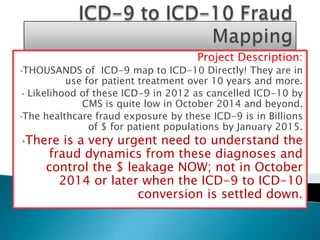
ICD-9 to ICD-10 Fraud Risk Assessment and Analytics Project
- 1. Project Description: •THOUSANDS of ICD-9 map to ICD-10 Directly! They are in use for patient treatment over 10 years and more. • Likelihood of these ICD-9 in 2012 as cancelled ICD-10 by CMS is quite low in October 2014 and beyond. •The healthcare fraud exposure by these ICD-9 is in Billions of $ for patient populations by January 2015. •There is a very urgent need to understand the fraud dynamics from these diagnoses and control the $ leakage NOW; not in October 2014 or later when the ICD-9 to ICD-10 conversion is settled down.
- 2. • •Some specialties such as ENT do not change much in the same patient for a given age. The procedures are not that expensive and hence conducive to fraud such as billing without services rendered and even overbilling that a payer notices too late! • Several stable diagnoses in Cardiology specialty is easy target for Billions $ upcoding and downcoding. • Furthermore, Specialty such as Pediatrics and OBGYN presents special challenge to Fraud •Detection. Advance analytics IS needed!!
- 3. •Mock up 300 lines of data from specialty such as ENT. •Apply Fraud Analytics Concept resulting in Fraud Conditions. •The Fraud Analytics Methods and Conditions will be used prospectively to monitor providers practice variations as well as utilize them as variables in Predictive Analytics.
- 4. •478.33 paralysis of vocal chords; bilateral partial •478.5 other diseases of vocal chord (abces, cellulitis, granuloma, leukoplakia, chronditis, singer's node) •478.74 stenosis of larynx •478.8 Upper respiratory tract hypersensitivity reaction, site unspecified •212.1 benign Neoplasm of respiratory and Intrthoracic Sinuses
- 5. ICD-9 code The ICD-10 conversion code 478.33 J38.Ø2 478.5 J38.3 478.74 J38.6 478.8 J39.3 212.1 D14.1
- 6. 400 350 10% 300 53% 250 Charge_$ Charge_$ Mean 200 +2 StdDev -2 StdDev 150 +3 StdDev -3 StdDev 100 50 0 1 3 5 7 9 11 13 15 17 19 21 23 25 27 29 31 33 35 37 39 41 43 45 47 49 51 Day Number
- 7. 350 300 0% C h 250 a 50% Charge_$ r 200 Mean g +2 StdDev 150 e -2 StdDev +3 StdDev 100 -3 StdDev $ 50 0 1 2 3 4 5 6 7 8 9 10111213141516171819202122232425262728293031323334353637 Day Number
- 8. Name: ENT_High_Low_biller. Metrics (or data inside this variable): - A. Total charge $ on two FWA Diagnoses/ total charge $ on all five diagnoses. B. Total charge $ on two FWA Diagnoses/ total charge $ on Three Non FWA diagnoses. C. Total number of claim lines on two FWA Diagnoses/ total claim lines on all five diagnoses.
- 9. Variable Name= ENT_High_Low_biller_A=0.46. ENT_High_Low_biller_B=0.85. ENT_High_Low_biller_C= 0.44 Conclusion: assuming that the suspected provider is in the network, 44% of the suspected diagnoses lines yielded 46% of the revenue from those two Dx for this provider. This provider likes to bill towards maximum contract charge $ on those two suspected Diagnoses regardless of patient gender and age (.46/.44=1.05). A Medicaid payer needs to stop this Now! Do not take a chance that CMS will delete them in October 2014. Even if CMS deletes all those thousands of codes (very unlikely to happen), BILLIONS will be lost by 1st January, 2015 (remember FWA is 300 Billion $ industry).
- 10. Six Sigma approach can’t stops bleeding in Millions of $ because one simple method can’t be Silver Bullet! However, Advance analytics such as Neural Network and Decision Tree needs to be applied to stop Billions $ Fraud because billing pattern is getting complicated every day. Remember that FWA phrase,” Where there are chronic patients present, Huge fraud is NEVER absent!!” There is a misconception that FWA and Disease Management are two different sides of Cost savings efforts; that it is doubling of efforts. It is NOT! I’ll show how Six Sigma and Advance Analytics FWA variables efficiently help reduce cost in Disease Management also.
- 11. Navin Kumar Sinha (2012). Double Check Consulting. 3744 Pennsylvania Ave, Apt 18, Fremont, CA 94536. Phone: 952-905-6636. MS: Statistical Genetics: Urbana-Champaign, IL. MBA: Utah State University (Decision Sciences). Experience of saving $50 million by conservative estimates in Healthcare Industry for Branded Companies all over USA.
