Cardiovascular and hemolynphatic diseases word printable
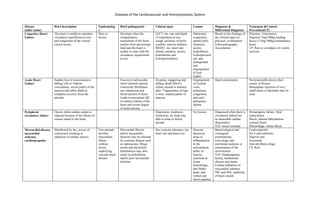
- 1. Diseases of the Cardiovascular and Hemolymphatic System Disease (other name) Brief description Epidemiolog y Brief pathogenesis Clinical signs Lesions Diagnosis & Differential Diagnosis Treatment &Control, Prevention(CP) Congestive Heart Failure The heart is unable to maintain circulatory equilibrium at rest and congestion of the venous circuit occurs. Rare in horses. Develops when the compensatory mechanism of the heart reaches their physiologic limit and the heart is unable to cope with the circulatory requirement at rest. LEFT: inc. rate and depth of respiration at rest, cough, presence of moist crackles, and inc dullness. RIGHT: inc. heart rate, edema, anasarca, ascites hydrothorax and hydropericardium. Pulmonary congestion, edema (left). Anasarca, ascites, hydrothorax, hydropericardi um, and enlargement and engorgement of liver (right). Based on the findings of the clinical signs on physical; examination. Echocardiography Auscultation Diuretics, Venesecton, Digoxin( 7mg/100kg-loading dose) (3.5mg/100kg-maintanance dose) CP: Rest or avoidance of violent exercise. Acute Heart Failure Sudden loss of consciousness, falling with or without convulsions, severe pallor of the mucosa and either death or complete recovery from the episode. Excessive tachycardia (short diastolic period, ventricular fibrillation (no contraction and blood ejection fr heart. Leads to precipitate fall in minute volume of the heart and severe degree of tissue anoxia. Dyspnea, staggering and falling, death follows within second or minutes after 1st appearance of sign is seen, marked pallor of mucosa. Engorgement of visceral veins, pulmonary congestion, and early pulmonary edema. Heart examination Not practicable due to short course of disease. Intracardiac injection of very small doses of adrenalin may be used. Peripheral circulatory failure Occurs when cardiac output is reduced because of the failure of venous return to the heart. Depression, weakness, listeleness, inc heart rate, falls in temp to below normal. No lesions. Diagnosed when there is circulatory failure but no detectable cardiac abnormality. D.D: severe toxemia Hematogenic failure: fluid replacement Shock; plasma Dehydration: isotonic fluids Hemorrhage: whole blood Myocardial disease, myocardial asthenia, cardiomyopathy Manifested by dec. power of contraction resulting in reduction of cardiac reserve. Few animals develop myocardial failure without severe underlying valvular heart disease. Myocardial fibrosis and/or myocardial function may be affected by systemic disease such as septicaemia. Drugs, toxins and electrolyte disturbances may also result in arrhythmias and/or poor myocardial function. Dec exercise tolerance, inc heart rate and heart size Discrete abscesses, areas of inflammation in the myocardium, pallor of muscle, petechial or linear hemorrhage, and flabby heart, thin walled and shows patches Bacteriological and virological examinations, toxicologic and nutritional analyses or examination of the environment D.D: Diaphragmatic hernia, mediastinal abscess and tumor. Cardiac dilatation of myocardial asthenia: INC and DEC audibility of heart sounds Corticosteroids Vit E and selenium, Digoxin and Frusemide Anti-arrythmic drugs CP: Rest
- 2. Diseases of the Cardiovascular and Hemolymphatic System of shrunken, tough fibrous tissue. Valvular disease Interferes with the normal flow of blood through the cardiac orifices causing murmurs and in severe cases,CHF. Degenerative valve disease (DVD) is seen in geriatric horses and also horses as young as 10 years of age. Murmurs and palpable thrills are caused by turbulence and eddying in blood flow and possibly also by the vibrations produced by abnormally directed flow impinging on the heart and vessel walls. Decreased cardiac output, Exercise intolerance, Cough, Increased heart rat Stenosis of the aortic valve, insufficiency of the aortic valve, stenosis and insufficiency of the pulmonary valve, insufficiency of the left and right atrioventricula r valve, and stenosis of the right or left atrioventricula rvalves. Recognition of an endocardial murmur. No specific treatment. endocarditis Inflammation of the endocardium may interfere with the ejection of blood from the heart by causing stenosis of the valves. May arise from implantation of bacteria onto the valves from the bloodstream or by bacterial embolism of the valve capillaries. It is also a common sequel on valve that are subject to flow-associated stressas the result of congenital cardiac defects. Subacute: persistent pyrexia, weight loss, lethargy, depression, lameness, septic/ nonspecific arthritis Acute: severe pyrexia, depression, reluctance to move, edema, jugular filling. Shrunken valves, distorted and thickened along edges. Mass in the valve orifice. Phonocardiography, echocardiography Blood culture D.D: Any and all causes of chronic inflammation and antigenic stimulation Antibiotics (erythromycin) Penicillin (50 000 IU/kg IV qid) combined initially with gentamicin. CP: Using an antimicrobial mouth wash to prevent bacterial infection Treatment of any infection with antibiotic therapy, especially in case of patients who already suffer from an existing heart condition or have artificial heart devices implanted
- 3. Diseases of the Cardiovascular and Hemolymphatic System pericarditis Inflammation of the pericardial sac. Pericarditis appears to be much less common in the UK than in the USA. This may be because pericarditis is sometimes associated with pleuro- pneumonia, which is more common in animals transported long distances overland between two climatic extremes. In early stages, it is accompanied by hyperemia and the deposition of fibrinous exudate which produces a friction rub when the pericardium and epicardiumrub together during cardiac movement. Pain, avoidance of movement, abduction of the elbows, arching of the back and shallow abdominal respiration. (Early stages). Fibrinous pericarditis: marked muffling of the heart sounds, tachycardia, distention of the jugular veins, and subcutaneous edema of the ventral body wall. Hyperemia of the pericardial lining and a deposit of fibrin, gas may be present, embolic abscesses. Electrocardiography Echocardiography Radiography Clinical pathology Antibacterial treatment of the specific infection. Broad spectrum antibiotics (sulfonamides) for non-specific treatment. Ventricular septal defect Subaortal defect occurring high in septum at the pars membranaceae. in one large study of congenital heart disease in dogs, a prevalence of 0.68% was noted; common defects included patent ductusarterios us (PDA, 28%), pulmonic stenosis (20%), subaortic stenosis (14%), persistent right aortic Shunting of blood from left ventricle into the right ventricle outseen tracts due to the higher pressure of the left ventricle, blood shunted into the right ventricle is recirculated thru the pulmonary vessels and left cardiac chambers, which cause dilatation of these structure. Lassitude, failure to grow well, and dyspnea. Echocardiography, catheterization, indicator dilation techniques D.D: Tricuspid regurgitation(adult). Foal Tricuspid dysplasia. Other congenital defects. No practical correction. Surgery, pulmonary artery banding, therapy.
- 4. Diseases of the Cardiovascular and Hemolymphatic System arch (8%), and ventricular septal defect (7%). Left atrioventricularval vular regurgitation( LAVR) Systolic murmur, severe dyspnea, tachypnea, cough, flaring of the nostrils. Acute: profuse, frothy, blood-stained discharged from nose Fibrous thickening Echocardiography Spectral and color film Doppler Ultrasound D.D: Chordal rupture, acute pulmonary edema, acute bronchospasm No treatment. Right atrioventricualrVal vularregurgitation (RAVR) Secondary consequence of generalized cardiac failure resulting from LAVR or bacterial endocarditis. Echocardiography Doppler ultrasound Aortic valvular regurgitation Backflow of blood from the aorta into the left ventricle due to insufficiency of the aortic semilunar valve. Causes include idiopathic valvular degeneration, rheumatic fever, endocarditis, myxomatous degeneration, congenital bicuspid aortic valve, aortic root dilatation or dissection, and connective tissue or rheumatologic disorders. Murmurs, regurgitation Nodules, bands plaques, fenestrations, holes in the margin of the valve cusps, Combination of auscultation, palpation of peripheral pulses, M- mode, two dimensional, and Doppler echocardiography. No specific treatment Aortic and pulmonic Stenosis Marked narrowing of its orifice. Either minor disruption of valvular structure that do not reduce the cross sectional area of the valve but cause disturbance of flow during systole. peripheral or ventral edema Echocardiography Cardiac catheterization. Tricuspid atresia/ atrial septal defect Consistent opening of the interatrial septum, which allows blood to shunt from the atrium with the greater pressure. Blood shunts from the left atrium to the right atrium, causing a volume overload of the right sided chambers. Poor growth rate, lethargy, severely limited exercise tolerance, cyanosis, and intense pan systolic shunt type of murmur. Blood gas analysis, echocardiography, contrast studies, angiocardiography, electrocardiography, catheterization D.D: Tetralogy of Fallot myocarditis Active inflammation of the heart muscle thatmaybe parasite, viral or bacterial in origin. Myocardial disease is often suspected when an arrhythmia develops after Exercise intolerance, dyspnea in exertion, gallop sound, arrhythmia, Cellular infiltrate- devoid Enzymology, echocardiography X-rays, EKG's, and echocardiograms CP: Preventative strategies to
- 5. Diseases of the Cardiovascular and Hemolymphatic System an infectious disease, such as strangles or influenza. When the heart muscle becomes inflamed, it loses strength and contracts less forcefully. The bacteria Streptococcus equi is the chief cause of myocarditis. neutrophils. reduce the likelihood of heart disease are, so far, limited to avoiding in-breeding, not breeding animals with known congenital defects of any kind, and not breeding horses that have acquired a heart disorder relatively early in life, as this may indicate a strong genetic component (with increased susceptibility in offspring). Ionophore toxicity This type of intoxication involves specific feed additives used as growth-promoting agents in cattle and as coccidiostats in poultry and other birds. Horses are highly susceptible. . Death is possible less than 24 hours after ingestion. Horses surviving the initial intoxication, or horses with chronic exposure, may show progressive signs of congestive heart failure due to irreparable cardiac muscle damage, as well as poor growth and poor weight gain. A number of cases of sudden death in the weeks or months after intoxication have been reported Acute: abd. Pan, diarrhea, severe dyspnea Per acute: inc swelling with inc urine output, hypovolemic shocks Sub-acute: depression, reduce feed intake, cardiac arrhythmias, tachycardia, hyperventilation Chronic: unthriftiness, cardiac dysfunction, reduced exercise intolerance. Toxic tubular nephritis and hepatitis, paleness, subcutaneous and pulmonary edema, congestion and hemorrhage, inc pleural, abdominal, and pericardial fluid. Ionophore poisoning is diagnosed by identifying ionophore content in the stomach. Thin-layer chromatography is used to make this identification and can be used to link ionophores to feed products. No specific treatment for ionophorepoisoning is known, but supportive care includes oral administration of activated charcoal in acute cases to block intestinal absorption. Although treatment success is rare, aggressive fluid therapy supports cardiac and kidney function, and correction of electrolyte abnormalities with supplemental potassium is advised. CP: Because most ionophorepoisonings involve contaminated or poorly mixed feeds, it's imperative that horse owners deal with reputable feed companies and that quality assurance programs be in place and enforced in all mills that produce equine nutritional product Pericardial effusion Effusive pericarditis results in right-sided CHF when the pressure within the pericardium rises so that it exceeds that within the heart, restricting diastolic filling of the cardiac chambers. The low-pressure RA is the first chamber to collapse under the pressure of the intra- pericardial fluid. This limits venous return. The increase in filling pressure leads to venous congestion and the limited preload means that cardiac output cannot be raised to meet Triad of tachycardia, muffled heart sounds, and venous hypertension. Auscultation, echocardiographic examination, pericardiocentesis D.D: Pleural disease Pericardiocentesis Anti-inflammatory therapy CP: Controlling inflammation and sepsis.
- 6. Diseases of the Cardiovascular and Hemolymphatic System any increased demands. The greater the pressure within the pericardium, the higher the pressure required to fill the RA and ventricle. The rate at which the effusion develops also affects the severity of the condition, because the pericardium can stretch to accommodate larger volumes of fluid if it accumulates slowly. If an acute effusive episode occurs, the fibrous sac will have little time to dilate and intra- pericardial pressure will be high. HEMOLYMPHATIC DIISEASES Blood Loss Anemia/Hemorrha gic Anemia Results from decrease circulating blood volume and associated hypovolemic shock. Severe hemorrhage usually is due to loss of vascular integrity which may result from iatrogenic or accidental trauma or from erosion of vessel walls by neoplastic or parasitic lesion Common causes of external hemorrhage caused by large vessel rupture include castration complication or accidental trauma. Epistaxis due to nasal surgery or guttural pouch mycosis Hemophilia Major effects of hemorrhage are loss of blood volume, loss of plasma proteins and erythrocytes. If rate of blood is rapid the loss of circulating blood volume results to peripheral circulatory failure and anemic anoxia results from loss of erythrocytes. Tachycardia, tachypnea, pale mucous membranes, prolonged jugular filling. Progressive exercise intolerance, muscular weakness and collapse Decreased organ perfusion can cause oliguria and ileus Extreme pallor of all tissues and a thin watery appearance of blood Physical examination to discern clinical signs of hemorrhage and to differentiate them from other signs of abdominal, thoracic or musculoskeletal diseases. Auscultation, percussion, centesis and percutaneous ultrasonography are useful ancillary diagnostic aids. Diagnostic work-up like platelet count and clotting process D.D: Shock and dehydration External hemorrhage is controlled with direct pressure or large vessel ligation Surgical intervention to identify and control sides of internal hemorrhage. Use of anti-fibrinolytic agents epsilon-aminocaproic acid and tranexamic acid is used to treat post-partum uterine artery hemorrhage IV administration of 0.37% formaldehyde to treat uncontrolled hemorrhage. IV crystalloids solution should be administered at 40-60ml/kg to provide cardiovascular support. Administration of hypertonic saline and colloid solution Whole blood transfusion Hemolytic Anemia Equine infectious A retroviral disease Retroviruses contains Acute form = fever, Thrombocyto Coggins test which is an No vaccine available
- 7. Diseases of the Cardiovascular and Hemolymphatic System Anemia characterized by chronic episodic and hemolytic anemia RNA-directed DNA polymerase which gives virus the ability to incorporate into host genome of infected macrophage It is transmitted through transfer of blood by interrupted feeding of arthropods like horse flies and deer flies can also be transferred through use of blood contaminated instruments. Tran’s placental transfer can happen. The virus is tropic for macrophage and act like ‘Trojan Horse’ providing latency after viral replication particles are released from the macrophage into surrounding extracellular milieu thus introducing a cycle of viral amplification within the host Hyperplasia of lymphoreticular system and hyperhemoglobulinemia develop. Hemolysis is considered to result from immune complex attachment to RBC via a viral hemagglutinin with subsequent extravascular removal of cells by the mononuclear phagocytic system. depression, thrombocytopenia that is clinically represented by mucosal petechiation Chronic form (more than 30 days) = anorexia, ventral edema, episodic fever spikes, abdominal pain, ataxia, abortion or infertility penia during acute phase with anemia and icterus developing during sub acute to chronic phases of disease Leucopenia with lymphocytosis and monocytosis Hyperglobulin emia, increase serum liver enzyme activities and proteinemia may develop agar gel immunodiffusion assay ELIZA CP: Absolute attention to restriction of blood transfer or blood-related material Isolation of no less than 200 yards from other horses and double screening in a stable environment Babesiosis caused by intraerythrocytic protozoan parasite of genus Babesia
- 8. Diseases of the Cardiovascular and Hemolymphatic System it is tick borne transmitted and causes intravascular hemolysis Phenothiazine Poisoning Oxidants like phenothiazines, onions or wilted red maple leaves damage erythrocyte Causes hemoglobin to become denatured with subsequent disulfide bond formation. Oxidized hemoglobin forms precipitates called Heinz bodies. These cell change result in increased fragility of cells with subsequent intravascular hemolysis Oxidative damage causes increase permeability of membrane, thereby altering ion transport mechanism and osmotic gradient. Tissue hypoxia secondary to methynoglobinemia Fever, tachycardia, tachypnea, lethargy, intense icterus, hemoglobinuria with characteristic brown coloration of skin and mucous membrane Anemia, increase mean corpuscular hemoglobin, free plasma hemoglobin, anisocytosis, increased RBC fragility, variable presence of Heinz bodies, neutrophilia Hyperkalemia, hyperglycemia, metabolic acidosis Laboratory evidence of oxidative damage Reducing fragility of erythrocyte, maximizing oxygenation Maintaining venal perfusion Providing supportive care Activated charcoal (8-24mg/kg up to 2.2kg PO) Ascorbic acid to maintain cellular a-tocopherol in reduced form and as scavenger of free radicals Oxygen Isoerythrolysis in foals/ Neonatal Isoerythrolysis develops when there are blood group incompatibilities between the mare and foal, particularly when the foal has the Aa or Qa red cell antigens and the mare does not. The mare becomes sensitized to the foal’s alloantigen and alloantibodies are concentrated in colostrum. When the affected foal ingest colostrum within 24 hours of birth , the hemolysitc antibody is absorbed along with other immune globulins and hemolytic anemia develops foals may die within 24 hours of life or may develop signs 24-96 hours after colostrum ingestion === tachypnea, depression, icterus and progressively developing anemia anemia, elevated icterus index, increase total serum bilirubin concentration, hemoglobinuri a and biliribinuria Direct Coomb’s test provides a presumptive diagnosis of NI Direct Immunofluorescence assay using cytometry supportive care, particularly placement of foal in quiet,cool environment,. Blood transfusion in severe anemia Autoimmune Hemolytic Anemia Primarily idiopathic condition or secondary to infection, drug administration or neoplasia Primary IMHA (autoimmune hemolysis) results from loss of self-tolerance and is relatively rare Secondary IMHA results from adherence of cross-reacting Production of autoantibodies to red cells, resulting in increased destruction of red cells by lysiserythrophagocytosis. The primary antibodies involved are IgGangIgM. Extravascular hemolysis Spherocytes may be present in cytology of peripheral blood smear Agglutination will suggest surface bound antibody Direct and indirect Coombs test Whole blood transfusion Antimicrobial therapy is required when sepsis is confirmed Immunosuppressive therapy may be considered Administration of Dexamethasone at 0.05 to 0.2mg/kg IV at 24 hour
- 9. Diseases of the Cardiovascular and Hemolymphatic System antibodies to erythrocyte surface antigen The presence of these molecules on RBC causes intravascular destruction by complement activation (IgM-mediated)-or most commonly extravascular removal of macrophage Toxin exposure due to snake bites from rattle snakes Piriplasmosis A tick-borne disease of horses resulting from infection with protozoan Babesiacaballi and theileriaequi. Babesiacaball i is transmitted transovarially from one tick generation. Vector of theileriaequi is dermacentorni tens which transfer the protozoa horizontally. Apparent in first 1-4 weeks of infection and include fever, depression anorexia, weakness, ataxia, lacrimation, mucoid discharge, chonosis, icterus, hemoglobinuria and potentially death Observation of parasitized erythrocytes with giemsia stained blood smears Isolation of the organism from blood or serology Complement fixation test or indirect fluorescent antibody test PRC Administration of imidocarb to reduce parasite load Equine Ehrlichiosis Caused by rickettsial organism (Erhlichiaequi) Fever, depression, petechiae, ventral edema, ataxia with reluctance to move Granulocytopenia, anemia, thrombocytopenia are detected on hematology Indirect Fluorescent antibody test PRC Should be differentiated with purpurahemorrhagica, equine viral arthritis and encephalitis Supportive care with NSAIDS therapy, Lower limb sweat wraps IV oxytetracycline for clearance Anemia Secondary to Inadequate Erythropoiesis Anemia of Chronic Disease Can be caused by chronic suppurative processes, radiation injury, poisoning bracken, thrichlorethylene-extracted soy Pleuropnemonitis Internal abscessation Peritonitis Chronic organ failure Presence of a chronic disease process accompanied by a mild to moderate, non- Related to eliminating the underlying disease condition and to ensuing that the anemia is not caused by blood loss or hemolysis
- 10. Diseases of the Cardiovascular and Hemolymphatic System bean meal, arsenic, phenylbutazone causes depression of bone marrow Immune-mediated or granulomatous disease Neoplasia Chronic viral disease such as Equine infectious Anemia regenerative, normochromic and normocytic anemia. Serum ion and total iron binding capacity is decreased can be demonstrated by normal serum Ferritin concentration or positive Prussian blue stain for marrow iron. Nutritional Deficiency Inadequate erythropoiesis caused by dietary inadequacy. Vitamin B12 and folic acid are important cofactors in erythrocyte maturation. Can also be caused by copper, cobalt and iron deficiency Iron-deficiency anemia is diagnosed on the basis of hypoferritemia, hypoferremia, normal to increased total iron- binding capacity and detection o decreased iron stores in examination of bone marrow aspirates Supplementation with iron Thrombocytopenia Caused by reduced platelet production, abnormal platelet distribution, and increased consumption or decreased platelet survival It causes altered hemostasis due to insufficient phospholipid substrate for coagulation proteins. The platelet plug localizes activated clotting factors and maintains vascular integrity, thus spontaneous hemorrhage from developing Hemorrhagic diathesis caused by small vessels bleeding and represented by petechiation, although ecchymosis of the ocular, oral, nasal or vaginal mucous membranes may be observed. Epistaxis, hyphema, microscopic hematuria or spontaneous hemorrhage may develop when the platelet concentration falls below 10,000/ul Confirmation of a decreased platelet count (<100,000/ul) Identification of surface-associated IG molecules on peripheral platelets using direct immunofluorescence and flow cytometry D.D: DIC, bone marrow disease or IMTP should be suspected No treatment available for primary bone marrow megakaryocyte hypoplasia Whole blood or platelet rich plasma transfusion Dexamethasone (0.05-0.1mg/kg IV) to decrease Fc binding, phagocytic removal and antibody production Hemostatic Diseases Can be inherited or acquired The most common acquired coagulation disorders in the hoses are Immune mediated Vasculitis and disseminated intravascular coagulation. Unexpected bleeding after minor trauma or surgery Petechial, and ecchymoses, hyphema, epistaxis, melena, hematoma, and hemorrhage Hemarthrosis, hemoabdomen, and Recognition of clinical signs and basic laboratory test Performing platelet count Measurement of activated partial thromboplastin time
- 11. Diseases of the Cardiovascular and Hemolymphatic System hemothorax can occur Clinical signs associated with hypercoagulation include jugular vein thrombosis or thromboembolic disease that affects the GIT, pulmonary, renal, and cerebral or the digital vasculature (APTT; intrinsic and common pathways), fibrin degeneration products concentration and fibrinogen Hemophilia A (Factor VIII Deficiency) Caused by a deficiency of factor VIII and is the most common inherited coagulation disorder Only occur in males and their life expectancy is short (6 months to 3 years) presence of unexpected, recurrent hemorrhage in a young male with an abnormally prolonged APTT and reduced factor VIII:C activity administration of fresh plasma can temporarily replace the clotting factor deficiency but the effect only last for hours to days Von Willebrands Disease Caused by quantitative or qualitative defects in von Willebrand factor. This result in a defect in platelet plug. epistaxis and bleeding from skin or mucous membranes after mild trauma or surgery specific assays for vWF= ELIZA Prekallikrein Deficiency A contact factor that becomes activated when plasma interacts with a negatively charged surface that initiates the intrinsic coagulation cascade minimal to excessive hemprrhage after castration Protein C deficiency It results in hypercoagulable state of horses recurrent venous thrombosis, nephrolithiasis and severe renal disease Acquired Coagulation Disorder Disseminated Intravascular Coagulation Most common hemostatic dysfunction in horse Acquired process in which activation of coagulation causes widespread fibrin deposition in the microcirculation resulting in ischemic damage to tissues. Hemorrhagic diathesis occurs as a result of consumption of procoagulants or hypersensitivity of fibrinolysis In DIC, antithrombin III and protein C become depleted as a result of overzealous activation of coagulation. This results in excessive, unchecked thrombin and clot formation, which in turn activates plasmin. FDPs are formed when plasmin degrades fibrin. As the FDPs begin to accumulate in the Range from mild thrombosis and ischemic organ failure to petechiae and hemorrhage Petechial or ecchymotic hemorrhages of the mucous membranes or sclerae, epistaxis, hyphema, and melena can occur Hypoperfusio n and microvascular thrombosis lead to focal or widespread tissue damage and culminates in colic, laminitis, and signs of renal, pulmonary Presence of clinical sigs – thrombocytopenia, prolonged APTT and PT, and increase in FDP concentration Intravenous fluid therapy to maintain tissue perfusion and combat shock. If septic process is present, antimicrobials are indicated Minimizing the effects of entotoxemia may attenuate the disease process. Flunixinmeglumine will mitigate the detrimental effects of eicosanoids Fresh plasma therapy is indicated with severe hemorrhage
- 12. Diseases of the Cardiovascular and Hemolymphatic System circulation, they contribute to the coagulopathy by inhibiting thrombin activity and by causing platelet dysfunction and cerebral disease Warfarin and Sweet Clover Toxicosis Horses may develop hemorrhagic diathesis after consumption of warfarin for for therapeutic reasons like treatment of thrombophlebitis and navicular disease, rodenticides, or moldy sweet clover Sweet clover hay or silage that is improperly cured can contain dicumarol Dicumarol and warfarin competitively inhibit vitamin K, which is essential for the production of clotting factors II, VII, IX, X. Hematomas, hematuria, epistaxis, and ecchymoses of mucous membranes Based on history of exposure and laboratory data. Clinical pathology reflects prolonged PT first because the plasma half-life of factor VII is shorter than the other clotting factors. Discontinuation of the drug Treatment with vitamin K Polycythemia/ erythrocytosis Is an increase in RBC mass. Relative polycythemia or hemoconcentration, is common in horses and occurs when plasma volume is decreased because of conditions such as dehydration or endotoxemia. Splenic contraction may cause transient polycythemia Absolute polycythemia indicates an increased red cell mass in the absence of plasma volume change. Primary absolute polycythemia occurs when red cell mass increase without concurrent increase in erythropoietin concentrations Lethargy, weight loss, and mucosal hyperemia Increased blood viscosity impairs oxygen delivery to tissues when packed Cell Volume exceeds 60%. Abnormal pigmentation, epistaxis, tachycardia, and tachypnea Based on the measurement of persistently increased PCV, hemoglobin concentration and red blood cell count in the face of normal plasma volume. Phlebotomy is indicated when the PCV remains persistently above 50%. 10 to 20 ml of blood/kg are removed and replaced by an equal volume of balanced polyionic fluid. Lymphoproliferati ve and Myeloproliferative Disorder 1. Lymphom a A general term denoting malignant transformation of lymphoid cells, but is often used in equine medicine in place of the term lymphosarcoma which is the malignant transformation of lymphoid cells into solid tumors Lymphoid leukemia denotes Decreased appetite, depression, weight loss, fever, lymphadenopathy and dependent edema Numerous lymphoma tumor locations include peripheral and internal lymph nodes, spleen, liver, kidneys, Physical examination through transrectal abdominal palpation and careful thoracic auscultation and percussion. Observation of the neoplastic cells in aspirates or biopsy Immunosuppressive glucocorticoid therapy may be palliative for steroid-responsive malignancies and may also suppress immune-mediated sequelae including hemolytic anemia and thrombocytopenia Use of multiple-agent induction protocol in horses with
- 13. Diseases of the Cardiovascular and Hemolymphatic System malignant transformation of lymphoid cells within the bone marrow Etiology unknown intestines, heart, lung nasopharynx, eye and adnexia skeletal muscle, skin, reproductive organs and central and peripheral nervous systems. specimens of lymph nodes and other masses or in centesis, samples of body cavity fluids, bone marrow aspirates, or peripheral blood lymphoma. Cytosine arabinose, chlorambucil, prednisone are used. 2. Plasma Cell Myeloma Plasma cells are terminally differentiated B-cell lymphocytes Malignant transformation can result in 3 categories tumors: chronic B cell Lymphocytic leukemia, B-cell lymphoma, and plasma cell tumors Limb edema, ataxia, lameness, epistaxis, lymphadenopathy, weight loss, and anorexia Secondary infections commonly involve the lower respiratory or urinary tract may develop Anemia and hyperglobulin emia are common abnormal laboratory findings. Definitive diagnosis is based on th demonstration of bone marrow plasmacytosis Skeletal survey radiographs of the long bones and cervical vertebrae and biochemical tests to detect renal or hepatic involvement. Most horses die or are euthanized within 4 months of developing clinical signs. Melphalan, prednisone, and cyclophosphamide areused 3. Myeloid Leukemia Characterized by medullary and extramedullary proliferation of bone marrow constituents including the erythroid, granulocytic, monocytic and megakaryocytic cell series Occurs in ages ranged from 10 months to 16 years and in both genders Ventral and peripheral edema, petechial, weight loss, depression, and enlarged lymph nodes Thrombocytopenia and anemia can occur Bone marrow examination Cytosine arabinose based o a low- dose protocol The aim of this therapy is to promote terminal differentiation of the neoplastic cell line and diminish clonal expansion
- 14. Diseases of the Cardiovascular and Hemolymphatic System Vasculitis An inflammation and necrosis of blood vessel walls, can affect any size, location or type of vessel in any age, breed or sex of horses. The mechanism of issue damage in immune- mediated vasculitis is thought to be caused by a type III hypersensitivity reaction in which soluble immune complexes are deposited in blood vessel walls in areas of increased vascular permeability. Activation of complement by immune complexes releases complement and other compounds that are chemotactic for neutrophils. Proteolytic enzymes released by infiltrative neutrophils directly damage vessel walls Edema of the skin and subcutaneous tissue, distal extrimities, face, and ventral abdomen Serum leakage, and crusting may occur Necrosis of affected areas result in ulceration and or sloughing of the skin Mucous membranes and sclerae are often hyperemiv and have multiple petechiae and ecchymoses Definitive diagnosis is made from the history, clinical signs and skin biopsy results Histopathologic findings of hypersensitivity vasculitis are infiltration of neutrophils, the presence of neutrophil nuclear debris and fibrinoid necrosis of affercted dermal vessels Direct Immunofluorescence test Removing the antigenic stimulus, suppressing the immune-response, reducing vessel wall inflammation and providing supportive care. Systemic glucocorticoids are warranted because purpurahemorrhagica and other undefined vasculitides are most likely immune-mediated Splenomegaly may occur for many reasons relating to neoplasia, equine infectious anemia, salmonellosis, and rarely anthrax primary spleenomegaly may also occur as a result of cogestion secondary to spleenic cirrhosis, cardiac failure, or active sequestration of erythrocytes
