Dental ceramics seminar
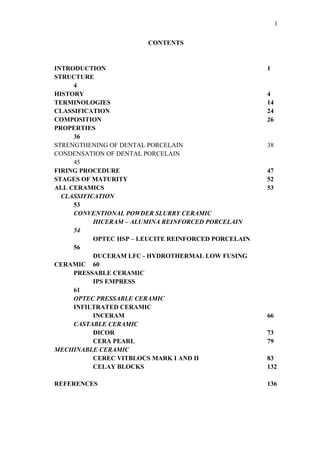
- 1. CONTENTS INTRODUCTION 1 STRUCTURE 4 HISTORY 4 TERMINOLOGIES 14 CLASSIFICATION 24 COMPOSITION 26 PROPERTIES 36 STRENGTHENING OF DENTAL PORCELAIN 38 CONDENSATION OF DENTAL PORCELAIN 45 FIRING PROCEDURE 47 STAGES OF MATURITY 52 ALL CERAMICS 53 CLASSIFICATION 53 CONVENTIONAL POWDER SLURRY CERAMIC HICERAM – ALUMINA REINFORCED PORCELAIN 54 OPTEC HSP – LEUCITE REINFORCED PORCELAIN 56 DUCERAM LFC - HYDROTHERMAL LOW FUSING CERAMIC 60 PRESSABLE CERAMIC IPS EMPRESS 61 OPTEC PRESSABLE CERAMIC INFILTRATED CERAMIC INCERAM 66 CASTABLE CERAMIC DICOR 73 CERA PEARL 79 MECHINABLE CERAMIC CEREC VITBLOCS MARK I AND II 83 CELAY BLOCKS 132 REFERENCES 136 1
- 2. INTRODUCTION Man has been obsessed with duplicating, restoring and replacing various lost body parts like the limbs, ear, nose and eyes with artificial prosthesis and teeth being no exception. Restoration of teeth is not recent but ancient, dating back to 1st century Roman B.C. Many materials have been used to restore and replace a lost teeth or a part of it, of these ivory was popular but not without its disadvantages.The quest for an artificial prosthesis similar to the nature tooth, both in function and esthetics, in the oral environment still remains as a foremost concern to the dentist, which has led to the use of CERAMICS in dentistry. CERAMICS Ceramics are defined as man-made solid objects formed by nonmetallic and inorganic raw materials that are baked at high temperatures. Stoneware and pottery are still made from impure clays, sand and feldspar minerals, and are baked in kiln,s First pulvering the raw materials into a fine powder and then adding water to obtain a working consistency for shaping and molding makes these objects. The unbaked objects dried and placed in a kiln and heating to sufficiently high temperatures to make the individual particles coalesce into a solid mass. Ceramics are nonmetallic, inorganic materials that contain metal oxides whose structure is crystalline, displaying a regular periodic arrangement of the component atoms and may exhibit ionic or covalent bonding. Also a low-fusing glass matrix filled with high-fusing filler. It is heated above the fusing temperature of the low- fusing glass but well below the temperature needed to fuse the high-fusing filler. The filler, as in composite resins, improves strength and esthetics. Glasses are described as supercooled liquids, not structureless or truly amorphous like a gas. In liquids, structural units or arrangements of atoms exist as they do in crystalline solids, but these units are not arranged in a regular manner. Glasses and liquids differ in one respect – in a glass, each atom has permanent neighbours at a farily definite distance while in a liquid the neighbours about any atom are continually changing. Glass is an inorganic product of fusion, which has cooled to a rigid condition without crystallization. Common glass is made of silica sand, sodium oxide and potassium oxide, and by adding aluminium oxide a plate glass is made. If silica is heated to 1000o C and then gradually increased in temperature to 1500o C over the course of hours it changes into cristobalite. Tridymatie is an impurity of cristobalite and is formed when the quartz is heated between 870-1470o C. Enamels are closely connected to the glass industry as they may be compared to fusible glass made opaque by adding opacifiers. Porcelain is a type of ceramic. All porcelains are ceramics but all ceramic are not porcelains. The traditional porcelain is composed of three naturally occurring minerals: pure white clay (kaolin), silica (quartz), and feldspar. After baking it is known as whiteware because of its color from the clay. The basic components of 2
- 3. dental porcelain are silica and feldspar. Additional components are aluminium oxide as well as pigments and opacifying agents, depending on the application.Ceramics, industrial porcelains and dental porcelains are fabricated from the same compounds, it is merely the concentrations of the various components that differentiate them. STRUCTURE 0 0 0 Si 0 Si 0 0 0 HISTORY OF CERAMIC Aesthetics and durability of material in the oral environment has always been a foremost concern to the dentist and is still a foremost concern to the dentist.The desire for a durable and aesthetic material is ancient although dental technology existed in Etrutia as early as 700 B.C. and during the Roman 1st Century BC. Little progress took place in dental art from the beginning of the Christian era to about 1500 AD. This was described as the dark ages of physical activities, a probably there was much activity, creative though and invention, but records were either not kept or later destroyed. Artificial teeth were made from 1. Animal products such as ivory teeth or bone These were unsatisfactory because they tend to deteriorate and disintegrate in the mouth and absorb stains and odour. AMBROISE PARE (1562) is credited for having prepared artificial teeth from bone and ivory. JACQUES GUILLENMEAU was a pupil of PARE, who prepared a substance by fusing certain waxes, gums, ground mastic, powdered pearl and white coral. This may have been the forerunner, in principle of esthetic fused porcelains, which appeared many years later. 2. Teeth taken from the mouth of dead persons The disadvantage were, • Expensive • Scared people • Developed a natural repugnance to put a corpse’s teeth into their mouth. • Repeated failures • Risk of transmitting diseases like syphilis 3. Bamboo The disadvantages of bamboo are esthetically poor and functionally not durable in the oral environment. 3
- 4. 4. Mineral tooth or Porcelain tooth CERAMICS originally referred to the art of fabricating of pottery. The term ceramic is derived from the Greek term “KERAMOS”, which means “A POTTER OR POTTERY”. It is believed that this word is realized to a Sanksrit term meaning “BURNED EARTH”, since the basic components were clays from the earth, which were heated to form pottery (FRIEDMANN 1991). Ceramic is a non-metallic, inorganic material. The term “CERAMIC” applies to a wide variety of materials, including metal oxides, borides, carbides, nitrides and complex mixture of these materials. Ceramic objects have been constructed for thousands of years. The earliest techniques used were crude. It consisted of shaping the item in clay/soil and then baking it to fuse the particles together, which resulted in coarse and porous products such as goblets and other forms of potter. 21,000 BC; earliest man-made ceramic artifacts were dated. 5000 BC: clay pots were discovered. Later development led to detailed stoneware items 100 BC: colored, glazed vessel made (Han Dynasty) 600 BC: translucent porcelain made (Tang Dynasty) Egyptian faieces are the first to enamel a substructure with a ceramic venner. Their typical blue green hues resulted form metal oxides created during the firing process. More recently the Chinese ceramist developed porcelain. Vitrification, translucency, hardness and impermeability characterized it. In the 17th century, the Europeans attempted to develop porcelain of similar quality that of the Chines. By 1720’s the Europeans mastered the art of manufacturing fine translucent porcelain. This lead to the promulgation of information regarding the fundamental components of porcelain: KAOLIN and FELDSPAR. In 1723, enameling of metal denture bases was described by PIERRE FAUCHARD, which initiated research in porcelain that imitates color of the teethand gingival tissue. By 1774, a Parisian apothecary ALEXIS DUCHATEAU with the assistance of a Parisian dentist NICHOLAS DUBOIS de CHEMENT made the first successful porcelain dentures at the GUERCHAND PORCELAIN FACTORY, replacing the stained and malodours ivory processes. NICHOLAS DUBOIS worked diligently at perfecting the invention (a very difficult achievement because the one-piece denture had to resist distortion during firing). In course of his experiments, DUBOIS continuously improved his porcelain formulation and was awarded both French and English patent. He termed them “UNCORRUPTIBLE TEETH” that gained wide currency and for many years was synonymous with porcelain teeth. In 1817, a French immigrant dentist, ANTOINE PLANTON introduced individual porcelain teeth in America. In 1837, CLAUDIUS ASH produced fine porcelain teeth and later went on to introduce “TUBE TEETH” which could be inserted over a post on a denture. It became widely accepted for use in bridges as well as in full dentures. 4
- 5. In 1851, JOHN ALLEN of Cincinnati patented “CONTINUOUS GUM TEETH” prosthesis consisting of two to three porcelain teeth fused to a small block of porcelain colored like gingiva. The search for suitable tooth colored filling material continued and was led by the prominent artist-dentist ADELBERT.J.VOLCK who brought about somewhat unsatisfactory products as early as 1857. The modern synthetic porcelain or silicate cements-porcelain inlays fashioned to fit prepared cavities precisely were marketed first in 1880. In 1882, glass inlays (not porcelain) was introduced by HERLRST. In 1885 LOGAN fused porcelain to platinum post thus resolving the retention problem. He termed them as “RICHMOND CROWN”. These crowns represent the first innovative use of metal ceramic system. The first ceramic crowns and inlays were made by C.H.LAND in 1886. He fused feldspathic porcelain to burnished platinum foil (used as a substructure) with high controlled heat of a gas furnace. Improvement in translucency and color of dental porcelains were realized through developments that ranged from the formulation of ELIAS WILDMENA in 1838 to introduction of vacuum firing in 1949. The popularity of ceramic restoration declined with the introduction of acrylic resin into dentistry till 1940’s after which its popularity increased as the disadvantage of acrylic resin were realized. Vacuum firing of ceramics resulted in denser and more translucent restorations than the air fired restorations. In 1950’s and early 1960’s dental porcelains were developed with high coefficient of thermal expansion, which allowed compatibility with dental casting alloys. This enabled the fabrication of porcelain fused to metal restorations. Refinements in the mental ceramics systems dominated dental ceramic research during the past 35 years that resulted in improved alloys, porcelain metal bonding and porcelains. All porcelain crown systems, despite its aesthetic advantage failed to gain widespread popularity because the chief disadvantage of early restorations was their low strength. This resulted in the usage of ceramic restorations in low stress situations such as anterior teeth. But still fractures of restorations were very common, which resulted in the development of higher strength materials. The development of high strength ceramics followed 2 paths. The first approach was to use 2 ceramic materials to fabricate the restoration. A high strength but non- aesthetic core material is veneered with a lower strength aesthetic material. This approach is similar to the metal ceramic system, but its advantage over the metal ceramic system is that the ceramic core can be more easily masked than the metal substructure. The second approach is to develop a ceramic that combines good aesthetic with high strength. This technique has the additional advantage of not needing the additional thickness of material to make a high strength core. However at present the strongest ceramics are non-aesthetic ceramics. The popularity of all 5
- 6. ceramic systems increased after the introduction of alumina reinforced dental porcelain. Mc.LEAN and HUGHES in 1965 were the first to introduce high strength porcelain into dentistry. They advocated the introduction of glass-alumina composites. McLEAN used a relatively opaque inner core of high alumina content for maximum strength. This was surrounded by combination of body and enamel powder with respectively 15% and 5% alumina resulting in restoration that were 40% stronger than traditional feldspathic porcelain. The technique was further developed by improving the fabrication technique of alumina core. Here the porous alumina was fused with a specially formulated glass by a process called slip casting. This material was called INCERAM (1988) whose strength is about 3 to 4 times greater than earlier alumina core material. Thus these materials have been used in high stress FPD’s. Different oxides have been used to strengthen ceramics like magnesium and zirconium. The ceramics, which used MgO, were called INCERAM SPINELL, whose strength is less than INCERAM but its translucency is better. So used for anterior crowns. Zirconium oxides were the latest to be used to strengthen ceramics, which can be used in the case of posterior bridges. High strength aesthetic ceramics have been developed again using glass-ceramic composite microstructure for improving strength. In one system molten porcelain is cast into a refractory mold formed by traditional loss wax technique. These are Castable ceramics and are called DICOR porcelain. These are transparent after casting and must be subjected to a carefully controlled 11 hours firing sequence to promote the mica crystal growth that gives the restoration its strength. This was introduced in 1972. ‘Shrink free’ all ceramic crown systems were introduced in 1980’s Eg.CERESTORE (1983: Cerestore injection-molded core by Sozio and Riley). Manufacturers have introduced high strength ceramics using leucite [potassium aluminum silicate] crystals dispersed in glassy matrix. Leucite is precipitated from feldspar is incorporated in metal-ceramic porcelain formulation to increase the coefficient of thermal expansion of ceramics to match that of the metal substructure E.g. OPTEC HSP, CERIMATE and IPS EMPRESS. In 1989 Alceram a replacement for Cerestore was introduced. CAD/CAM [COMUTER AIDED DESIGNING / COMPUTER AIDED MANUFACTURING] has been introduced into dentistry as early as 1970 which has now revolutionized the designing and processing of all ceramic crowns and bridges by cutting down the time for impression making and processing of the ceramic crowns and bridges. E.g. CEREC 2, CEREC 3, CELAY, PROCERA (1993). TERMINOLOGY ALUMINA : The oxide of aluminum (A1O3) ALUMINA CORE : A ceramic containing sufficient crystalline alumina to achieve adequate strength and opacity when used for the production of a core for ceramic jacket crowns. 6
- 7. ALUMINOUS PORCELAIN : Glass strengthened by the addition of alumina. AMORPHOUS : Without definite form or shape; formless; without real or apparent crystalline form; uncrystallized. CAD-CAM: Computer-aided design combined with computer-aided machining. In dentistry, laser mapping of a cavity preparation can be fed to a computer-controlled milling machine. CERAMIC : Any of various heat resistant and corrosion resistant materials made by shaping then firing a nonmetallic metal, such as clay, at a high temperature; a compound of metallic and nonmetallic elements. CERAMIC, DENTAL: A compound of metals (aluminum, calcium, lithium, magnesium, potassium, sodium, tin, titanium and zirconium) and nonmetals (silicon, boron, fluorine and oxygen) that may be used as a single structural component as one of the several layers that are used in the fabrication of a ceramic-based restoration. CERAMIC JACKET CROWN : An all-ceramic crown without a supporting metal substrate that is made a ceramic with a substantial crystal content (>50 vol%) from which its higher strength and / or toughness is derived; distinguished from porcelain jacket crowns which are made with a lower strength core material, usually aluminous porcelain or feldspathic porcelain. CLAY :A native hydrated aluminum silicate, produced by the decomposition of rocks due to weathered (A1203, SiO2. H2O); insoluble in water and organic solvents but absorbs water to form a plastic, moldable mass, water serving as a lubricant between the colloidal particles; a widely distributed colloidal lusterless earthy substance, plastic when moist but permanently hard when fired, that is composed primarily of decomposed igneous and metamorphic rocks rich in the mineral feldspar in the form of crystalline grains <0.002mm in diameter, whose essential constituents are kaolinite and other hydrous aluminous minerals. DISPERSION STRENGTHENING : A mechanism by which a crystalline phase of high strength and high modulus of elasticity is dispersed in an amorphous glassy matrix to produce a high strength composition. FELDSPAR : Any of a group of abundant rock-forming minerals occuring principally in igneous, plutonic and some metamorphic rocks and consisting of silicates of aluminum with potassium, sodium, calcium and rarely barium; X20, A12O3.SiO2 where X is either Na or K. FELDSPATHIC PORCELAIN :A ceramic composed of a glass matrix phase and one or more crystalline phase one of which is leucite (K20,A12O3, 4SiO2) which is used to create high-expansion porcelain that is thermally compatible with metal allow core substructures; a more technically correct name for this is leucite porcelain because feldspar is not present in the final processed porcelain nor is it necessary as a raw material to produce leucite crystals. FLUX : (Latin fluere – to flow) a substance used to promote fusion especially of metals or minerals; a substance (as rosin or borax) applied to surface to be joined by soldering, brazing or welding just prior to or during the operation to clean and free them from oxide and promote their union; a substance (as borax) added in glassmaking for promoting vitrification. 7
- 8. FRIT : Materials of which glass is made after having been calcified or partly fused in a furnace but before vitrification; glass variously compounded that is quenched and ground as a basis for glazes or enamels; powdered glass; ceramic melt in which a glass is formed. GLASS :Any of a large class of materials with highly variable mechanical and optical properties that solidify from the molten state without crystallization, that are typically based on silicon dioxide, boric dioxide, aluminum oxide or phosphorous pent oxide, that are generally transparent or translucent and that are regarded physically as super- cooled liquids rather than true solids. An amorphous inorganic usually transparent or translucent substance consisting typically of a mixture of silicates or borates or phosphates formed by fusion of sand or some other form of silica or by fusion of oxides of boron or phosphorous with a flux (soda, potash) and a stabilizer (lime, alumina) and sometimes metallic oxides for coloring; a non-crystalline brittle solid. GLASS-CERAMIC : A solid consisting of a glassy matrix and one or more crystal phases produced by the controlled nucleation and growth of crystals in the glass. GLASS-INFILTRATED DENTAL CERAMIC : A minimally sintered A1203 or MgA12O4 core with a void network that has been sealed by the capillary flow of molten glass; In-CERAM (A12O3) and IN-CERAM Spinell (MgA12O4) core. INJECTION –MOLDED CERAMIC : A glass or other ceramic material that is used to form the ceramic core by heating and compressing a heating ceramic into a mold under pressure; IPS Empress. KAOLIN : Fine clay used in ceramics and refractories and as a filter or coating for paper and textiles. KAOLINITE :A mineral, the principle constituent of kaolin, A12O3, 2SiO2.2H2O. LEUCITE : White or gray mineral, KA1Si2O6, consisting of potassium aluminum silicate occuring in igneous rocks with a glassy fracture. MICA : Any of a group of chemically and physically related mineral silicate, common in igneous and metamorphic rock each containing hydroxyl, alkali and aluminum silicate groups. OPACIFIER : A white or pale cream-colored oxide, which is used to decrease translucency and act as a masking agent, often, tin oxide or titanium dioxide. PORCELAIN :A hard, white, translucent ceramic made by firing a pure clay and then glazing with variously colored fusible materials; china; a white, ceramic- containing glass with a glazed surface; ceramic containing minerals held together with glass. PORCELAIN JACKET CROWN : One of the first all-ceramic crowns, made from a low strength aluminous core material and veneering porcelain usually utilizes a thin platinum foil substructure. POTASH : K2CO3 [potassium carbonate]; K2 (OH) [potassium hydroxide]; any of several compounds containing potassium, especially soluble compounds, such as K20 [potassium oxide], KC1 [potassium chloride] and various potassium sulfates. POTASH FELDSPAR : Orthoclase. QUARTZ : A mineral, SiO2 consisting of a silicon dioxide that next to feldspar is the commonest mineral. 8
- 9. REFRACTORY : Capable of enduring or resisting high temperatures. SAND : Consisting mostly of quartz commonly used for making mortar and glass. SILICA : Chemically resistant dioxide, SiO2, of silicon that occurs naturally in the 3 crystalline modifications of quartz, tridymite and cristobalite, in amorphous and hydrated forms (as opal) and in less pure forms (sand, diatomite, tripoli) and combined in silicates that can be prepared artificially as a fine powder water glass or other soluble silicates and also in colloidal form, and that is used primarily in making glass, ceramics and refractories, in producing elemental silicon, its alloys and compounds. SILICATE : Any of numerous insoluble often complex metal salts containing silicon and oxygen in the anion, that constitute the largest group of minerals and with quartz make up the greater part of the earth’s crust. SINTER : To cause to become a coherent mass by heating without melting: although there is not a fusion of the porcelain powder particles, they join together by flow on contact as a result of surface energy; densification by partial fusion. SLIP-CAST SLURRY : A fine particle ceramic dispersed in an aqueous liquid medium is poured into a porous mould, which rapidly extracts the liquid causing the formation of a close-packed but weak ceramic particle structure. SODA : Any of various forms of sodium carbonate; chemically combined sodium. SPINEL : Any of several hard, white, orange, red, green, blue, or black minerals with composition MgA12O4. SWAGE : Shape to the form of a model, cast or die by compressive strength (porcelain teeth soldered to gold plates swaged to fit the mouth). VITRIFICATION : (Latin vitrum –glass) to change into glass or a glassy substance by heat and fusion. CLASSIFICATION ACCORDING TO TYPE 1. Feldspathic porcelain 2. Aluminous porcelain 3. Glass infiltrated aluminous 4. Glass infiltrated spinell 5. Glass ceramics ACCORDING TO USE 1. Ceramic for artificial teeth 2. Jacket crown, inlay and onlay ceramic 3. Metal ceramic 4. Anterior bridge ceramic ACCORDING TO PROCESSING TECHNIQUE 1. Sintered porcelain 2. Castable porcelain 3. Machined porcelain 4. Infiltrated porcelain 5. Pressed porcelain 9
- 10. 6. ACCORDING TO FIRING TECHNIQUE 1. Air fired (at atmospheric pressure) 2. Vacuum fired (at reduced pressure) 3. Diffusible gas firing ACCORDING TO FIRING TEMPERATURE 1. High fusing - >1300 C 2. Medium fusing - 1101 t0 1300C 3. Low fusing - 850-1101C 4. Ultra low fusing - <850C ACCORDING TO SUBSTRATE MATERIAL 1. Cast metal 2. Sintered metal 3. Swaged metal 4. Glass ionomer 5. CAD/CAM. COMPOSITION Dental porcelains, to a large extent, are glassy materials. Glasses are super-cooled liquids / non-crystalline solids with only a short-range order in their atomic arrangement. During cooling, molten glass solidifies with a liquid structure instead of a crystalline structure. Such a structure is called vitreous and the process of forming it is known as vitrification. The principal anion present in all glasses is O2 ion, which forms very stable bonds with small multivalent cations such as silicon, boron, phosphorous etc. (e.g.,. in silicon glasses, SiO4 tetrahedra are formed which are responsible for the random network of glass). These ions are termed as glass formers. For dental applications, only two glass forming oxides – silicon oxide and boron oxide are used to develop the principal network. Additional properties like low fusion temperature, high viscosity, color and resistance to devitrification is obtained by the addition of other oxides like potassium, sodium, calcium, boron or aluminum oxides to the glass forming lattice, SiO4. HIGH FUSING PORCELAINS FELDSPAR Traditionally, the basic ingredients of these types of porcelains are feldspar kaolin (clay) and quartz. Feldspar is the primary constituent, and all porcelains based on feldspar are referred to as feldspathic porcelains. Natural feldspars can be either sodium feldspar (albite) or potassium feldspar (orthoclase / microline) which are minerals composed of potash (K2O), Soda (Na2O) Alumina (Al2O3) and silica (SiO2). For dental purposes, light potassium based feldspar is generally selected because of its increased resistance to pryoplastic flow and an increased viscosity. The pyroplastic flow of dental porcelain should be low in order to prevent rounding of margins, loss of tooth from and obliteration of surface markings. Feldspars are present in concentrations of 75 to 85% and undergo incongruent melting at temperatures between 1150°C and 1530°C. Incongruent melting is the process by which one material melts to form a liquid plus a different crystalline material. Hence a glassy phase is formed and suspended inside it are crystalline potassium alumino silicate crystals known as leucite. 10
- 11. KAOLIN / CLAY Kaolin / clay (Al2O3, 2SiO2, 2H2O) serves as a binder. When mixed with water, it forms a sticky mass, which allows the unfired porcelain to be easily worked and molded. On heating, it reacts limitedly with feldspar (known as pyrochemical reaction) and thereby provides rigidly. It also adheres to the framework of quartz particles and shrinks considerably during firing. Unfortunately, pure kaolin is white in color and reduces the translucency of porcelain. Consequently, it is included only in small concentrations of 4 to 5%. PURE QUARTZ Pure quartz is used porcelain as a strengthener. The main function of quartz (silica) is to impart more strength and firmness, and a greater translucency. Silica remains uncharged at the usual firing temperatures and hence contributes stability to the mass during heating by providing a framework for other constituents. It is present in concentrations of 13 to 14%. Traces of iron may be present as impurities in the quartz and must be removed to prevent discoloration of porcelain. MEDIUM, LOW AN ULTRA LOW FUSING PORCELAINS The low and medium fusing porcelain powders are glass which have been ground from blocks of matured porcelain. For this, the raw ingredients are mixed and fused, and the fused mass is the quenched in water. The rapid cooling induces stresses in the glass to the extent that considerable cracks and fractures occur. This process is referred to as fritting and the product so obtained is called a frit. The brittle material is then ground to a fine powder of almost colloidal dimensions. During subsequent firing, little or no pyrochemical reaction occurs, but the glass phase softens and flows slightly. This softening allows the powder particles to coalesce together (sintering) and form a dense solid. However, the temperature must be controlled to minimize the pyroplastic flow. The raw ingredients for the low and medium fusing porcelains are basically the same as for the high fusing porcelain powders but in addition contain balancing oxides / fluxes. These additions tend to modify the properties by interrupting the glass network and hence are also known as glass modifiers. GLASS MODIFIERS These acts as fluxes and help in reducing the softening temperature of glass by decreasing the amount of cross-linking between the oxygen and the glass forming elements like silica i.e., they disrupt the continuity of the SiO4 network. E.g., if Na2O is added, the sodium ions break the bridging Si-O-Si bond leaving behind two non- bridging oxygen’s. The modifier concentration should not be too high, because if too many tetrahedra are disrupted, there may occur crystallization during the porcelain firing operations. The most commonly used glass modifiers are potassium, sodium and calcium oxides. These are introduced as carbonates that revert to oxides on heating. Other oxides added may be lithium oxide, magnesium oxide, phosphorous pentoxide etc. 0 0 11
- 12. 0 Si 0 Si 0 + Na2O 0 0 0 0 0 Si • • Si 0 + 2Na+ 0 0 Diagram showing interruption of silica tetrahedral by sodium oxide. INTERMEDIATE OXIDES The addition of glass modifiers not only lowers the softening temperature but also reduces the viscosity of the glass. A less viscous porcelain would have a lower resistance to slump or pyroplastic flow and it is therefore necessary to produce glasses with low firing temperatures and a high viscosity. This can be achieved by using intermediate oxides lie aluminum oxide (Al2O3), which cannot actually form a glass but can take part in the glass network. BORIC OXIDE Boric oxide (B2O3) serves as a glass modifier as well as a glass former. The amorphous matrix of B2O3 is formed by the three dimensional arrangement of BO3 triangles. Because the bonds extend in only three directions compared to four in SiO4 the stability of boric oxide is weaker i.e., glass formed of boric oxide has a comparatively lower melting point, less viscosity and a higher expansion. When B2O3 is added to silica glass, the amorphous network consists of a continuous arrangement of SiO4 tetrahedra and BO3 triangles. Inspite of the continuous lattice arrangement, the softening point of glass is lowered because of the interruption of the more rigid and stable SiO4 network by the BO3 lattice. A typical low fusing porcelain can be shown to have the following composition. Composition of typical low fusing porcelain Low fusing porcelain Oxide Weight percent Glass Formers SiO2 B2O3 69.36 7.53 Glass Modifiers CaO K2O NaO 1.85 8.33 4.81 Intermediate oxides Al2O3 8.11 12
- 13. OPACIFYING AND COLORING DENTAL PORCELAIN The translucency of dental porcelain depends on whether a single-phase glass or mixture of glasses is used. If a single-phase glass frit is employed in which all of the constituents are completely taken into solution, the resultant product is highly transparent. In case of fluxed feldspathic porcelains, the degree of fusion and pyro- chemical reactions are limited to an extent such that some crystalline feldspar remains un-dissolved in the glassy matrix. This difference in refractory indices of the crystal and glass produces porcelain with opalescent or grayish blue translucency. Another method of developing translucent gray or opalescent characteristics in porcelain is the use of a mixture of two or more single phase glass frits of slightly different refractive indices.The translucency of porcelain can be further decreased by using an opacifying agent. An opacifying agent is generally a metal oxide-ground to a very fine particle size of <5µm. Zircomium oxide is the most common opacifier employed and is usually incorporated into the concentrated color frit to be later added to the unfired porcelain. The difference between the refractive indices of the glass and the opacifier is the basic mechanism behind opalescence. Different wavelength of visible light are scattered differently by the opacifying particles. This effect depends upon the size as well as the volume distribution of the particles. Particles in the size range 0.4 to 0.8 µm generate a blue tinge in reflecting light and turn yellowish red in transmitted light. Preferably, the size of the particle should be nearly the same as the wavelength of visible light. Dentin porcelains are more opaque compared to enamel porcelains. COLOURING AGENTS Pigmenting or coloring oxides are added to obtain various shades needed to simulate natural teeth. These pigments, generally metal oxides, are added to the glass used for porcelain manufacture and then subjected to the fritting process. The frit so obtained is highly color concentrated. These colored glasses are then finely ground and blended with the un-pigmented porcelain powder to obtain the proper hue and chroma. The different colouring pigments used in dental porcelain are given in the table below. Different coloring pigments used in dental porcelain Ferric oxide (black), platinum gray Gray Chromium oxide, Copper oxide Green Cobalt Salts Blue Ferrous oxide, Nickel oxide Brown Titanium oxide Yellowish brown Manganese oxide Lavender Chromium-tin, Chromium-alumina Pink Indium Yellow / Ivory STAINS AND COLOR MODIFIERS Stains are generally low fusing colored porcelains used to imitate markings like enamel check lines, calcification spots, fluoresced areas etc. Stains in finely powdered form are mixed with water or glycerine and water or any other special liquid. The wet mix is applied with a brush either on to the surface of porcelain 13
- 14. before glazing, or built into the porcelain (internal staining). Internal staining is preferable as it gives more life like results and also prevents direct damage to the stains by the surrounding chemical environment. Color modifiers on the other hand are less concentrated than stains and are used to obtain gingival effects or highlight body colours, and are best used at the same temperature as the dental porcelain. GLAZES AND ADD-ON PORCELAIN Glazing is done so as to produce enamel like luster after occlusal and morphologic corrections have been made in a porcelain restoration. It also seals pores on the surface of a fired porcelain. The removal or reduction in the size and number of these surface flaws after glazing markedly increases the strength of porcelain by preventing crack propagation. It has been seen that if the glaze is removed by grinding, transverse strength may be only half that of glazed porcelain. Glazing can be of two types: self glazing (autoglazing) and add-on glazing. In the self-glazing procedure, an external glaze layer is not applied but the completed restoration itself is subjected to glazing. Whereas in the add-on glazing, an external glaze layer is applied on the surface. Add-on glazes are uncolored glasses whose fusing temperature have been lowered by the addition of glass modifiers. The thermal expansion of an add-on glaze is also fractionally lower than the ceramic body to which it is applied. This places the glazed layer under compression and hence crazing or peeling of the surface is avoided. Disadvantages of add-on glazes are its low chemical durability, difficult to apply evenly and almost impossible to attain a detailed surface characterization. Too high temperatures or prolonged glazing could result in increased pyroplastic flow of the material and hence roundening off of the line angles and loss of surface characteristics. Also, an over glazed surface appears glassy and takes on the greenish hue of a natural glass thereby defying the natural enamel look. Add-on porcelains are generally similar to glaze porcelains except for the addition of opacifiers and color pigments. Add-on porcelains should exclusively be used for simple corrections of tooth contour or contact points. PROPERTIES Compressive strength - 50,000 psi Tensile strength - 5,000 psi Shear strength - 16,000 psi Elastic modulus - 10X106 psi Linear coefficient of thermal expansion - 12X10-6 / °C Specific gravity - 2.2 to 2.3 Liner shrinkage - High fusing - 11.5% Low fusing - 14.0% Refractive index - 1.52 to 1.54 The compressive strength is quite high compare to tensile or shear strength. 1. The tensile strength is low because of the unavoidable surface defects. 2. The shear strength is low because of lack of ductility in the material. 3. Voids and blebs greatly reduce the strength of porcelain. 4. Blebs are internal voids tend to reduce the specific gravity of porcelain. 14
- 15. 5. Porcelains extremely hard materials and because of this property offer considerable resistance to abrasion. This could be a disadvantage in that it causes excessive wear of the opposing natural tooth structure or the restorative material. 6. The brittleness → 0.1% deformation is sufficient to fracture porcelain before fracture. 7. Uranium oxide / cerium oxide is added to match the fluorescence of porcelain to that of the natural tooth. 8. Porcelain: a. Relatively inert. b. Chemically stable. c. Corrosion resistant. d. Highly biocompatible. e. Conducive to gingival health – as it prevents plaque addition. f. Solubility is less. TWO FACTORS AFFECTING THE PROPERTIES 1. Manner and degree of condensation / compaction of power. 2. Degree of firing and procedure followed to fuse mass. STRENGTHENING DENTAL PORCELAIN METHODS 1. Development of residual compressive stresses 2. Interruption of crack propagation DEVELOPMENT OF RESIDUAL COMPRESSIVE STRESSES: The propagation of cracks from surface flaws is responsible for the poor mechanical behaviour of ceramics in tention, although it is also possible that flaws within the interior of the material can also cause fracture initiation under certain conditions. One widely used method of strengthening glasses and ceramics is the introduction of residual compressive stresses within the surface of the object. Strengthening is gained by virtue of the face that these residual stresses must first be negated by developing tensile stresses before any net tensile stress develops. For example, if the net compressive stress within a surface of ceramic is 60 Mpa, it would take a total induced tensile stress of + 100 Mpa in this region to cause a fracture of the material. Consider two strips of ceramic A, one that was subjected to a treatment that introduced a residual compressive stress of – 100 Mpa into its surface and the other that was not treated. As the two strips are flexed equal amounts, the untreated strip develops tensile in its convex surface, whereas the treated strip merely experiences a decrease in the residual compressive stress. When the tensile stress in the untreated strip reaches + 60 Mpa, for example, the untreated strip fracture but the treated strip has a residual compressive stress of – 49 Mpa remaining within its surface. If the untreated strip breaks at 60 Mpa, the treated strip subjected to the same force will still have – 40 Mpa of residual compressive stress remaining. It would take an additional applied tensile stress of + 10 Mpa to bring the surface tensile of the 15
- 16. treated strip to +60 Mpa. This increase in applied tensile stress from 60 to 160 Mpa represents a 200% increase in strength over the untreated strip. There are several techniques for introducing these residuals compressive stresses into the surfaces of ceramic articles. Three of these methods are discussed below. Ion Exchange: The technique of ion exchange sometimes called chemical temperaturing, is one of the more sophisticated and effective methods of introducing residual compressive stresses into the surfaces of ceramics. This process involves the exchange of larger potassium ions for the smaller sodium ions, a common constituent of a variety of glasses. If a sodium-containing glass article is placed in a bath of molten potassium nitrate, potassium ions in the bath exchange places with some of the sodium ions in the surface of the glass article. The potassium ion is about 35% larger than the sodium ion. The squeezing of the potassium ion into the place formerly occupied by the sodium ion creates large residual compressive stresses (roughly 700 Mpa 100,000 psi) in the surfaces of glasses subjected to this treatment. These residual compressive stresses produce a pronounced strengthening effect. However, this process is best used on the internal surface of a crown, veneer, or inlay because this surface is protected from grinding and exposure to acids. One study has shown that grinding of only 100 µm from an external surface reduces the strength of the treated structure to its original value. Furthermore, contact with acidulated phosphate fluoride over a cumulative time of 3 hours removes most of the ion-exchanged layer as well. Not all ceramics are amenable to ion exchange. For example, alumina core materials, DICOR glass-ceramic core material, and some conventional feldspathic porcelains that are highly enriched with potash feldspar (K2O, Al2O3.6SiO2) cannot be sufficiently ion exchanged with potassium to warrant this treatment. Thermal Tempering: Perhaps the most common method for strengthening glass is by thermal tempering. Thermal tempering creates residual surface compressive stress by rapidly cooling (quenching) the surface of the object while it is hot and in the softened (molten) state. This rapid cooling produces a skin of rigid glass surrounding a soft (molten) core. As the molten core solidifies, it tends to shrink, but the outer skin remains rigid. The pull of the solidifying molten core, as it shrinks, creates residual tensile stresses in the core and residual compressive stresses within the outer surface. For dental applications, it is more effective to quench hot glass-phase ceramics in silicone oil or other special liquids rather than using air jets that may not uniformly cool the surface. Thermal Compatibility : Most metals expand linearly with temperature up to the melting range. Thus, a metal expands approximately the same amount when heated from 50o C to 60o C as it does from 200o C to 210o C. Dental porcelains behave differently; they have different values in different temperatures ranges, and, as a result, the thermal expansion or contraction of the porcelain cannot be precisely matched to that of the allow. Instead, the thermal behaviour of the metal and porcelain must be adjusted by the manufacturer in such a way that during the cool-down and properly directed so that 16
- 17. the porcelain is not subject to immediate or delayed failure. Ideally, the porcelain should be under slight compression in the final restoration. This objective is accomplished by selecting an alloy that contracts slightly more than the porcelain on cooling to room temperature.Consider three layers of porcelain: the outer two of the same composition and thermal contraction coefficient and the middle layer of a different composition and a higher thermal contraction coefficient. Suppose that the layers are bonded together and the bonded structure is allowed to cool to room temperature. The inner layer has a higher coefficient of thermal contraction and thus contracts more as it cools. Hence, an cooling to room temperature, the inner layer produces compressive stresses in the outer layers as previously described for thermal tempering. This three-layer laminate technique is used by Corning Glass Works to manufacture their dinnerware.A similar rationale applies to porcelains and alloys for metal-ceramic restorations. The metal and porcelain should be selected with a slight mismatch in their thermal contraction coefficients (the metal thermal contraction coefficient is slightly larger), so that the metal contracts slightly more than the porcelain on cooling from the firing temperature to room temperature. This mismatch leaves the porcelain in residual compression and provides additional strength for the restoration. Disruption of Crack Propagation : A further, yet fundamentally different, method of strengthening glasses and ceramics is to reinforce them with a dispersed phase of a different material that is capable to hindering a crack from propagating through the material. There are two different types of dispersions used to interrupt crack propagation. One type relies on the toughness of the particle to absorb energy from the crack and deplete its driving force for propagation. The other relies on a crystal structural change under stress to absorb energy from the crack. These methods of strengthening are described later. Dispersion of a Crystalline Phase : When a tough, crystalline material such as alumina (Al2O3) in particulate form is added to a glass, the glass is toughened and strengthened because the crack cannot penetrate the alumina particles as easily as it can the glass. The technique has found application in dentistry in the development of aluminous porcelains (A12O3 particles in a glassy porcelain matrix) for PJCs. Another ceramic dental material that uses reinforcement of a glass by a dispersed crystalline substance is Dicor glass-ceramic. The cast glass crown is subjected to a heat treatment that causes micron-sized mica crystals to grow in the glass. When glass-ceramic restorations are subjected to high tensile stresses, these microscopic crystals will disrupt crack propagation, thereby strengthening the crown. In most instances, the use of a dispersed crystalline phase to disrupt crack propagation requires a close match between the thermal contraction coefficients of the crystalline material and the surrounding glass matrix. Transformation Toughening : A new technique for strengthening glasses involves the incorporation of a crystalline material that is capable of undergoing a change in crystal structure when placed under stress. The crystalline material usually used is termed partially stabilized zirconia (PSZ). The energy required for the transformation of PSZ is taken 17
- 18. from the energy that allows the crack to propagate. Experimental work has shown that transformation toughening may be a viable method for strengthening dental porcelains. One drawback of PSZ is that its index of refraction is much higher than that of surrounding glass matrix. As a result, the particles of PSZ scatter light as it passes through the bulk of the porcelain, and this scattering produces an opacifying effect that may not be aesthetic in most dental restorations. CONDENSATION OF DENTAL PORCELAIN Porcelain powder is mixed with a liquid binder so that the particles are held together, and the thick creamy paste can be worked and built to the desired shape. The process of bringing the particles closer and of removing the liquid binder is known as condensation. Distilled water is the liquid binder used most commonly. However, glycerine, propylene glycol or alcohol has also been tried. The liquid because of its surface tension property serves as the binder. During subsequent firing it is eliminated, and the porcelain particles fill the space formerly occupied by the binder thereby resulting in shrinkage. The aim of consideration is to pack the particles as close as possible in order to reduce the amount of porosity and shrinkage during firing. Two important factors, which determine the effectiveness of condensation, are the size and shape of the powder particles. If only one-size particles are used, even the greatest condensation is expected to leave a void space of 45 percent between the particles. With two sized particles, the void space is reduced to2 5 percent, and with three or more sized particles, the void space comes down to 22 percent. System that uses three sizes of powder is known as the gap grading system. In addition, the shape of the powder particles also governs the packing density. Round particles produce better packing compared with angular particles. The most important factor in condensation is the effect of surface tension. As the liquid is withdrawn, surface tension causes the powder particles to pack closely together. However, sufficient amount of liquid should be present so as to wet all the powder particles. Several methods of condensation are employed (1) in the vibration method; the paste is applied on to the platinum matrix and vibrated slowly. This brings the excess water on to the surface, which is then drawn away with a linen or clean tissue. Excessive vibration should be avoided as it can cause slumping of the mass (2). In the spatulation method, a small spatula is used to apply and smooth the wet porcelain. The smoothening action disturbs the particles bringing them closer and also the water rises to the surface, which is removed as described earlier (3) Dry brush technique involves placement of dry powder onto the wet surface. The excess water moves from mixture to the dry powder by capillary action and the wet particles are pulled together (4) In the whipping method, a large soft brush is moved in a light dusting action over the wet porcelain. This brings excess water to the surface, and the same brush can be used to remove any course surface particles along with the excess water. A combination of the vibration and the whipping methods can also be used. The mix is first vibrated and then whipped with a brush. 18
- 19. FIRING PROCEDURE Most of the thermochemical reactions in porcelain are completed during the manufacturing process. The role of firing is simply to sinter the particles of porcelain powder together to form a dense restoration. Some chemical reaction may however occur during prolonged firing or multiple firings, like the formation of leucite crystals in porcelain. During firing, the following changes are seen in the porcelain. The first change involves the loss of water, which was added to the powder to form a workable mass. The excess water is partially removed by slightly warming the mix before it is placed in the preheated furnace. This prevents the sudden production of steam that could result in voids or fractures. After the mass is placed in a furnace, both free and combined water are lost of until a temperature or 480o C is reached. The second change occurs with a further rise in temperature when the particles fuse together by sintering. As a continuous mass is formed, there occurs a decrease in volume referred to as firing shrinkage (32-37% for low fusing and 28.34% for high fusing). The third change seen is glazing which occurs at temperatures of 955-1065o C. Glazing results in the formation of a glossy surface. After the mass has been fired, it is cooled very slowly because rapid cooled might result in surface cracking and crazing. Porcelain restorations may be fired either by the temperature method or the temperature-time method. In the former, the furnace temperature is raised at a constant rate until a specific temperature is reached. In the latter, the temperature is raised at a given rate until certain levels are reached, after which the temperature is maintained for a measured period of time until the desired reactions are completed. Different media can be employed for firing like: a) Air b) Vacuum c) Diffusible gas AIR FIRING PROCEDURE: All porcelain powder mixes have a certain amount of porosity present in them. When these porcelains are placed in the air furnace, the furnace atmosphere occupies these void spaces. Once the softening of glass begins, the grains of porcelain start lensing at their contact points. Surface tension causes some of the porosity to be swept out via the grain boundaries, but some of it gets entrapped by the flowing ceramic around the air voids. With the increase in temperature, the void spaces containing air assume a spherical appearance under the influence of surface tension. Still further rise in temperature increases the pressure of the entrapped air and the bubbles enlarge. Cooling decreases the pressure and hence the size of the bubble. The surface of air-fired porcelain is generally devoid of bubbles because intestinal air near the surface can escape easily. Whenever air-firing methods are employed, a very slow maturation period is preferred to allow for the maximum amount of entrapped air to escape. The porcelain should not be exposed to its full maturing temperature and it is advisable to stay 30o C to 50o C below the maximum firing temperature. 19
- 20. POROSITY Bubbles or voids in the fired porcelain are caused by inclusion of air during firing or in some cases as a byproduct of vitrification of feldspar. Porosity reduces both translucency and strength of dental porcelain. Translucency depends on the number and size of the entrapped air bubbles. Large sized particles have fewer but larger air voids between them compared to small sized particles. Fewer bubbles, even of large size, give improved translucency. On the other hand, fine sized particles have multiple small air bubbles present in between them, which makes them highly opaque. It is, therefore, clear that porcelain powders fired in air must be of necessarily coarse nature. VACUUM FIRING This technique is used to reduce porosity in dental porcelains. It works on the basis of removing air or atmosphere from the interstitial spaces before surface sealing occurs. Although the vacuum (760 torr) removes most of the air from interstitial spaces, some of it is left behind. With the increase in temperature and because of surface tension, the remaining air spaces assume a spherical appearance. When air at normal atmospheric pressure is allowed to enter the furnace, it exerts a compressive effect on the surface skin, which further compresses the internal voids to one tenth of their original size. This results in a very dense porcelain with very few remaining bubbles and that too of extremely small size. Factors to be kept in mind while firing porcelain in vacuum are : 1. Porcelain powders must be dried slowly to eliminate the water vapour, and vacuum should be applied before the placement of porcelain in the hot zone of furnace. The interstitial spaces are hence reduced before the surface skin seals off the interior too rapidly. 2. Vacuum should not be applied after the surface skin has sealed and the porcelain has matured. Prolonged application can force the residual air bubbles to rise to the surface and cause surface blistering. Additionally, high temperatures can cause swelling of these blisters. 3. The vacuum should be broken while the work is still in the hot zone of the furnace. This permits the dense skin to hydraulically compress the low- pressure internal voids. 4. Vacuum firing cannot reduce the large sized bubbles to any significant degree. Hence, it is necessary to avoid porcelains with large interstitial spaces i.e., porcelain powders with small sized particles are preferred. DIFFUSIBLE GAS FIRING In this technique, a diffusible gas like helium, hydrogen or steam is substituted for the ordinary furnace temperature. Air is driven out of the porcelain powder bed and replaced by the diffusible gas. With these gases, the interstitial spaces do not enlarge under the influence of increasing temperature, but decrease in size or disappear. This occurs because these gases diffuse outward through the porcelain or actually dissolve in porcelain. 20
- 21. VARIOUS STAGES OF MATURITY Several stages of dental porcelain have been identified when it is ‘sintered’ or ‘fired’. The common terminology used for describing the surface appearance of an unglazed porcelain is ‘bisque’. Low bisque : The surface of porcelain is quite porous. The grains of porcelain begin to soften and ‘lense’ at their contact points. Shrinkage is minimal and the fired body is extremely weak or friable. Medium bisque : Pores still exist on the surface of porcelain, but the flow of glass grains is increased. As a result, any entrapped furnace atmosphere that could not escape via the grain boundaries becomes trapped and sphere shaped. A definite shrinkage is evident. High bisque: The flow of glass grains is further increased, thereby completely sealing the surface and presenting smoothness to the porcelain. In the case of non-feldspathic porcelains, a slight shine appears at this stage. The fired body is strong and any corrections by grinding can be made prior to final glazing at this stage. ALL CERAMIC SYSTEMS CLASSIFICATION 1. Conventional powder slurry ceramic • Hi Ceram – Alumina reinforced porcelain • Optec HSP – Leucite reinforced porcelain • Duceram LFC – Hydrothermal low fusing ceramic 2. Pressable ceramic • IPS Empress • Optec Pressable ceramic 3. Infiltrated ceramic • In-Ceram 4. Castable ceramic • DICOR • Cera Pearl 5. Mechinable ceramic • Cerec Vitablocs Mark I and II • Celay Blocks • DICOR MGC ALUMINA REINFORCED CERAMIC / ALUMINIOUS CERAMICS It was introduced by McLEAN and HUGES in 1965. They advocated the use of glass alumina composite. McLean used a relatively opaque of high alumina content for maximum strength surrounded by a combination of body and enamel 21
- 22. powder 15% and 5% respectively, of alumina resulting in a restoration that has 40% more strength than traditional restoration. Gradually high alumina ceramics developed which consisted of minimum 95% alumina. When alumina powder was fired first a welding of contact points occur followed by normal sintering which, resulted in a unique fusing effect of partial fusion. Further there is a expansion of crystal lattice by migration of atoms which lead to movement of grain boundaries and reduction of porosity. The strength of the crown increased to about 800 Mpa. Indications 1. There is a shoulder thickness of only 0.5 mm possible on the labial surface. 2. There is an occlusal clearance of more than 0.5 mm in lateral excursions. HI CERAM Hi-Ceram was developed in 1985 borrowing a technique from industrial manufacturing.It is a system similar to aluminous core ceramic crown, using an epoxy die, a swaged resin coping and a conventionally applied ceramic. Indications : 1. Anterior crowns 2. Posterior crowns where occlusal conditions are favourable. 3. Patients who do not want a metal core. 4. Patients who are allergic to metals. 5. Patients who require light reflection from tooth through the core of the crown for esthetic purpose. Contraindication 1. For posterior crowns where occlusal stress is high. OPTEC HSP (HIGH STRENTTH PORCELAIN)/OPTEC VP (VENEER PORCELAIN) Many porcelain systems cause wear to the opposing dentition during function, which usually necessitates nightguard use. New low-wear ceramics may remove the need for a nightguard in the future. With the advent of low-fusing, low-wear ceramics built over a pressable ceramic (Optimal Pressable Ceramic [OPC], Jeneric / Pentron, Inc.), has excellent esthetics, translucent margins and many of the new colors are designed to match bleached teeth. The Optimal System is the newest generation of ceramic powder, stemming from Jeneric / Pantron’s eight years of research, development and clinical success with high-strength leucite based ceramic products. Lifelike anterior metal ceramic restorations are very difficult to fabricate; even the most talent ceramist has difficulty producing natural color and translucency because of the metal core. The elimination of the metal framework or coping immediately increases the chance for esthetic success. Ceramic cores are either opaque or translucent; the opaque cores exhibit better fracture toughness. Translucency is better controlled with semi-opaque cores or when the porcelain matches the color and light transmission of the natural dentin as in the leucite-reinforced ceramics (Optec, Jeneric / Pentron, Inc.; IPS Empress, Ivoclar Williams). The strength needed for anterior crowns does not always call for a metal or ceramic opaque core. According to Anusavice, “All-ceramic crowns should be reserved for anterior and premolar teeth”. 22
- 23. It is a lucite –reinforced All ceramic material (leucite is 45-50%). IPS Empress and OPC basically are the same ; however, OPC’s leucite crystal (filler) is smaller, resulting in higher compressive strength (187 to 320 psi) and a flexural strength of over 23,000 psi. The process of heat pressing the ceramic rather than stacking the material differentiates OPC form IPS Empress. It has 50% leucite in a glass matrix therefore stronger than conventional feldspathic porcelain. These leucite crystals are dispersed in a glassy matrix by controlling their nucleation during production. No core is required like Dicor. VP is higher in chroma than HSP. Indications • Anterior Single Units. • Posterior Single Units. • Veneers. Contraindications • Clenching and bruxism. • Short clinical crowns • Large or immature pulp chambers. • Abnormal occlusal relationships • Existing periodontal disease. OPC is the second-generation product of IPS EMPRESS. OPC is 15% stronger. OPC has a clinical history of 8 years. OPC has 58 shades of porcelain powders compared to the 19 of IPS EMPRESS, which aids in achieving the highest level of esthetics. OPC is matched to the universally used Vita shade guide system. No need to purchase a new chromoscope shade guide. It is fabricated using injection-molding technique. PHYSICAL PROPERTIES Flexural Strength It is approximately 167Mpa. With OPC, Jeneric Pentron has increased strength and reliability by reducing the size of the leucite crystal and improving its distribution without reducing the total crystalline content. This gives it a compressive strength of 187 to 320psi and flexural strength of over 23,000psi. Unlike a few other All-ceramic systems, Optimal is a bondable material, giving the entire tooth an additional measure of strength. Translucency Its translucency is 3. Marginal Fit Optimal provides an extremely high degree of fit to tooth. This results in increased load bearing capacity. Low Fusing Ceramics Low fusing ceramics have been developed primarily for the use with titanium frameworks. Titanium is now being used for metal ceramics because of its biocompatibility and corrosion resistance.Low fusion porcelains are required to 23
- 24. adequately match the coefficient of thermal expansion of titanium to reduce residual stress, which may result in failure of the overlying ceramic. The fusion temperature of these materials ranges from 650o C to 850o C. Lower fusing temperatures may also preserve the microstructure of the ceramics, in contrast to the high fusing material, which may suffer from dissolution of crystalline components. PHYSICAL PROPERTIES Flexural Strength Flexural strength of low fusing ceramics is comparable to feldspathic ceramics. Indications : • Used directly to fabricate all ceramic inlays, onlays and veneers. • For repair and correction of metal ceramic margins. DUCERAM LFC It is a low fusing ceramic. It is composed of an amorphous fluorine glass containing hydroxyl ions and the base layer composed of Duceram Metal Ceramic leucite containing porcelain. Duceram LFC is then layered on base layer as a powder-slurry. It is then strengthened by ion exchange mechanism involving hydroxyl ions thus decreases the surface micro flaws and increase fracture resistance. It has a firing temperature of 702o C. IPS EMPRESS IPS EMPRESS is a heat-pressed glass-ceramic that has superior mechanical properties for several reasons. The high shrinkage of leucite crystals creates compressive stress in the vitreous phase, when prevents the development of surface cracks. The randomly oriented leucite crystals are tightly packed in the vitreous phase and stop the propagation of micro cracks. The combination of heat pressing, initial firing, and stain and glaze of the veneers creates an additional 50% in strength. The higher cohesive strength and fracture toughness allow for thicker areas of porcelain with a lesser risk of fracture. IPS EMPRESS glass-ceramic has been successfully used as metal free dental restorative in clinical situations for the past 6 years. Numerous studies confirm that this material fulfills the high standards of esthetics demanded form restorations such as inlays onlays and veneers. IPS EMPRESS systems are characterized as follows: 1. It is an All-ceramic system. 2. It is a glass-ceramic system. 3. It is leucite reinforced. 4. It is based of principles of surface crystallization. 5. Features increased strength due to dispersion strengthening. 6. It is processed using a heat processing technique. 24
- 25. CHEMICAL COMPOSITION ON IPS EMPRESS The chemical composition of IPS EMPRESS glass-ceramic is given in weight %. • SiO2 – 59.0 to 63.0 • AI2O3 – 19. to 23.5 • H2O – 10.0 to 14.0 • Na2O – 3.5 to 6.5 • CeO2 - 0 to 1.0 • CaO – 0.05 to 3.0 • BaO – 0 to 1.5 • TiO2 – 0 to 0.5 Manufacturing of IPS empress glass-ceramic Initially a base glass whose composition is of particular importance is chosen this is important for controlled crystallization (at a later stage) is melted subsequently. It is heat treated to initiate nucleation and primary crystallization, and then it is grounded.The powder to which the stabilizer, additives, fluorescent agent and pigments have been added is then pressed to form ingot. Once the ingot has been sintered to about 1200o C it is ready for sale on the market for processing in EP500 press furnace. Fabrication of IPS Empress restoration : The fabrication of a dental crown according to layering technique, for example is characterized by wax up of a reduced model that is invested in a special investing material, after a muffle has been preheated the wax is burnt-out, it is placed in a EP500 press furnace (Ivoclar Company Limited, Schaan, Liechtenstein). Subsequently, a glass-ceramic ingot for layering technique is pressed into the mould of the reduced crown at 1180o C according to the viscous flow process. The crown framework is exposed to this temperature for 35 minutes. It is then cooled, divested and finished. Then the ceramic incisal materials for layering technique for short “layering ceramic” and glaze are applied. These materials are sintered at about 910 to 870o C respectively. Glass-ceramic ingots for sintering technique is preferred for fabrication of the various restorations like inlay, onlays, and veneers etc. The ingot is pressed at 1050o C for staining technique. This provides IPS EMPRESS glass-ceramic with its ultimate strength and esthetic properties. PHYSICAL PROPERTIES Flexural Strentth The basis strength of EMPRESS glass-ceramic has been shown to measure approximately 120 to 140 Mpa. The basic strength accounts to the EMPRESS glass- ceramic, which has been divided from the muffle but not exposed to further heat treatment of layering. Heat processing the material significantly improves is flexural strength whereas heat- treating the material alone dose not. Additional firing after heat pressing further increases the material strength to about 140 to 220 Mpa. The flexural strength of the IPS EMPRESS glass-ceramic is the result of microscopic areas of compressive strain 25
- 26. on the surface of the crown, inlays etc, produced by internal stress by heat. Significant increase in the flexural strength can be achieved by glazing the ceramic materials for the staining and the layering techniques. Fracture Resistance IPS EMPRESS crowns have a good fracture resistance when compared with all other All-ceramic crowns. The fracture resistance of DICOR is not much higher than that of VITADUR. The fracture resistance of IPS EMPRESS is about 0.5 to 1 Kn. The fracture resistance of IPS EMPRESS greatly depends on the cementation method. Sandblasting, etching with HF and subsequently silanizing greatly increasing the fracture resistance. The fracture resistance is higher when the IPS EMPRESS is fixed with adhesive cements than conventional cements. Fracture Toughness Dental ceramic can fail through growth of microscopic surface flaws that form during processing or from surface impact during service. New dental ceramics have been developed to improve resistance to crack propagation, which induced furomica, leucite, alumina and zirconia reinforced glass. The leucite reinforced All-ceramic system, IPS EMPRESS demonstrated significantly higher fracture toughness than alumina or fluromica reinforced materials DICOR and DICOR MGC. INCERAM SADOUN developed INCERAM in 1985. It makes use of aluminous core that is infiltrated with a glass to achieve high strength substratures that can support crowns and bridges. It belongs to a class of material known as interpenetration phase composites. These materials have at least two phases that are interveined and extend continuously from the internal to external surfaces. These material posses improved mechanical and physical properties when compared to the individual components. They have improved fracture resistance and strength due to the fact that a crack must pass through alternative layer of components no matter what direction the crack propagates. Composition of Inceram Al2O3 – 90.8% SiO2 – 3.6% K2O – 1.0% CaO – 0.04% Fabrication Procedure An All-Ceramic restoration system INCERAM is based on the slip casting of an alumina core with its subsequent glass infusion. After the impression is taken the die is poured with special gypsum supplied with INCERAM, then the INCERAM ALUMINA is applied onto the die.The alumina powder is mixed with deionized water supplied in pre-measured container. Dispensing agent is added to create a homogenous mix of alumina in water. This mixture is sonicated in VITASONIC thus initiating the dispersion process. Then vacuum is applied to remove the air bubbles.This solution of alumina is referred to as “slip” which is then painted onto the gypsum die with a brush. The alumina is built up to form a core for the ceramic tooth. 26
- 27. The water is removed by the capillary action of the porous gypsum, which packs the particles into a rigid network. The aluminous core is then placed in the IN-CERAMET furnace and sintered. The cycle involves a slow heating of approximately 2o C/min to 1120o C for 2 hours to produce approximation of the particles with minimal compaction and minimal shrinkage of alumina. Sintering is only about 0.2% thus an interconnected porous network is created connecting pores on the outer surface with those on the inner surface.Low viscosity lanthanum aluminosilicate glass is used to fill the pores in the alumina. The glass is mixed with water and placed on a platinum – gold alloy sheet. The external surface of the core is placed on the glass, which is heated in the IN- CERMET to 1100o C for 4-6 hours. The glass becomes molten and flows into the pores by capillary diffusion. The excess glass is removed by sandblasting with alumina particles.The last step is fabrication of INCERAM restoration involves application of aluminous porcelain to the core to produce the final form of restoration. The low viscosity lanthanum glass is used to infiltrate the alumina core in INCERAM. This should be in air environment as recommended by the manufacture. The INCERAM aluminous glass ceramic produced by lanthanum glass infiltration is about 50% translucent as dentin. In clinical situations where there is a discolored preparation or a cast post and core this increased opacity over the dentin is advantageous were as when maximum translucency is necessary INCERAM ALUMINA is problematic. PHYSICAL PROPERTIES Flexural Strength The flexural strength of INCERAM ALUMINA varies from 300 Mpa to 600 Mpa. It is four times greater than other classes of dental ceramics. It is theorized that this high strength results from the primarily crystalline nature of this material and its minimal glassy phase. A flaw would have to propagate through its high modulus alumina to cause ultimate failure.INCERAM material is not used as core alone ; they are also veneered with a low strength material to achieve the final esthetic result. The effect on strength of veneering cost a minimal drop in the strength of INCERAM ALUMINA material if the core remained at least 1mm thick. If the core material is thinned to about 0.5mm and then veneered with 1 mm thickness of porcelain, then the flexural strength drops to 255 Mpa. This should be adequate for incisors and bicuspids but not for molars. Fracture Resistance The fracture strength of INCERAM ALUMINA is higher when compared to other all-ceramic systems. It is about 1060 (341 N). Fracture Toughness Dental ceramics can fail through growth of microscopic surface flaws that form during processing or from surface impact during service. In Inceram alumina the resistance to crack propagation is improved by reinforcement with alumina. Fracture toughness is about 4.49 Mpa.m1/2 or 4.7 Mpa M-2 . 27
- 28. Inceram Spinell A second-generation material, inceram spinell, is based on the inceram technique, has recently been introduced. The technique of fabrication is essentially the same as the original system.The primary difference is a change in composition to produce a more translucent core. The porous core is fabricated from a magnesium – alumina powder to form the porous core after sintering instead of alumina powder as in INCERAM ALUMINA. This type of material has a specific crystalline structure referred to as “SPINELL”.The porous spinell is secondarily infiltrated with a low viscosity, lanthanum aluminosilicate glass, which produces a more translucent substructure upon which Vitadur Alpha is veneered to form the final restoration. The glass infiltration of INCERAM SPINELL should be done in a vacuum environment. INCERAM SPINELL is twice as translucent as INCERAM ALUMINA because the refractive index of its crystalline phase is closer to that of glass and the vaccum infiltration leaves less porosity. The translucency of INCERAM SPINELL closely matches that of dentin. Indications: • Anterior crowns • In clinical situations where maximum translucency is needed. Contraindications : • Posterior restorations. • Anterior and posterior FPDs • In discolored preparations and cast posts as the level of translucency is excessive and leads to an overly glassy low value appearance. PHYSICAL PROPERTIES Flexual Strength The flexural strength of INCERAM SPINELL is 15% to 40% that of INCERAM ALUMINA thus being indicated for anterior crowns only. About 350 Mpa. Fracture Toughness The fracture toughness of INCERAM SPINELL is about 2.7 Mpa M-2. Inceram Zirconia INCERAM ZIRCONIA is also a second-generation material based on INCERAM fabrication technique. The difference is being a change in composition to produce a material that has improved flexural strength and fracture toughness. The porous core fabricated with INCERAM ZIRCONIA has a tetragonal form of crystal. The porous core is secondarily infiltrated with a low viscosity, lanthanum alumino-silicate glass, which produces a stronger substructure. Zirconia has a physical property called transformation toughening (strengthening) when an external source is applied to the material is goes through a phase transformation to a monoclinic form of zirconia. The monoclinic form of crystal is 3% to 5% larger, thus in places of micro cracks this process can seal the cracks. 28
- 29. PHYSICAL PROPERTIES Flexural Strength Flexural strength of INCERAM ZIRCONIA is twice as that of alumina. The highest strength at 800 Mpa. Fracture toughness Also tough that of aluimina. It is about 6.8 Mpa M-2. Indication • 3 unit FPDs for posteriors. CASTABLE GLASS CERAMIC DICOR A glass ceramic is a material that is formed into the desired shape as a glass and subsequently heat-treated under controlled conditions to induce partial devitrification ir crystallization. This conversion process, which involves crystal nucleation and growth is referred to as “ceramming” and is accompanied by a small and controlled volume change. The crystalline particles, needles or plates formed during the ceramming process constitute an interlocking network, which increases the strength of the material by interrupting crack propagation. The first description of DICOR castable ceramic was given by Adair and Grossman in 1984. The glasses ceramic material is composed of SiO2, K2O, MgO, MgF2, minor amounts of Al2O3, and ZrO2 incorporated for durability, and a fluorescing agent for esthetics. The fluoride acts as a nucleating agent, and improves the fluidity of the molten glass. After ceramming, the material is approximately 55% crystalline an contains tetrasilicic fluoride crystals (K2 Mg5 Si8O20Fl), which closely resemble mica. The refractive index of these crystals is close to that of the surrounding glass matrix, helping to maintain translucency in the devitrified body. Mica crystals are achromatic and the desired shade in final restoration is developed by adding external colorants. The disadvantage behind the use of these colorant stains is that they may be lost during occlusal adjustment, during routine prophylaxis or through the use of acidulated fluoride gels. The fabrication method for DICOR restorations uses the lost wax and centrifugal casting techniques similar to those used for fabricating alloy castings. A wax pattern similar to the final restoration is made and invested in a phosphate bonded refractory material. Molten glass is then cast into the heated mould after dewaxing. The cast restoration is freed from the investment, covered by a protective ‘embedment” material and subjected to ceramming. Addition of 2.5% lithium fluoride to the embedment material may promote crystallization of mica and increase the fracture toughness of glass ceramic. The completed restoration is acid etched on its fit surface to enhance bonding to the underlying tooth. Surface stains and colored luting cements are employed to improve upon the esthetics. Properties The physical properties of DICOR are given in the table. PROPERTY DICOR ENAMEL FELDSPATHIC PORCELAIN Density, g.cm3 2.7 3.0 2.4 29
- 30. Translucency 0.56 0.48 0.27 Modulus of rupture psi 22000 1500 11000 Compressive strength, psi 120000 58000 25000 Modulus of Elasticity, psix106 10.2 12.2 12.0 Microhardness 362 343 450 Esthetic Qualities DICOR restorations are highly esthetic because of their translucency, which closely matches that of natural tooth enamel. The numerous small mica crystals that constitute castable ceramic closely match in their index of refraction to the surrounding glass phase. In addition, the castable ceramic permits a one-piece restoration made entirely of the same material, and no opaque substructure exists to impede light scattering. A chameleon effect is seen with DICOR restorations in which the restoration acquires a part of the colour from adjacent teeth and fillings as well as the underlying cement lute. Application of an external colouring system allows independent control over hue, chroma and value. However, as mentioned before, there are chances of losing this external layer thereby defeating the best of esthetics. Precision Of Fit It has been found to withstand 20 years of simulated toothbrush abrasion without any changes. The resistance of DICOR to chemicals and staining agents also compares favorably with conventional feldspathic porcelains. Little wear of the cast ceramic or the opposing dentition occurs when using DICOR restorations. Two reasons for this property are: a. Closely matching hardness between the cast ceramic material and natural enamel. b. The DICOR shading porcelains contain minimal abrasive opacifying agents. Tissue Acceptance DICOR is chemically inert and has shown to pass all the biocompatibility tests. The periodontal tissue reaction to DICOR is considered quite favourable because 1. There is no need for opaquer porcelains to mask the metal substructure. These coarse grained opaque porcelains generally promote the adherence of plaque. 2. The absence of an opaque layer allows the technician to obtain natural contouring often found in metal ceramic restorations. Little discomfort occurs on contact with hot or cold foods because of its extremely low thermal conductivity and a coefficient of thermal expansion, which closely matches that of natural enamel. Radiographic Qualities The radiographic density of DICOR is similar to that of enamel allowing proper evaluation of the underlying structures and the margins. Advantages 1. Excellent marginal fit 2. Relatively high strength 30
- 31. 3. Surface hardness and occlusal wear is similar to enamel 4. Can reproduce wax patterns precisely by using the lost wax technique 5. Simple uncomplicated fabrication from waxup to casting, ceramming and colouring 6. Ease of adjustment 7. Excellent esthetics resulting from natural translucency 8. Inherent resistance to plaque accumulation (seven times less than on the natual tooth surfaces). Disadvantages 1. Chances of losing low fusing feldspathic shading porcelains, which have been applied for good colour matching. Uses Inlays, onlays, complete crowns and possibly partial tooth coverage restorations. It is not indicated for fixed partial denture or removable partial denture abutments with deep rests or internal attachments. CERA PEARL Castable apatite ceramic was first developed by Hobo and Bioceram Group as CaO-P2O5-MgO-SiO2 glass ceramic. This material can be cast similar to the dental metal alloys. Its casting once obtained has an amorphous structure but when subjected to ceramming, crystalline oxylapatite, Ca10(PO4)6O results. This apatite is chemically unstable but becomes stable when exposed to moisture by forming crystalline hydroxylapatite. Compared to normal enamel, the crystals of Cera Pearl show a somewhat irregular arrangement and this different arrangement probably accounts for its superior mechanical properties. Cera Pearl is composed of CaO, P2O5, MgO, SiO2 and traces of other elements. CaO(45%) and P2O5 (15%) are the main ingredients in glass formation. They are essential for formation of hydroxylapatite crystals as well. MgO (5%) helps in the formation of hydroxyapatite and along with CaO decreases the viscosity of the compound when melted. SiO2(34%) in combination with P2O5 forms the matrix. Further SiO2 regulates the thermal properties. Because the crystalline constituent is similar to natural enamel, Cera Pearl is also expected to be quite biocompatible. The Young’s modulus, tensile strength and compressive strength of Cera Pearl are appreciably higher than conventional porcelains and most restorative materials where as hardness compares favourably with the natural enamel. The values for these mechanical properties are given in the table below. Cera Pearl is indicated for both crowns and inlays. However, Cera Pearl is still currently in a research phase and is not yet commercially available. It is included in the text because it is a castable glass ceramic and has properties that are comparable to other ceramic materials. 31
- 32. Material Young’sModulus (GPA) TensileStrength(MPa) Compressive Strength (MPa) KnoopHardness Number(KHN) Coefficientof ThermalExpansion (10-6 /C) Thermal Conductivity(Cal cm/cm2 sec°C) Cera Pearl 103 150 590 350 11.0 .0023 Gold Alloy 95 140 220-240 14.4 Enamel 80 14 390 390 11.4 .0022 Dentin 20 70 280 70 7.0 .0014 Porcelain 70 80 170 590 12.0 .0024 Amalgam 58 70 360 120 25.0 .0540 Composite resin 18 18 185 39.0 .0026 SHRINK FREE CERAMIC CERESTORE It is a shrink-free alumina crown developed by the Coors Biomedical Co. and later sold to Johnson & Johnson. It is fabricated using lost wax technique and then injection molding to produce a coping. MgAl2O4 spinell and an alpha-alumina oxide make the core replaced by Alceram. The use of a shrink-free ceramic coping formed on an epoxy die by a transfer molding process overcomes the limits and firing shrinkage of conventionally produced aluminous porcelain jacket crowns. The Cerestore coping is veneered with conventional aesthetic porcelain. Flexural strength: It is approximately 150 Mpa. CERAMIC MACHINING SYSTEMS CAD-CAM (Computer Assisted Design-Computer Aided Manufacturing) system has been introduced to the dental profession recently. Development of CAD-CAM system for the dental profession began in 1970’s with DURET in France, ALTSCHULER in US & BRANDESTINI in Switzerland. Optical scanning and computer generation of restoration were attempted as early as 1971 (ALTSCHULER 1971/1973). With the continued improvement in the technology, a number of systems are currently being investigated. The teams most actively pursuing this technology of CAD/CAM systems in dentistry are: 1. French group headed by Dr. FRANCOIS DURET. 2. Denti CAD units by Dr. DIANNE RCHOW. 3. CEREC system by MORMANN and BRANDESTINI. The introduction of CAD/CAM system to restorative dentistry represents a major technological breakthrough. It is now possible to design and fabricate ceramic restoration at a single appointment, as opposed to the traditional method of making impression, fabricating a provisional prosthesis and using a laboratory for development of a restoration. Certain errors, which were inherent to the indirect method, have been eliminated in these systems. Additionally CAD/CAM generated 32
- 33. save the dentist and patient time, provides an esthetic restoration and have the potential for extended wear resistance. All CAD-CAM system are technically complex & involves three distinct and complex steps: 1. Collection of information 2. Designing of restoration and 3. Fabrication of the restoration The popular CAD-CAM systems used in dentistry are: • CELAY system • CEREC system • DCS Precident system • PROCERA system CEREC CEREC is a dental CAD/CAM machine. CAD/CAM stands for computer assisted design, computer aided manufacturing. Mormann’s work led to the development of Siemens’ CEREC CAD-CAM system. It was developed in Zurich Switzerland. It is used to fabricate inlays, onlays, ¾ crowns, 7/8 crowns and veneers. This system enables the direct chair side placement of ceramic restoration without auxiliary laboratory support. CEREC CAD/CAM machine is used to produce full ceramic restorations in one patient visit. It has been used clinically since 1986. CEREC 2 was introduced in 1996; CEREC 3 and Scan were introduced by Sirona Dental Systems (Germany) in 2000. The CEREC technique consist of: 1. Three-dimensional scanning of the cavity or taking an optical impression. 2. Immediate data transformation and 3. Axial milling, which is integrated into a mobile unit. Occlusal surfaces can now be machined on the Cerec 2 unit smaller pixel size/higher accuracy in depth measuring = increased resolution of the optical impression. There are 3 different programs for design, Extrapolation, Correlation, and linear. (1) Anatomically adapted (extrapolation) (2) Correlated to functionally generated path (correlation (3) Bucco-linearly flat (inner). The Cerec system is the only method in dentistry to permit the exact machining of ceramic veneers. The precision of Cerec 2 grinding unit improvements form the Cerec 1 system, in an SEM examination marginal widths of Cerce 2 were considerably smaller than Cerec1. THE CEREC FAMILY: CEREC CAD/CAM was developed in ZURICH SWITZERLAND. It has been in clinical use since 1985.86. Since the introduction of CEREC CAD/CAM in 1985 there has been major advancement CAD/CAM systems, which has resulted in the development of CEREC 2 AND CEREC 3 systems. 33
- 34. CEREC 3 is the latest version. CEREC 3 has many advantages over CEREC 2 system. Those having CEREC 2 systems by incorporating new software called CEREC L ink can exploit these advantages. The following section gives a brief introduction to the CEREC family. CEREC: The CEREC was first introduced in 1986. it consisted of a mobile unite containing a small camera, a computer with scan and 3-axis-of rotation milling machine. This old milling machine was water-pressure driven “hydro” version. CEREC2: It is a tried-and-tested, compact CAD/CAM (Computer Aided Design-Computer Integrated Machining) system for chairside applications. It is the CAD/CIM system with the largest number of users worldwide, several million successful restorations and clinical experience since 1986. it consists of a mobile unit containing a small camera, a computer with scan and 3-axis-of-rotation milling machine. The milling machine has an electric motor called “E” version to provide a better and smoother cutting of ceramic resulting in better fitting restorations. The occlusal surfaces can now be machined on the Cerec 2 unit. It has smaller pixel size/higher accuracy in depth measuring which increases the resolution of the optical impression. There are 3 different programs for designing: Extrapolation, Correlation, and linear. (1) Anatomically adapted (extrapolation) (2) Correlated to functionally generated path (correlation) (3) Bucco-linearly flat (linear). The precision of Cerec 2 grinding unit has been found to be 2.4 times higher than Cerec. CEREC3:It is the modular CAD/CAM system that adapts flexibly to practice requirements. It provides virtually unlimited scope for incorporating the CEREC 3 modules into the practice layout. It gives flexible integration into the practice workflow (direct or indirect working; labside or chairside; one or more treatment sessions – the choice being yours). It provides rapid imaging, design, handling hygiene through the integration of the SIDEXIS intraoral X-ray system and the SIROCAM 2 intraoral camera. CEREC 3 is flexible and offers the most advanced solution for every practice concept. The new highlight in the CEREC product range is the modular CEREC 3, which offers virtually unlimited scope to optimize practice workflow. Consisting of a separate imaging unit and milling unit, the CEREC 3 adapts to a wide variety of different practice layouts. The systems are designed for multiple as well as single restorations and enable to use the imaging unit for other tasks during the milling process. The imaging and milling units can be located in one room or in separate locations. They communicate with each other either via cable or via radio signals. The CEREC 3 milling unit can be installed in a wide variety of different locations like in the treatment room itself (essay access), in a cupboard (reduced noise), in an unused corner or niche (saves space), in the practice lab or as a fascinating eye- catcher in the waiting room. 34
- 35. The multiple functions of the CEREC3 imaging unit are creating optical impressions, designing the ceramic restoration, and chairside patient communication. Advantages of CEREC 3: 1. The CEREC 3 imaging unit incorporates a mobile PC, which has been specially approved for medical applications. Milling chamber is separate form the imaging / designing unit. 2. The system is now Windows – based. 3. Cerec 3 can be used in conjunction with a Cerec 2 by using the “Link” software. 4. Two burs (one is tapered) do the cutting instead of one bur and one diamond wheel. 5. No “adjust” process (time savings) 6. Faster milling times (5 minute savings) 7. Greater occlusal anatomy 8. All design windows can be open at once 9. Help screen runs automatically and guides through the process. MILLING CHAMBER: The new CEREC 3 software is Windows based allowing greater compatibility and sharing possibilities. CEREC EQUIPMENT The intuitive user interface has been optimized for dental applications and does not require any specialist computer knowledge. Equipment: • Flat panel monitor. • High-precision measuring camera. • Microprocessor-controlled image capture card, which processes the images from the 3-D measuring camera in real time. • Windows-based CEREC 3-Software. The CEREC 3 imaging unit with SIDEXIS and SIROCAM 2 is designed for mobile applications as well as for integration into a networked practice system. CEREC SCAN: It is an entry-level model for indirect working. Low capital outlay is ideal for new practice start-ups. All processing steps can be delegated to the assistant. Upgrade option: It can be turned into a fully-fledged CEREC system via the addition of an imaging unit. Based on the CEREC 3 milling unit, the CEREC Scan has been optimized for the indirect working mode, i.e. the creation of ceramic restoration from dental models. The resultant cost reductions make the CEREC Scan an attractive option for dentists who are setting up in practice for the fist time and whose financial resources are limited. By adding the imaging unit at a later date the CEREC Scan can be converted into to a fully-fledged CEREC 3 system. 35
- 36. FABRICANTING PROCEDURE: Following the preparation phase the assistant takes a conventional insitu impression and then produces a partial model made of quick-setting silicone This model is then clamped into the holder of the milling unit, where it is scanned by the built-in laser (duration: approx.5 minutes). The design process is performed on a separate a PC in the dental practice. The actual production of the ceramic restoration takes place in the milling unit. Although the CEREC Scan restorations are produced indirectly they can still be completed in a single treatment session, due not least to the speed of the laser scanning operation. The patient can watch the fascinating scanning and milling process “live”. The CERECE Scan is geared to the same broad range of clinical indications as the CEREC 3. The production process can be delegated to an assistant or dental technician in the practice laboratory. This cuts costs and helps to integrate the CEREC concept into the existing treatment procedure. In LAB from SIRONA: Introduced at the 2002 Chicago Mid-Winter meeting, the inLab system is designed specifically for Laboratory applications. The idea is to use CEREC’s fast manufacturing processes for producing crown “copings” and bridge “frameworks”. These substructures are to be milled from VITA INCERAM SPINELL, ALUMINA and ZIRCONIA blocks. The flexural strength of these materials is as follows: • INCERAM SPINELL: 350Mpa. • INCERAM ALUMINA: 550Mpa. • INCERAM ZIROCONIA: 750Mpa. Ideally, the clinician and the technician can apply the appropriate strength material for varying clinical applications. Once the substructure has been milled, the technician glass infiltrates the pre-sintered framework and then builds up the final restoration with a traditional porcelain stacking procedure with VITADUR ALPA porcelain. The process of building the substructure (coping or bridge framework) is as follows: 1) Scanning of the model 8-12 minutes 2) Designing the substructure (on a PC) 5 minutes 3) Milling the substructure 12-30 minutes 4) Glass infiltration 5-10 minutes A crown coping will take about 30 minutes to the finish. A bridge takes slightly longer at 57 minutes. Note however, the technician can be performing other functions during much of this process, namely the scanning and milling. Actual technician hands-on time is mere 5-15 minutes depending on the size of the restoration. This compares with a very long time to accomplish the same takes with regular INCERAM techniques, which is one of the main reasons INCERAM is not as widespread as it should be, but it should be because INCREAM has one of the best track records of ALL-CERAMIC materials. 36
- 37. Another bonus to this system over, says Procera is the choice of color matching. When the substructure is infiltrated with glass there is a choice of four colors. No opaqueing is required. This alone makes the inLab system more desirable but the laser scanning system is more accurate than mechanical systems. In fact the marginal accuracy of the inLab’s is excellent. CEREC SOFTWARE The original software of CEREC system is the Cos 1.0. This was replaced with updated versions like Cos 2.0 and Cos 2.1, which are used for CEREC 2 systems. Crown 1.30 and 1.31: There have been many software upgrades since CEREC 2 came onto the market. Most of these upgrades have been offered to users free of charge. CROWN 1.30 is the latest release. It replaces Crown 1.21 and allows to use the CEREC 2 with Link software version R600. Compared to working with R425, the PC constructs the milling data instead of the CEREC 2. This makes things much faster. Other features include: • Continue milling after instrument change • Perfect adaptation of the restoration to the used block-size by automatic • Block-rotation prior or the milling, which leads to smaller blocks and longer lifetime of disk and bur. CEREC 3 Software: The first software used for CEREC 3 systems was the R425. The CEREC 3 system now used the following software R600, R601, R800, R850 and the recently updated versions R900. R425: It is the older version, which does not allow transfer of data from PC back to CEREC 2. R600: It allows all designs, including the Correlation & linear. It helps to save files (Restoration/Export) anywhere on your computer, or to send the file to any one of the drives (floppy, zip, CD, etc) or might have on your computer itself. You can open files (Restoration/import) from anywhere on your computer or your drives. When designing in Link, you can now choose which type of bur you want to mill with. This allows you to use your computer to generate the milling data for your CEREC 2 (your computer generates milling data faster than your CEREC2). The CEREC 3 software is easy to use and produces optimum results. The CEREC 3 software like the corresponding hardware is based on a modular concept. We can choose the basic software for the creation of inlays and onlays or opt for the CEREC 3 Crown and/or CEREC 3 Veneer software packages. Whatever choice is made it 37
- 38. produces high-quality ceramic restorations simply, quickly and with the utmost reliability. More than three quarters of all CEREC users deploy crown construction software. Compared with the previous versions, the new CEREC 3 Crown is even quicker and easier to use. An example to illustrate how simple it is to create high-quality ceramic restorations will be given in the clinical procedure for CEREC system. CEREC LINK: It is a software package, which allows CEREC 2 users to exploit all the functions of CEREC 3 (including parallel design and milling). It helps in export of CEREC 2 images to a PC, access to PC functions during the design process and parallel milling and design. OPTICAL IMPRESSION: After tooth preparation the impression of the prepared tooth should be taken. In the CEREC CAD-CAM system instead of a conventional. Impression with elastomeric impression material an optical impression with a CEREC camera is taken. Before taking an optical impression the prepared tooth surfaces are powdered with a special powder, which has the ability to reflect the infrared light emitted from the camera. BACKGROUND INFORMATION ON POWDERING: To take an optical impression it is necessary to powder (or opaque) the tooth surface to be imaged because of two reasons: The surface of the tooth must be covered with a non-reflective coating to make it easier for the infrared camera to see detail. Without the non-reflective coating the effect on the camera is similar to our looking into a very bright light. Because of the high translucency of enamel, without an opaque surface applied to the tooth, the infrared beam would be projected back to the camera from totally different depths within the tooth. METHODS OF POWDERING: Powdering of the prepared tooth surface can be done using either: 1. BUTANE-PROPELLED POWDERIGN SYSTEM 2. PAINT ON SYSTEM or SCAN WHITE 3. POWDER MEISTER SYSTEM BUTANE PROPELLED POWDERING SYSTEM: The butane-propelled powdering systems has been the most widely used powdering system with CEREC, as it was the first introduced system of powdering but it has many disadvantages, which are as follows: it frequently clogs; even when a concerted attempt is made to hold the butane can upright. The powdering tubs are flimsy and easily deflected by the cheek or tongue. In order to change the direction of the powdering tube, a second hand is required, necessitating the clinician to let go of mirror or cheek. PAINT-ON OR SCANEWHITE SYSTEM: The above difficulties with the butane powdering system have forced many users to use a paint-on system. This paint-on system called Scan White has its own disadvantages. In the January 1999 issue of the International Journal of 38
