Respiratory diseases of equine
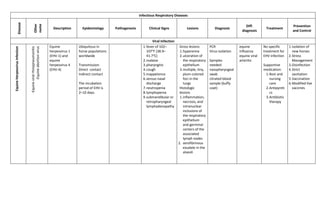
- 1. Infectious Respiratory Diseases Disease Other name Description Epidemiology Pathogenesis Clinical Signs Lesions Diagnosis Diff. diagnosis Treatment Prevention and Control Viral Infection EquineHerpesvirusInfection -Equineviralrhinopneumonitis -Equineabortionvirus Equine herpesvirus 1 (EHV-1) and equine herpesvirus 4 (EHV-4) Ubiquitous in horse populations worldwide Transmission: Direct contact Indirect contact The incubation period of EHV is 2–10 days. 1.fever of 102– 107°F (38.9– 41.7°C) 2.malaise 3.pharyngitis 4.cough 5.Inappetence 6.serous nasal discharge 7.neutropenia 8.lymphopenia 9.submandibular or retropharyngeal lymphadenopathy Gross lesions 1.hyperemia 2.ulceration of the respiratory epithelium 3.multiple, tiny, plum-colored foci in the lungs Histologic lesions 1.inflammation, necrosis, and intranuclear inclusions of the respiratory epithelium and germinal centers of the associated lymph nodes 2. serofibrinous exudate in the alveoli PCR Virus isolation Samples needed: nasopharyngeal swab citrated blood sample (buffy coat) equine influenza equine viral arteritis No specific treatment for EHV infection Supportive medication: 1.Rest and nursing care 2.Antipyreti cs 3.Antibiotic therapy 1.Isolation of new horses 2.Stress Management 3.Disinfection 4.Strict sanitation 5.Vaccination 6.Modified live vaccines
- 2. EquineInfluenza Most economically important contagious respiratory disease of horses. Highly contagious and spreads rapidly by direct contact Orthomyxovirus A/Equi-1 Orthomyxovirus A/Equi-2 Distinct influenza viruses have been found in horse populations worldwide except in Iceland and New Zealand. Influenza is rarely fatal except in donkeys, zebras, and debilitated horses. Transmision: inhalation of respiratory secretions Incubation period: ∼1–3 days Virus attaches to epithelial cells via hemagglutinin spikes and enters cells via endocytosis. Virus damages epithelial cells in the respiratory tree desquamation and focal erosion of the respiratory epithelium, Interruption of the protective mucociliary blanket impairment of clearance accumulation of mucus and bacteria in the airways exposure of the lamina propria and irritant receptors leading to frequent coughing. 1.high fever (up to 106°F [41.1°C]) 2.serous nasal discharge 3.submandibular lymphadenopathy 4.dry, harsh, and nonproductive coughing 5.Depression 6.anorexia 7.weakness 1.Nasal discharge 2.although scant and serous initially but may become mucopurulent due to secondary bacterial infection 3.Anemia, leukopenia and lymphopenia 4.Increased neutrophil : lymphocyte ratio 5.Monocytosis 1.Virus isolation 2.Serologic tests 3.Pulmonary imaging 4.Thoracic radiographs Equine Herpesvirus Infection equine viral arteritis 1.Supportive treatment 2.NSAID 3.Antibiotics 4.Rest 1.Hygienic management 2.Vaccination
- 3. EquineViralArteritis Epizooticcellulitis Pinkeye Equinetyphoid Rotlaufseuche an acute, contagious, viral disease of equids ETIOLOGIC AGENT: Equine Arteritis Virus (EAV) EAV is present in equine populations in many countries worldwide, with the notable exceptions of Japan and Iceland. It is frequently highest in Standardbreds and Warmbloods. Transmission: Aerosolization of respiratory secretions Fomite contamination with respiratory secretions Venereal transmission Congenital transmission Incubation period: 7–19 days After intranasal challenge (aerosolization), the virus invades the respiratory tract epithelium and the alveolar macrophages. By 72 hours after infection, replicating viruses are detectable in the bronchopulmonar y lymph nodes, endothelium, and circulating macrophages. Dissemination of the virus by hematogenous routes allows infection of mesenteric lymph nodes; spleen; liver; kidneys; nasopharyngeal, pleural, and peritoneal fluid; and urine. By 6 to 8 days after infection, the virus has localized within the endothelium and medial myocytes of blood vessels, where it causes a necrotizing arteritis, a panvasculitis. The clinical Respiratory signs: 1.serous nasal discharge 2.Cough 3.Conjunctivitis 4.Lacrimation 5.palpebral and periorbital edema Gross lesions: (respiratory) Pulmonary edema emphysema interstitial pneumonia excess peritoneal, pleural, and pericardial fluid Microscopic lesions: Vasculitis (smaller arterioles and venules) seen in the placenta and the brain, liver, spleen, and lungs of the fetus 1.reverse transcriptase- PCR 2.Virus Neutralization Test 3.ELISA tests 4.Virus isolation 5.Immunohistoc hemical examination 1.Equine influenza 2.Equine herpesvirus 1 and 4– related diseases 3.Infection with equine rhinitis A and B viruses 4.Equine adenovirus es 5.Purpura hemorrhagi ca 6.Equine infectious anemia 7.Hoary alyssum toxicosis 8.African horse sickness fever 9.Getah virus infection 10.Dourine No Specific Antiviral Treatment Symptomatic treatment indicated only in severe cases. 1.Sound management practices 2.isolation of new arrivals 3.maintenance of pregnant mares in small i 4.solated groups 5.identification of carrier stallions 6.annual immunization of noncarrier breeding stallion populations 7.Vaccination
- 4. HendraVirusInfection EquineMorbillivirus Hendra virus (HeV) is the prototype species of a new genus Henipavirus within the subfamily Paramyxovirinae First recognized in Hendra, Australia in 1995 as a new zoonotic disease of horses Hendra virus is classified as a biosafety Level 4 agent defined as posing a high risk of life- threatening disease in humans Hendra virus infection and disease in horses has only been reported in Australia. with 13 events recorded between 1994 and 2009 Fruit bats are the reservoir of infection, and disease transmission requires very close contact with infected horses or bat droppings. Transmission: undetermined mechanism hypothetical route: through contact with food or water contaminated with material from infected bats Australian paralysis tick Ixodes holocylus. This tick is a blood feeder that feeds both on bats and horses Consumption of contaminated food or water Fomites Tissue tropism In Vascular tissues including pulmonary epithelium and capillaries Extensive destruction of pulmonary capillary endothelium The virus replicates within the upper and lower respiratory tract epithelium and causes an interstitial pneumonia. Pulmonary distress: fever (>104° F) depression tachycardia tachypnea sweating poor capillary refill abnormal lung sounds (caused by pulmonary edema) Neurologic deficits: ataxia head pressing recumbency Incubation period: 8 to 16 days or 4 to 10 days The time between the onset of signs until death is usually between 1 and 3 days. Respiratory lesions: Gross lesions 1.Severe edema and congestion of the lungs 2.Marked dilatation of the subpleural lymphatics. 3.Airways are filled with thick froth, which is often blood- tinged. Microscopic lesions 1.serofibrinous alveolar edema 2.hemorrhage 3.thrombosis of capillaries 4.necrosis of alveolar walls 5.alveolar macrophages are evident in the lungs. 1.RT-PCR 2.detection of viral RNA 3.immunoperoxi dase staining/ seroconversion 4.Virus Neutralization assay 5.ELISA Samples: blood sample nasal or oral swab 1.African Horse Fever 2.anthrax 3.botulism 4.certain bacterial infections 5.plant or chemical poisoning NONE minimizing contact with bat body fluids . Control 1.Euthanasia 2.deep burial of cases 3.monitoring 4.Isolation 5.movement restriction of in-contact animals 6.disinfection of potentially contaminate d surfaces.
- 5. AfricanHorseSickness Zebras are considered to be the natural vertebrate host and reservoir of the AHSV Culicoides imicola is considered to be the most important field vector for AHSV. The disease is limited geographically to areas of Africa, the Middle East, and Southern Europe. Once the virus gains entry into the host, it replicates in the regional lymph nodes before being spread hematogenously to most organs and tissues in the body. In the lungs, spleen, lymphoid tissues, and in certain endothelial cells, a secondary viral replication phase ensues. Incubation period from inoculation to secondary viremic phase is approximately 9 days. Acute form (Pulmonary Form) fever (up to 107° F) severe respiratory distress: tachypnea base-wide stance extended neck nostril flaring coughing Frothy white and, occasionally, blood-tinged fluid may be evident at the nostrils. The course of the disease is usually 4 to 5 days. The mortality rate for this form is 95%. Lesions are not pathognomonic for AHS Diagnostic Confirmation: Viral Isolation Or Identification PCR or by ELISA EVA Purpura Hemorrhagica Equine Infectious Anemia Babesiosis (Early Stages) No specific treatment Supportive and symptomatic treatment Vector control Restricting import of infected animals Slaughter of viremic animals Vaccination
- 6. Bacterial InfectionRhodococcusequiPneumonia Rhodococcus equi causes life- threatening pneumonia in foals between 1 and 5 months of age The bacterium has a worldwide distribution. Transmission: Inhalation of dust particles laden with virulent R. equi Swallowing of sputum laden with R equi =Inhalation of dust particles laden with virulent R = R. equi phagocytosed by macrophages = The replication of R. equi within macrophages ultimately results in the death of the host cell. = Large numbers of cells migrate to the site in response to infection with R. equi, ultimately resulting in granuloma formation. = inflammatory mediators may allow proliferation of organisms and cause the loss of pulmonary function. Anorexia Lethargy Febrile state Tachypnea Acute respiratory distress Fever Cough Diarrhea Crackles and wheezes (Thoracic Auscultation) Disease are difficult to detect until pulmonary infection reaches a critical mass The most common manifestation of R. equi infection in foals is chronic pyogranulomat ous bronchopneum onia with abscessation and associated suppurative lymphadenitis. 1. Bacterial culture Definitive diagnosis of R. equi pneumonia. 2. Thoracic radiography 3. Thoracic ultrasound 4. PCR Serologic testing agar gel immunodiffusion (AGID) enzyme-linked immunosorbent assay (ELISA) overdiagnosis of R. equi infection Supportive therapy 1.Judicial IV fluid therapy and 2.Nasal insufflation with oxygen 3.Bronchodila tor therapy 4.Prophylactic antiulcer 1.decrease exposure to the organism 2.elimination of environment al conditions that favor disseminatio n of the organism 3.early detection of clinical cases 4.Surveillance programs 5.passive immunity for neonatal foals
- 7. Strangles Distemper an infectious, contagious disease of Equidae characterized by abscessation of the lymphoid tissue of the upper respiratory tract. causative organism: Streptococcus equi equi a gram-positive, capsulated β- hemolytic Lancefield group C coccus, which is an obligate parasite and a primary pathogen. Worldwide in distribution Transmission: Direct horse-to- horse contact Indirect transmission includes S. equi enters through the mouth or nose and attaches to cells in the crypt of the lingual and palatine tonsils, as well as to the follicular- associated epithelium of the pharyngeal and tubal tonsils. Translocation occurs in a few hours to the mandibular and suprapharyngea l lymph nodes that drain the pharyngeal and tonsil region. Failure of neutrophils to phagocytose and kill the streptococci culminates in the accumulation of many extracellular streptococci in the form of long chains surrounded by large numbers of degenerating neutrophils. 1.fever (103–106°F [39.4–41.1°C]) 2.First sign of infection 3.mucoid to mucopurulent nasal discharge 4.depression 5.difficulty swallowing 6.inspiratory respiratory noise 7.extended head and neck. 1.submandibular lymphadenopat hy 2.compression of the dorsal pharyngeal wall 3.abscessation in other lymph nodes of the body - Metastatic strangles (“bastard strangles”) Abdomen and thorax , and brain 1.Clinical signs 2.Bacterial culture 3.polymerase chain reaction (PCR) 4.endoscopic examination of the upper respiratory tract 5.ultrasonograp hy 6.radiographic examination 1.Warm compresses 2.applied to sites of lymphadeno pathy to facilitate maturation of abscesses 3.povidone- iodine solution (3– 5% diluted) 4.NSAID 5.Antibacteria l 6.Administrati on of penicillin 1.Vaccination 2.Isolation 3.Sanitation and disinfection 4.Should wear protective clothing or change clothes before traveling to the next equine facility 5.Quarantine 14–21 days
- 8. Pleuropneumonia Pleuritis Pleurisy infection of the lungs and pleural space Develops secondary to bacterial pneumonia or penetrating thoracic wounds Worldwide in distribution occurring in all ages and both sexes. Predisposing factors. 1. Viral respiratory infection 2. long-distance transport 3. general anesthesia 4. strenuous exercise Suppresion impaired pulmonary defense mechanisms Invasion Bacterial colonization and infection of the lower airway, alveoli, and lung parenchyma Proliferation Influx of inflammatory cells (neutrophils) Tissue destruction Accumulation of cell debris in the alveoli and airways. Accumulation Extension of inflammation and infection. 1.Fever 2.Depression 3.Lethargy 4.Inappetence 5.Respiratory distress 6.Cough 7.Nasal discharge 8.Exercise intolerance 9.Reduced breath sounds) 10. Presence of pleural fluid 11. Pneumonia Hematologic lesions: 1.Leukocytosis w/ mature neutrophilia 2.Hyperfibrinog enemia 3.Hypoalbumine mia 4.Hyperglobulin emia 5.Pleural fluid: 6.Leukocytosis 7.Hyperproteine mia 8.Presence of intra- and extracellular bacteria 1.Thoracic ultrasonograp hy 2.Thoracocente sis 3.Thoracic radiography 4.Examination of pleural fluid 5.Cytologic evaluation 6.Bacterial culture and sensitivity 1.Intrathoracic neoplasia 2.Penetrating chest wounds 3.Esophageal perforation 4.Diaphragmati c hernia 5.Congestive heart failure 6.Hemangiosar coma 7.African horse sickness 8.Pulmonary hydatidosis 9.Pulmonary infarction and pneumonia 1.Antibiotic therapy 2.Thoracosto my 3.Pleural space drainage 4.Supportive care 5.intravenous fluid therapy, 6.nutritional support, 7.NSAID therapy. Reduction of risk factors associate with the disease FungalInfections FungalRhinitis Pythium insidiosum Occurs predominantly in the united states, occasionally in Australia, and rarely in other warm climatic regions. Respiratory stridor Exercise intolerance Chronic unilateral,purulent nasal discharge which may contain blood Numerous small granulating ulcers or fissures in the rostral part of the nasal cavity endoscopy Surgical excision Topical Amphotericin B Cryptococcus neoformans Mucopurulent and sanguinus and have a Granuloma formation Biopsy Cytology
- 9. foul odor Invasive rhinitis and sinusitis Draining tracts through the facial bones culture Aspergillus spp. Non-invasive Mild yellowish mucoid nasal discharge Invasive Scanty, foul smelling, unilateral, purulent discharge possibly containing blood Extensive destruction of the mucosa of the nasal turbinates and the maxillary or frontal sinuses Cell culture Topical treatment of eniconazole FungalPneumonia Blastomyces dermatidis Coccidoides immitis Cryptococcus neoformans Histoplasma capulatum inhalation of spores Inhalation of windborne arthrospores Chronic cough Nasal discharge Exercise intolerance Anorexia Weight loss Pleural effusion - Commonly seen in coccidiomycosis Radiography Ultrasonograph y Tracheobronch ial asporates Serological detection Antifungal drugs ( 10-12 weeks) For primary infection Should ideally be based on sensitivity testing ParasiticInfection Parascaris equorum Found in foals less than 4-6 mos. Old Productive cough Hyperpnea Loss of weight Overt pneumonia Endoscopic examination Fecalysis Dictyocaulu sarnfieldi Rarely affects horses Persistent, non- progressive coughing Tracheal aspiration Edoscopy Fecalysis
- 10. Echinococcusgranulosus generally well- tolerated in horses, and cysts in the liver and lung may be an incidental finding at post- mortem examination intermittent fever, depression, rapid shallow respiration, pectoral edema, large pulmonary or pleural cysts rupture, resulting in a large volume of pleural effusion. Ultrasound examination 1.albendazole (10 mg/kg, PO, SID x 30d) 2.thoracic drainage 3.surgical debridemen t of the pleura and cyst on the surface of the diaphragm DISEASE OTHER NAME DESCRIPTION ETIOLOGY/ EPIDEMIOLOGY PATHOGENESIS CLINICAL SIGNS LESIONS DIAGNOSIS DIFFERENTIAL DIAGNOSIS TREATMENT CONTROL AND PREVENTI ON MULTINODULAR PULMONARY FIBROSIS Interstitial pneumoni a/ Pulmonar y fibrosis heterogenous group of pulmonary disorders that produce pulmonary fibrosis in middle-aged to older horses toxins and idiosyncratic reactions Tachycardia; tachypnea, respiratory difficulty at rest, Lethargy fever weight loss. diffuse, severe, nodular interstitial pattern. Histopathologi c evaluation of biopsy anti- inflammatory medications; antibiotics; corticosteroids ; acyclovir INFLAMMATORYAIRWAYDISEASE Lower respirator y tract inflammat ion/ Small airway inflammat ory disease heterogeneous group of inflammatory conditions of the lower respiratory tract that appear to be primarily noninfectious allergic airway disease, recurrent pulmonary stress, deep inhalation of dust, atmospheric pollutants, and/or persistent respiratory viral infections develops after an overt viral respiratory infection and may result from inability of the immune system to fully eliminate viruses or bacteria from small airways chronic cough and mucoid to mucopurulent nasal discharge Slight swelling of myelin sheaths and Schwann cells with dilation of intraneural capillaries to heavy leukocytic infiltration of the nerves and necrosis Based on poor race performance and clinical signs. Systemic corticosteroid therapy, , aerosol administration of nedocromil sodium or an inhaled corticosteroid preparation (beclomethaso ne or fluticasone) Use low- dust bedding; Enhance ventilation; Avoid feeding dusty hay
- 11. EXERCISE-INDUCEDPULMONARY HEMORRHAGEINHORSES(EIPH) Epistaxis Bleeder occurs in most racehorses and is observed in many other horses used in equine sports that require strenuous exercise for short periods of time high pulmonary vascular pressures during maximal exercise, neovascularization secondary to pulmonary inflammation, and intrathoracic shear forces generated during exercise Results from thickening of pulmonary vein walls, resulting in decreased luminal diameter and increased intravascular pressure at the level of the pulmonary capillaries. epistaxis Endoscopic observation of blood in the airways 30–90 min after exercise provides definitive evidence of EIPH. cytologic examination of bronchoalveolar lavage, cytologic examination of bronchoalveolar lavage fluid, Thoracic radiography guttural pouch and ethmoid hematoma Flurosemide, Other vasodilators Application of nasal dilator bands reduces RBC counts in bronchoalve olar fluid from affected horses running on a treadmill by 33% LARYNGEALHEMIPLEGIAINHORSES Roaring/ Left laryngeal hemiplegi a Most common cause of abnormal inspiratory noise in the exercising horse. characterized by paresis or paralysis of the left arytenoid cartilage and vocal fold. It manifests clinically as exercise intolerance and inspiratory respiratory noise (“roaring”) during exercise -decreased airway sizes inspiratory noise during exercise exercise intolerance. Clinical signs; Endoscopic observation of reduced or absent mobility of the arytenoid cartilage and vocal fold. Arytenoid chondritis Prosteticlaryng oplasty, Laryngeal ;ventriculecto my performed via laryngotomy, or ventriculocord ectomy performed via transendoscopi c laser, improves airflow and reduces the “roaring” sound during exercise Prosthetic laryngopla sty is commonly done in racing horses and is the only technique that satisfactori ly reduces the impedance to inspiratory flow PHARYNGEAL LYMPHOID HYPERPLASIA pharyngiti s common condition of the dorsal pharyngeal wall observed in young horses (1–3 yr old) Result of exposure to novel antigens: bacteria, viruses, organic dusts, and other allergens Pharyngal pain Reduced appetite small foci or follicles of lymphoid tissue spread diffusely over the roof and lateral walls of the pharynx Endoscopic examination rest and NSAID administration are warranted in horses demonstrating pharyngeal pain.
- 12. DORSALDISPLACEMENTOFTHESOFTPALATE a performance- limiting condition of the upper respiratory tract and is a relatively common cause of upper respiratory noise during exercise the caudal free margin of the soft palate moves dorsal to the epiglottis, creating a functional obstruction within the airway. The cross-sectional area of the pharynx is reduced, and airflow resistance and turbulence are increased. Inflammation of the URT due to infection may cause neuropathy of the pharyngeal branch of the vagus n. as it traverses the floor of the medial compartment of the guttural pouch, resulting in neuromuscular dysfunction of the pharyngeal muscles that control the soft palate. The retropharyngeal lymph nodes are in direct gurgling respiratory noisecontact with the pharyngeal branch of the vagus nerve, and retropharyngeal lymphadenopathy may result in compression and irritation gurgling respiratory noise/ “choking down”; difficulty of breathing Based on clinical signs ; nasopharynge al endoscopy; lateral x-rays of the head. Rest and anti- inflammatory therapy; Sternothyrohy oideusmyecto my;Soft palate resection (staphylectomy
- 13. EPIGLOTTICENTRAPMENT a less common cause of respiratory noise and exercise intolerance the aryepiglottic fold completely envelops the apex and lateral margins of the epiglottis inspiratory and expiratory respiratory noise during exercise and poor exercise performance. Less common signs include cough, nasal discharge, and headshaking. Redundant folds, swollen and ulcerated epiglottis Endoscopic examination axial division of the aryepiglottic fold to free the epiglottis SUBEPIGLOTTICCYST an uncommon cause of respiratory noise in young horses. They are likely present from birth, but remain undetected until the horse begins exercise training Most commonly reported in thoroughbreds and standardbreds suspected to arise from remnants of the thyroglossal duct. respiratory noise; exercise ;intolerance Large cysts may produce coughing, dysphagia, and aspiration in foals. endoscopic examination of the upper respiratory tract Dorsal displacement of the soft palate complete removal of the secretory lining of the cyst FOURTH BRANCHIAL ARCH DEFECT Aplasia or hypoplasia of the extrinsic structure of the larynx respiratory noise, although mild dysphagia, eructation, and cough absence of one or both wings of the thyroid cartilage, Radiography; Endoscopic examination GutturalPouchEMPYEMA the accumulation of purulent, septic exudate in the guttural pouch Caused by bacteria primarily Streptococcus spp. intermittent purulent nasal dis charge, painful swelling in the parotid area, and in severe cases, stiff head carriage and stertorous breathing. Fever, depression, and anorexia swelling in the parotid area, endoscopic examination of the guttural pouch; radiography of the pharynx Systemic antimicrobial therapy; guttural pouch lavage and drainage; penicillin;
- 14. GUTTURALPOUCH TYMPANY Condition in young horses in which excessive air is trapped in the pouch(es) Foals are most commonly presented 2-4 months of age The affected guttural pouch is distended with air and forms a characteristic nonpainful swelling in the parotid region. Tympanitic swelling of the viborg region; resp. noise; cough;dysphagia is based on clinical signs and radiographic examination of the skull bronchopneum onia; Guttural pouch empyema Medical management with NSAID and antimicrobial therapy GUTURALPOUCH MYCOSISMycoticplaques inthegutturalpouchare typicallylocatedonthe caudodorsalaspectofthe medialgutturalpouch, overtheinternalcarotid artery Mycotic plaques in the guttural pouch are typically located on the caudodorsal aspect of the medial guttural pouch, over the internal carotid artery Etiology is fungi primarily aspergillus spp Clinical signs arise from damage to the cranial nerves and the arteries within the mucosal lining of the guttural pouch. epistaxis endoscopic examination of the guttural pouch topical and systemic antifungal therapy, based on sensitivity testing RUPTUREOFTHELONGUS CAPITISMUSCLE second most common cause (after mycosis) of severe hemorrhage from the guttural pouch The longus capitis muscle inserts into the basiphenoid and occipital bones Epistaxis;head tilt; nystagmus; ataxia swelling and hemorrhage can be seen in the most rostral and medial aspects of the guttural pouch; pharyngeal collapse Guttural pouch mycosis involves stall rest for 4–6 wk; broad- spectrum antibiotics are given for 5–7 days for any infection at the site of muscle rupture REFERENCES: http://www.thehorse.com/articles/28846/managing-inflammatory-airway-disease-in-horses-aaep-2011 Erica Larson, News Editor. March 16. 2012 Christa Lesté-Lasserre, 2013. www.horse.com Bianca Schwarz, PhD, DVM, Dipl. ECEIM, head of the Internal Medicine Service in the Equine Clinic of Altforweiler, Germany, and a former researcher at the Equine Clinic of the University of Vienna in Austria. T
