4035 (2006). 59. Di Gaetano, N. et al. Complement activation determines the therapeutic activity of rituximab in vivo. J. Immunol. 171, 1581–1587 (2003). 60. Weng, W. K. & Levy, R. Expression of complement inhibitors CD46, CD55, and CD59 on tumor cells does not predict clinical outcome after rituximab treatment in follicular non-Hodgkin lymphoma. Blood 98, 1352–1357 (2001). 61. Kavanaugh, A. et al. Assessment of rituximab’s immunomodulatory synovial effects (ARISE trial). 1: clinical and synovial biomarker results. Ann. Rheum. Dis. 67, 402–408 (2008). 62. Walsh, C. A., Fearon, U., FitzGerald, O., Veale, D. J. & Bresnihan, B. Decreased CD20 expression in rheumatoid arthritis synovium following 8 weeks of rituximab therapy. Clin. Exp. Rheumatol. 26, 656–658 (2008). 63. Herold, K. C. et al. Anti-CD3 monoclonal antibody in new-onset type 1 diabetes mellitus. N. Engl. J. Med. 346, 1692–1698 (2002). 64. Smith, S. L. Ten years of orthoclone OKT3 (muromonab–CD3): a review. J. Transplant. Coord. 6, 109–121 (1996). 65. Norman, D. J., Chatenoud, L., Cohen, D., Goldman, M. & Shield, C. F. Consensus statement regarding OKT3- induced cytokine-release syndrome and human antimouse antibodies. Transplant. Proc. 25, 89–92 (1993). 66. Chatenoud, L. Anti-CD3 antibodies: towards clinical antigen-specific immunomodulation. Curr. Opin. Pharmacol. 4, 403–407 (2004). 67. Wiczling, P., Rosenzweig, M., Vaickus, L. & Jusko, W. J. Pharmacokinetics and pharmacodynamics of a chimeric/humanized anti-CD3 monoclonal antibody, otelixizumab (TRX4), in subjects with psoriasis and with type 1 diabetes mellitus. J. Clin. Pharmacol. 23 Nov 2009 (doi:10.1177/0091270009349376). 68. Herold, K. C. et al. Activation of human T cells by FcR nonbinding anti-CD3 mAb, hOKT3γ1(Ala–Ala). J. Clin. Invest. 111, 409–418 (2003). 69. Bisikirska, B., Colgan, J., Luban, J., Bluestone, J. A. & Herold, K. C. TCR stimulation with modified anti-CD3 mAb expands CD8+ T cell population and induces CD8+ CD25+ Tregs. J. Clin. Invest. 115, 2904–2913 (2005). 70. Nelson, A. L. & Reichert, J. M. Development trends for therapeutic antibody fragments. Nature Biotechnol. 27, 331–337 (2009). 71. Labrijn, A. F., Aalberse, R. C. & Schuurman, J. When binding is enough: nonactivating antibody formats. Curr. Opin. Immunol. 20, 479–485 (2008). A comprehensive review of alternative strategies to generate antibodies that have minimized effector functions and that do not activate their targets. 72. Alegre, M. L. et al. A non-activating “humanized” anti- CD3 monoclonal antibody retains immunosuppressive properties in vivo. Transplantation 57, 1537–1543 (1994). 73. Woodle, E. S. et al. Phase I trial of a humanized, Fc receptor nonbinding OKT3 antibody, huOKT3γ1(Ala– Ala) in the treatment of acute renal allograft rejection. Transplantation 68, 608–616 (1999). 74. Bolt, S. et al. The generation of a humanized, non- mitogenic CD3 monoclonal antibody which retains in vitro immunosuppressive properties. Eur. J. Immunol. 23, 403–411 (1993). 75. Salfeld, J. G. Isotype selection in antibody engineering. Nature Biotechnol. 25, 1369–1372 (2007). 76. van der Neut Kolfschoten, M. et al. Anti-inflammatory activity of human IgG4 antibodies by dynamic Fab arm exchange. Science 317, 1554–1557 (2007). This article shows that IgG4 can exchange Fab arms in vivo to form bispecific antibodies, and it identifies mutations for preventing this exchange. 77. Jefferis, R. Antibody therapeutics: isotype and glycoform selection. Expert Opin. Biol. Ther. 7, 1401–1413 (2007). 78. Bruhns, P. et al. Specificity and affinity of human Fcγ receptors and their polymorphic variants for human IgG subclasses. Blood 113, 3716–3725 (2009). 79. Reddy, M. P. et al. Elimination of Fc receptor- dependent effector functions of a modified IgG4 monoclonal antibody to human CD4. J. Immunol. 164, 1925–1933 (2000). 80. Rother, R. P., Rollins, S. A., Mojcik, C. F., Brodsky, R. A. & Bell, L. Discovery and development of the complement inhibitor eculizumab for the treatment of paroxysmal nocturnal hemoglobinuria. Nature Biotechnol. 25, 1256–1264 (2007). 81. Davis, P. M., Abraham, R., Xu, L., Nadler, S. G. & Suchard, S. J. Abatacept binds to the Fc receptor CD64 but does not mediate complement-dependent cytotoxicity or antibody-dependent cellular cytotoxicity. J. Rheumatol. 34, 2204–2210 (2007). 82. Kabat, E. A., Wu, T. T., Perry, H. M., Gottesman, K. S. & Foeller, C. Sequences of Proteins of Immunological Interest 5th edn (US National Institutes of Health, Bethesda, 1991). 83. Choy, E. H. et al. Efficacy of a novel PEGylated humanized anti-TNF fragment (CDP870) in patients with rheumatoid arthritis: a phase II double-blinded, randomized, dose-escalating trial. Rheumatol. (Oxford) 41, 1133–1137 (2002). 84. Teeling, J. L. et al. Characterization of new human CD20 monoclonal antibodies with potent cytolytic activity against non-Hodgkin lymphomas. Blood 104, 1793–1800 (2004). 85. Shields, R. L. et al. High resolution mapping of the binding site on human IgG1 for FcγRI, FcγRII, FcγRIII, and FcRn and design of IgG1 variants with improved binding to the FcγR. J. Biol. Chem. 276, 6591–6604 (2001). A detailed mutational mapping of human IgG1 Fc for FcγRs and FcRn. Fc variants described include ones that improve binding to FcγRIIIA and enhance ADCC. 86. Stavenhagen, J. B. et al. Enhancing the potency of therapeutic monoclonal antibodies via Fc optimization. Adv. Enzyme Regul. 48, 152–164 (2008). 87. Lazar, G. A. et al. Engineered antibody Fc variants with enhanced effector function. Proc. Natl Acad. Sci. USA 103, 4005–4010 (2006). The paper shows a broadly applicable Fc protein engineering strategy, used to create variants of several approved therapeutic antibodies with ~100-fold more potent ADCC properties. 88. Richards, J. O. et al. Optimization of antibody binding to FcγRIIa enhances macrophage phagocytosis of tumor cells. Mol. Cancer Ther. 7, 2517–2527 (2008). 89. Jung, S. T. et al. Aglycosylated IgG variants expressed in bacteria that selectively bind FcγRI potentiate tumor cell killing by monocyte-dendritic cells. Proc. Natl Acad. Sci. USA 107, 604–609 (2010). 90. Jefferis, R. Glycosylation as a strategy to improve antibody-based therapeutics. Nature Rev. Drug Discov. 8, 226–234 (2009). 91. Umaña, P., Jean-Mairet, J., Moudry, R., Amstutz, H. & Bailey, J. E. Engineered glycoforms of an antineuroblastoma IgG1 with optimized antibody- dependent cellular cytotoxic activity. Nature Biotechnol. 17, 176–180 (1999). This is the first example of the alteration of the glycosylation of an Fc to enhance ADCC activity of IgG. 92. Shields, R. L. et al. Lack of fucose on human IgG1 N.-linked oligosaccharide improves binding to human FcγRIII and antibody-dependent cellular toxicity. J. Biol. Chem. 277, 26733–26740 (2002). 93. Shinkawa, T. et al. The absence of fucose but not the presence of galactose or bisecting N-acetylglucosamine of human IgG1 complex-type oligosaccharides shows the critical role of enhancing antibody-dependent cellular cytotoxicity. J. Biol. Chem. 278, 3466–3473 (2003). A detailed analysis of the influence of Fc glycans on the ability of a humanized antibody to support ADCC, showing that the absence of fucose has the most important role in enhancing ADCC. 94. Yamane-Ohnuki, N. et al. Establishment of FUT8 knockout Chinese hamster ovary cells: an ideal host cell line for producing completely defucosylated antibodies with enhanced antibody-dependent cellular cytotoxicity. Biotechnol. Bioeng. 87, 614–622 (2004). 95. Iida, S. et al. Nonfucosylated therapeutic IgG1 antibody can evade the inhibitory effect of serum immunoglobulin G on antibody-dependent cellular cytotoxicity through its high binding to FcγRIIIa. Clin. Cancer Res. 12, 2879–2887 (2006). This paper shows a broadly applicable Fc glyco-engineering strategy used to create variants of rituximab and trastuzumab with ~100-fold more potent ADCC activity. Non-fucosylated IgG1, unlike fucosylated counterparts, largely evade the inhibitory effect of plasma IgG on ADCC. 96. Li, H. et al. Optimization of humanized IgGs in glycoengineered Pichia pastoris. Nature Biotechnol. 24, 210–215 (2006). 97. Idusogie, E. E. et al. Mapping of the C1q binding site on rituxan, a chimeric antibody with a human IgG1 Fc. J. Immunol. 164, 4178–4184 (2000). 98. Idusogie, E. E. et al. Engineered antibodies with increased activity to recruit complement. J. Immunol. 166, 2571–2575 (2001). 99. Dall’Acqua, W. F., Cook, K. E., Damschroder, M. M., Woods, R. M. & Wu, H. Modulation of the effector functions of a human IgG1 through engineering of its hinge region. J. Immunol. 177, 1129–1138 (2006). 100. Natsume, A. et al. Engineered antibodies of IgG1/IgG3 mixed isotype with enhanced cytotoxic activities. Cancer Res. 68, 3863–3872 (2008). This article describes a potent enhancement of CDC activity of IgG using a IgG1–IgG3 hybrid isotype. REVIEWs NATURE REviEWS | Immunology volUME 10 | MAy 2010 | 315 focus on THERAPEuTIc AnTIBoDIEs © 20 Macmillan Publishers Limited. All rights reserved 10
