Via aérea dificil
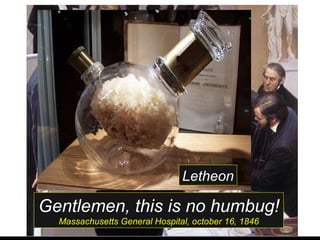
- 1. Gentlemen, this is no humbug! Massachusetts General Hospital, october 16, 1846 Letheon
- 2. PABLO BRAGA GUSMAN Mestre e Doutor em Anestesiologia, UNESP Research fellowship, Pitié Salpêtrière, Paris Secretário da Sociedade de Anestesiologia do ES II Simpósio de Anestesia Ambulatorial Itaigara Memorial Hospital Dia Via aérea difícil em cirurgia ambulatorial
- 3. Via aérea difícil em cirurgia ambulatorial AUSÊNCIA DE DECLARAÇÃO DE POTENCIAL CONFLITO DE INTERESSE De acordo com as normas: CFM: 1595/2000 e RDC 102/2000
- 4. 78,5% 6,4% 4,5% 7% 4% 18,5%
- 5. Oxímetro de pulso / capnografia
- 7. Manejo das Vias aéreas
- 17. Oxigênio é essencial para a vida! Mas também não permita hipercarbia! A irway: abrir vias aéreas B reathing: ventilação com pressão positiva C irculation: compressões torácicas D isability: acesso a lesões neurológicas
- 18. PROCEDIMENTO DISPOSITIVO FLUXO de O2 L / min CONCENTRAÇÃO DE OXIGENIO Sem oxigênio suplementar Boca a boca N/A 16% Boca - máscara N/A 16% Bolsa / válvula / máscara N/A 16%
- 19. PROCEDIMENTO DISPOSITIVO FLUXO de O2 L / min CONCENTRAÇÃO DE OXIGENIO Com oxigênio suplementar Cánula nasal 1-6 24-30% Boca – máscara 10 50% Máscara facial simples 8-10 40-60% AMBU sem reservatório 8-10 40-60% Máscara simples com reservatório 6 60%
- 20. PROCEDIMENTO DISPOSITIVO FLUXO de O2 L / min CONCENTRAÇÃO DE OXIGENIO Com oxigênio suplementar AMBU com reservatório 10-15 90-100% Máscara com reservatório sem recirculação 10-15 90-100% Com válvula de demanda De acordo com a fonte 90-100%
- 29. (Recommandé par la Soc Française Anésthésie Réanimation) Lista de equipamentos para intubação dificil Lista mínima Lista completa - Laringoscópio - Laringoscópio - Guias maleáveis - Guias maleáveis - Mascara laríngea - Guia luminoso (Trachlight) - Oxigenação transtraqueal - Mascara laríngea - Intubação retrograda - Fastrach - Oxigenação transtraqueal - IOT retrógrada - Fibroscopia bronquica
- 31. # Sempre confirmar ventilação (com tubo traqueal ou Máscara Laríngea) com CO 2 expirado (capnografia ou colorimétrico).
- 47. Reynolds, CHEST 2005
- 55. Can Succinylcholine Be Abandoned? Cook, D. Ryan MD Volume 90(5S) Supplement, May 2000, pp S24-S28 Nonneuromuscular Blocking Effects: Dysrhythmias Pulmonary Edema and Hemorrhage Intragastric Pressure Intraocular Pressure Hyperkalemia and Myoglobinemia Hyperkalemic Cardiac Arrest and Occult Myopathies Malignant Hyperthermia and Masseter Spasm
- 61. Efficacy of sugammadex for the reversal of rocuronium-induced blockade: a pooled analysis of dose-response studies - Holanda Pharmacokinetics of rocuronium and sugammadex in patients with normal and impaired renal function. – Holanda Reversal of profound rocuronium-induced neuromuscular blockade is significantly faster with sugammadex than with neostigmine- EUA Sugammadex reversal of profound rocuronium-induced neuromuscular block is significantly faster than spontaneous recovery from succinylcholine- EUA A prospective randomised double blind study to evaluate the effect of infusion of amino acid enriched solution on recovery from neuromuscular blockade produced by vecuronium bromide and atracurium besylate - India Effect of higher than required doses of sugammadex on recovery from rocuronium-induced block in guinea pigs - Escócia Sugammadex (2.0 mg/kg) reverses shallow rocuronium-induced neuromuscular blockade significantly faster than neostigmine (50 g/kg)- Alemanha
- 65. Grupo de discussão AnestesiaDor : http://br.groups.yahoo.com/group/anestesiador/ http://blogdoanestesiador.blogspot.com http://www.twitter.com/anestesiador
Hinweis der Redaktion
- In order to assess and minimize adverse outcomes related to airway management, ASA developed the Task Force on Management of the Difficult Airway. This task force then produced the "Practice Guidelines for Management of the Difficult Airway." It is stated that the "purpose of these guidelines is to facilitate management of the difficult airway and to reduce the likelihood of adverse outcomes."1 This was approved by the ASA House of Delegates on October 21, 1992, and became effective July 1, 1993. The difficult airway algorithm produced by this effort can now be found in essentially every anesthetizing location in use today. Difficult airway management can have a tremendous impact on patient outcome as well as the anesthesia care provider. In order to assess the management of tough airway scenarios, the ASA Closed Claims Project created a supplemental difficult airway data collection form that focused on the principles of the ASA difficult airway algorithm. At present, there are 98 closed claims from 1987-95 involving management of a difficult airway for which this data form was completed. As there is generally an average of five years between the actual event and the claim reaching the ASA Closed Claim Project database, nearly all of these 98 cases took place prior to the formal adoption of the ASA difficult airway guidelines. However, the presence of these guidelines did not change what was (and is) considered to be the standard of care in the management of the difficult airway. We therefore reviewed the management of these cases as described below.
- Em meados da década de 90, em uma segunda avaliação dos eventos de natureza respiratória do ASA Closed Claims Project, observous-e uma expressiva redução na ocorrência de casos devidos à ventilação inadequada que pode justamente ser atribuída à mais ampla utilização de recirsaos de monitorização como oximetria de pulso e capnografia a partir dessa época.
- To avoid catastrophes secondary to difficult intubations, any patient that may require intubation should first undergo a historical and physical airway exam if the situation allows. AIRWAY HISTORY : If possible, attain and review prior anesthesia records. Ask the patient: about problems with prior anesthesia such as jaw pain, hoarse voice, dental injury – any thing that may suggest the anesthesiologist had difficulty intubating or providing positive pressure ventilation or that the patient has an anatomic abnormality. if they have ever been informed by an anesthesiologist that they were difficult to intubate or ventilate. if they have dentures, sleep apnea, TMJ problems or history of prior airway surgery or trauma (including burns). if they have a history of head and neck tumors or infection. PHYSICAL EXAM : Your physical exam will be your most reliable tool for anticipating difficulties in airway management. Start by reviewing vital signs, particularly oxygen saturation. Then, commence your exam with a general assessment: is the patient obese or morbidly obese? do they appear to have a short chin or an over-bite? are there any signs of previous head, neck or thorax surgery? is the patient pale or cyanotic? is the patient able to sit up? is the patient breathing comfortably? does the patient require supplemental oxygen? is the patient appropriate and able to follow commands? does the patient have full range of motion of the neck? In addition to a cardiovascular and pulmonary exam, a focused airway exam should be conducted. Detailed evaluation and documentation of pre-procedure abnormalities is imperative: examine the mouth and oral cavity (the best combination for east airway management is a large oral cavity with a small mobile tongue) evaluate the extent and symmetry of mouth opening (three finger breadths is optimal) check for loose, missing or cracked teeth note any prominent buck teeth or particularly large incisors that may interfere with laryngoscopy (dental and oral injuries are common complications of laryngoscopy) note the size of the tongue (large tongues may interfere with use of the laryngoscope) note the arch of the palate (high arched palates have been known to hamper visualization of the larynx) examine the chin: the two important features of the chin include mandibular space and tissue compliance. Predicted airway risk is low if the thyromental space (distance from the mandible to the thyroid) is three finger breadths or greater and tissue compliance is high. examine the pharynx. The appearance of the posterior PHARYNX may predict ease of laryngoscopy and visualization of the LARYNX . Malampatti has classified patients in classes I-IV based on visualization of structures during pre-operative evaluation. The patient is asked to open the mouth wide, stick out the tongue, and extend the neck to allow for maximal visualization of the PHARYNX . If the whole of the tonsillar pillars are visualized, the airway is rated Class I and intubation is likely to be uncomplicated. If the uvula, but not the tonsillar pillars can be visualized, the airway is rated as Class II. Class III is characterized by visualization of part of the uvula and soft palate. An airway is characterized as Class IV if the tongue obstructs view of any structures beyond the hard palate. Class IV is associated with increased risk of difficult intubation.
- PHYSICAL EXAM : In addition to a cardiovascular and pulmonary exam, a focused airway exam should be conducted. Detailed evaluation and documentation of pre-procedure abnormalities is imperative: examine the mouth and oral cavity (the best combination for east airway management is a large oral cavity with a small mobile tongue) evaluate the extent and symmetry of mouth opening (three finger breadths is optimal) check for loose, missing or cracked teeth note any prominent buck teeth or particularly large incisors that may interfere with laryngoscopy (dental and oral injuries are common complications of laryngoscopy) note the size of the tongue (large tongues may interfere with use of the laryngoscope) note the arch of the palate (high arched palates have been known to hamper visualization of the larynx) examine the chin: the two important features of the chin include mandibular space and tissue compliance. Predicted airway risk is low if the thyromental space (distance from the mandible to the thyroid) is three finger breadths or greater and tissue compliance is high. examine the pharynx. The appearance of the posterior PHARYNX may predict ease of laryngoscopy and visualization of the LARYNX . Malampatti has classified patients in classes I-IV based on visualization of structures during pre-operative evaluation. The patient is asked to open the mouth wide, stick out the tongue, and extend the neck to allow for maximal visualization of the PHARYNX . If the whole of the tonsillar pillars are visualized, the airway is rated Class I and intubation is likely to be uncomplicated. If the uvula, but not the tonsillar pillars can be visualized, the airway is rated as Class II. Class III is characterized by visualization of part of the uvula and soft palate. An airway is characterized as Class IV if the tongue obstructs view of any structures beyond the hard palate. Class IV is associated with increased risk of difficult intubation.
- APPROACH TO THE AIRWAY IN TRAUMA PATIENTS: The A of ABC The most immediately life threatening complication of any trauma is loss of airway patency. Maintaining oxygenation and preventing hypercarbia are critical in managing the trauma patient, especially if the patient has sustained a head injury. Thus, the first step in evaluating and treating any trauma patient is to assess airway patency and, if compromised, restore it: the A of A (airway), B (breathing), C (circulation). Any patient who is awake, alert and able to talk has a patent airway. Whether they need supplemental oxygen can be determined by vitals and physical exam. Patients who are unconscious or have signs suggestive of respiratory compromise, however, require immediate attention.
- Oxigenoterapia suplementar Some patients require oxygen supplementation, despite maintaining a patent airway and normal ventilatory drive. In such cases devices such as nasal cannula, face tents and simple masks can be used to deliver oxygen via positive pressure. The nasal cannula (plastic tubing inserted into nares) is the most commonly employed low-flow oxygen delivery device. It provides supplemental oxygen at flows ranging from 0 to 8 L/min, enabling a maximum of 40% O2 to be delivered. The oxygen concentration (FIO2) can be estimated by adding 4% per liter of O2 delivered. For greater oxygen delivery in a patient with a patent airway, a reservoir systems such as a simple mask, which covers the nose and mouth and can provide flow rates of 10L/min and a maximum FIO2 of 55% to be delivered, and a non-rebreather mask, which uses a series of one way valves and can deliver 10-15 L min and a maximum FIO2 of 80%. High flow systems, such as nebulizers, can also be used for increased oxygen delivery.
- Connaître les principes de l’organisation d’un bloc opératoire pour la prise en charge de l’intubation difficile en tenant compte des recommandations de la conférence d’experts 2006. Connaître les limites de la prédiction de l’intubation difficile et savoir organiser l’intubation difficile imprévue. Savoir organiser, dès la consultation d’anesthésie, la prise en charge de l’intubation difficile prévue. Savoir mettre en place l’algorithme d’oxygénation et connaître les formations permettant de s’assurer de la performance des différents acteurs. Connaître la problématique de la gestion du matériel d’intubation difficile et des endoscopes souples bronchiques. Savoir intégrer cette organisation dans une démarche de qualité du service incluant matériels, organisation et enseignement.
- La problématique et les axes d’amélioration L’organisation du bloc opératoire Tous les personnels travaillant dans ce type de structure ont leur part de responsabilité dans l’organisation. L’enquête de 1999 sur la mortalité anesthésique en France a mis en évidence le rôle des facteurs humains et organisationnels impliqués dans les décès liés à l’anesthésie [1] : - organisation : mauvaise orientation du patient et programmation chirurgicale inadéquate ; - absence de protocole ; - facteurs individuels : manque d’expérience ou de compétence, erreurs de jugement ou d’analyse ; facteurs de groupe : problèmes de communication et absence de leader. Ce sont les facteurs individuels (contribution relative de 51 %) et plus encore les facteurs de groupe (contribution relative de 62 %) qui étaient retrouvés comme facteurs de mortalité anesthésique.
- La consultation d’anesthésie : le dépistage pour s’organiser Le texte long “Prédiction et définition de la ventilation au masque difficile et de l’intubation difficile” et le texte court de la conférence d’experts ID exposent clairement les éléments de dépistage et permettent donc de définir un état d’alerte permettant l’optimisation de la prise en charge des voies aériennes du patient [4, 5] : “Le dépistage de l’intubation difficile (ID) et de la ventilation au masque difficile (VMD) doit être systématique et documenté chaque fois qu’une intubation est prévue ou probable (consultation d’anesthésie, admission en réanimation)”. Les critères recommandés sont : - les antécédents d’ID ; - la classe de Mallampati supérieure à 2, distance thyromentonnière inférieure à 6 cm et ouverture de bouche inférieure à 35 mm ; la recherche de la mobilité mandibulaire (test de morsure de lèvre) ; - la mobilité du rachis cervical (angle fait par la tête en extension maximum sur le cou et en flexion maximum supérieur à 90°) ; - ainsi qu’un IMC supérieur à 35 kg/m2, un syndrome d’apnées obstructives du sommeil avec tour de cou supérieur à 45,6 cm, une pathologie cervico-faciale et un état prééclamptique.
- Cette stratégie doit aussi tenir compte de la prédiction de la ventilation difficile au masque facial [4, 5, 8] : “L’âge supérieur à 55 ans, un index de masse corporelle (IMC) supérieur à 26 kg/m2, l’absence de dents, la limitation de la protrusion mandibulaire, la présence d’un ronflement et d’une barbe ont été retrouvés comme facteurs prédictifs d’une VMD. La présence de deux de ces facteurs est prédictive d’une VMD.
- Le nombre nécessaire d’essais avant d’avoir un taux de succès satisfaisant (“courbe d'apprentissage”) a été évalué pour la plupart des techniques mais cette évaluation a porté généralement sur des patients sans difficulté d’accès aux voies aériennes et dans des conditions optimales. - La ventilation au masque facial est difficile à apprendre par des néophytes puisque le taux de succès est inférieur à 50 % après dix tentatives [34]. - L’intubation trachéale est également difficile à apprendre puisque le taux de succès n’est de 90 % qu’après 57 tentatives avec 18 % des enseignés nécessitant encore une aide après la 80e tentative [35]. Une évaluation plus récente confirme cette donnée avec un taux de succès de 90 % après 47 tentatives [23]. Toutefois, l’introduction des vidéo-laryngoscopes [36, 37] modifie l’enseignement de l’intubation en permettant à l’enseignant de suivre chacun des gestes de l’enseigné, comme lors de l’enseignement de la fibroscopie. - L’apprentissage de l’insertion d’un masque laryngé est plus facile et plus rapide : 94 % de succès dès la première expérience [38] et plus de 97 % dès la seconde lors de la réanimation de patients en arrêt cardiaque [39], aucun échec après un enseignement théorique et sur mannequin et huit tentatives sur patient [18]. Néanmoins, la maîtrise technique de la mise en place d’un masque laryngé n’est pas la seule exigence : contexte médical, appréciation de la profondeur de l’anesthésie. -
- -Un minimum de vingt tentatives est nécessaire pour l’apprentissage de l’insertion d’un masque laryngé Fastrach® [40]. - L’évaluation de la courbe d’apprentissage de l’intubation facilitée par la fibroscopie est compliquée par les divers critères de succès retenus : dix tentatives sont nécessaires pour réaliser une intubation en moins de deux minutes dans 90 % des cas [41], dix-huit tentatives sont nécessaires pour réaliser une intubation en moins d’une minute dans 70 à 80 % des cas [42]. L’extrapolation de cette dernière étude conduit à considérer que l’on peut atteindre le niveau d’un “expert” après 45 intubations facilitées par la fibroscopie [42]. L’enseignement sur patient non sédaté est plus simple car il n’y a pas de limite dans le temps et moins de risques d’obstruction des voies aériennes supérieures que chez un patient sédaté. Il était la règle [43] mais l’amélioration des techniques de sédation modifie cette attitude dans certaines équipes. Une étape intermédiaire avant l’apprentissage de l’intubation facilitée par la fibroscopie sur patient sédaté peut être la naso-fibroscopie [44] et la fibroscopie bronchique diagnostique, examens réalisés sous anesthésie locale sous le contrôle d’oto-rhino-laryngologistes et de pneumologues entraînés.
- Le premier principe est d’envisager à chaque étape d’un algorithme la possibilité de réveiller le patient et de reporter, voire d’annuler, l’intervention. Le deuxième principe est d’avoir prévu à l’avance un algorithme décisionnel afin que l’attitude adoptée suive une démarche logique, adaptée à la situation, et aux compétences techniques de l’anesthésiste-réanimateur. Le troisième principe consiste à prévoir les conditions de sécurité du patient.
- Techniques de contrôle des voies aériennes Avant de procéder à l’intubation du patient, deux questions majeures se posent : - Existe-t-il une lésion du rachis cervical ? - Quelle voie d’intubation choisir : orale ou nasale ? Le dogme de l’intubation nasotrachéale en cas de lésion du rachis cervical suspectée ou avérée est remis en question car cette voie peut être difficile et présente certains inconvénients (Tabl. II) . La voie nasotrachéale peut être pratiquée dans de rares cas, chez certains polytraumatisés coopérants ayant une ventilation spontanée, ne présentant pas de lésions cranio-faciales complexes, et chez qui une anesthésie locale de très bonne qualité peut être effectuée. Malgré son apparente facilité, cette technique requiert du temps pour sa réalisation et, surtout, de l’expérience pour sa réussite.
- Os Estiletes Ópticos Visuais incorporam a visualização de imagem por fibroscopia, juntamente com o pequeno diâmetro e a forma dos estiletes de intubação clássicos (guia iluminado, guias metálicos, “bougies”) amplamente conhecidos. O estilete óptico Shikani (SOS) combina a função de estilete luminoso com fibroscópio nos tamanhos adulto e pediátrico. É constituído por um tubo de aço inoxidável maleável com 4.3 mm de diâmetro com sua ponta em forma de “J”. Dispõe de um sistema duplo de fibra óptica interno, um capaz de carrear luz e outro para visualização. Um fixador móvel com um encaixe para o conector do TT, ajusta a posição deste tubo no estilete, e ao mesmo tempo serve para administrar O2 diretamente ao seu interior. O conjunto é selado, possibilitando sua limpeza e esterilização. O estilete óptico tem basicamente as mesmas indicações do estilete luminoso convencional: intubação acordado, situações de VAD onde após indução da anestesia a intubação por laringoscopia direta não for possível, mas que ainda se possa ventilar o paciente sob máscara facial. Técnica: 1) Lubrificar o estilete e aplicar substância anti-embaçante na lente distal ou mergulhar sua ponta em água quente por alguns minutos. 2) Posicionar o estilete no interior do TT. lente distal não deve ultrapassar a ponta do TTposicionar a lente distal a 5mm do bisel 3) O operador traciona a mandíbula usando a mão esquerda, muitas vezes a tração da língua também facilita a intubação. 4) Inserir o estilete + TT na orofaringe pela rima labial direita e avançar sempre na linha média até alcançar a hipofaringe. 5) Sob visão direta, a ponta do estilete é introduzida por entre as cordas vocais. 6) Soltar o TT de seu fixador, e deslizar o TT pelo estilete até a traquéia sob visão direta. 7) Remover o estilete e confirmar a intubação. Lembretes importantes: A dificuldade técnica mais comumente encontrada com o uso dos estiletes ópticos é sua inserção muito profunda, geralmente se direcionando ao esôfago. A epiglote deve ser inicialmente identificada como ponto de referência. Após ultrapassar a epiglote, geralmente as cordas locais já são visualizadas. Caso não se consiga identificar estruturas de referência, como a epiglote, cordas vocais ou anéis traqueais, é indicado a retração do estilete e o reinicio de todo o processo. Uma maior extensão do pescoço pode ser útil.
- Laringoscópios Articulados Possuem uma articulação regulável no engate do corpo com a lâmina, o que permite a mudança deste ângulo, e com isso, um acesso mais fácil em pacientes obesos ou com gigantomastia. McCoy É um tipo especial de lamina de laringoscópio com ponta articulada, de forma a melhorar a exposição da laringe. Útil em casos de laringoscopia difícil, onde comparativamente às laminas convencionais, leva a uma melhor exposição da laringe em casos Cormack-Lehane graus II e III, mas não com os de grau IV.
- São laringoscópios que dispõe de um sistema de fibra-óptica rígida combinado a lâminas curvas e retráteis, que permitem a intubação com o paciente em posição neutra. Possibilitam a visualização da abertura glótica mesmo quando há dificuldade no alinhamento dos eixos oro-faríngeo e faringo-traqueal. Úteis em casos de laringoscopia difícil e principalmente quando não se deseja movimentação cervical, como nos pacientes com espodilite anquilosante, instabilidade cervical, artrite severa, limitação na abertura bucal. Como todos os dispositivos com fibra óptica, o campo visual já restrito é sujeito a limitações na presença de secreção ou sangue.
- Techniques de contrôle des voies aériennes La voie orale avec séquence d’induction rapide est requise dans la majorité des cas et s’effectue en plusieurs phases : l’installation, la préoxygénation, l’induction, la manoeuvre de Sellick, puis l’intubation trachéale du patient. L’installation est marquée par le positionnement de la tête (en haut à + 30 à 40° ou en bas), par l’évacuation du contenu gastrique avec une sonde, celle-ci pouvant être enlevée ou laissée en place selon les auteurs, cette manoeuvre permettant aussi de vérifier le bon fonctionnement du dispositif d’aspiration. La préoxygénation est réalisée avec une FiO2 de 100 % pendant 3 à 5 minutes ou par 4 inspirations profondes (correspondant à la capacité vitale), ce qui permet une dénitrogénation équivalente à celle de la préoxygénation habituelle en l’absence de pathologie respiratoire préexistante. La manoeuvre de Sellick est débutée lors de l’induction et poursuivie jusqu’au moment où la sonde d’intubation est en place et le ballonnet gonflé. Certains patients peuvent être hypoxémiques malgré la préoxygénation et peuvent nécessiter la ventilation au masque avant l’intubation afin de prévenir une majoration de cette hypoxémie ; dans ce cas, la manoeuvre de Sellick devra être effectuée lors de la ventilation afin de prévenir toute insufflation gastrique. Les agents anesthésiques pour l’induction doivent être choisis en fonction de l’état clinique du patient, en particulier hémodynamique, avec un hypnotique comme le thiopental, la kétamine, l’étomidate, le midazolam ou le propofol, et un curare, la succinylcholine.
- Techniques de contrôle des voies aériennes La préoxygénation est réalisée avec une FiO2 de 100 % pendant 3 à 5 minutes ou par 4 inspirations profondes (correspondant à la capacité vitale), ce qui permet une dénitrogénation équivalente à celle de la préoxygénation habituelle en l’absence de pathologie respiratoire préexistante.
- Techniques de contrôle des voies aériennes Preinduction Drugs Stimulation of the airway with a laryngoscope and endotracheal tube presents an extremely noxious stimulus,39 which is associated with an intense sympathetic discharge resulting in hypertension and tachycardia (called the pressor response ). The physiologic consequences of this pressor response are well-tolerated by healthy persons undergoing elective intubation. A hypertensive response, however, may induce myocardial and cerebrovascular injury in critically ill patients with limited reserves for adequate tissue oxygenation.2 Moreover, critically ill patients who require emergent intubation experience hypoxia, hypercarbia, and acidosis, which induce an extreme sympathetic outflow that is associated with tachycardia, labile BP, and an increased myocardial contractility.40 Attenuation of these physiologic physiologic stresses after the placement of an airway may unmask relative hypovolemia and/or vasodilation, which result in postintubation hypotension.40 Endotracheal intubation also can provoke bronchospasm and coughing that may aggravate underlying conditions, such as asthma, intraocular hypertension, and intracranial hypertension. Patients who are at risk for adverse events from airway manipulation benefit from the use of preinduction drugs, which include opioids, lidocaine, -b-bloqueadores como antagonistas adrenérgicos (Synergistic with fentanyl; most commonly used for neurosurgical patients with raised intracranial pressures; limited but growing experience in isolated head trauma in the emergency department), and non-depolarizing neuromuscular blockers (Elevated intracranial/intraocular pressure; prevention of succinylcholine-induced myalgia)
- Induction Agents Induction agents are used to facilitate intubation by rapidly inducing unconsciousness. Familiarity with a range of induction drugs is important because the specific clinical circumstance dictates the appropriate induction method (Table 3). Agents that are indicated for patients with respiratory failure may be contraindicated in other clinical settings. Intensivists should, therefore, avoid using a single standardized induction approach. Etomidate is a nonbarbiturate hypnotic agent that is used for the rapid induction of anesthesia. This imidazole derivative has a rapid onset of action and a short half-life. It predictably does not affect BP. Etomidate has cerebral-protective effects by reducing cerebral blood flow and cerebral oxygen uptake (V˙ o2). It does not, however, attenuate the pressor response that is related to intubation or provide analgesia. Adverse effects of etomidate include nausea, vomiting, myoclonic movements, lowering of the seizure threshold in patients with known seizure disorders, and adrenal suppression.43,49,61–63 Etomidate, even after a single bolus dose, inhibits cortisol production in the adrenal gland at various enzymatic levels and reduces adrenal responsiveness to exogenous adrenal corticotrophin hormone for up to12 h.49,64 Deleterious effects of etomidate-induced adrenal suppression have not been established after a single induction dose. Because of its rapid onset, short half-life, and good risk-benefit profile, etomidate has become the primary induction agent for emergency airway management. It is especially useful for patients with hypotension and multiple trauma because it does not alter systemic BP. Propofol is a rapid-acting, lipid-soluble induction drug that induces hypnosis in a single arm-brain circulation time. The characteristics of propofol include a short half-life and duration of activity, anticonvulsive properties, and antiemetic effects. Propofol reduces intracranial pressure by decreasing intracranial blood volume and decreasing cerebral metabolism.65,66 These mechanisms may underlie the improved outcomes with the use of propofol that have been demonstrated in patients with traumatic brain injury who are at risk of raised intracranial pressure.42,63,67 At doses that induce deep sedation, propofol causes apnea and produces profound relaxation of laryngeal musculature. This profound muscular relaxation effect allows propofol, when used in combination with a non-depolarizing NMBA (rocuronium) or opioids (remifentanil or alfentanil) to produce intubation conditions that are similar to those obtained with succinylcholine.68–71 However, we continue to favor its use with succinylcholine to ensure adequate intubating conditions. Propofol facilitates RSI, to a greater degree than etomidate, because it provides a deeper plane of anesthesia, thereby attenuating any effects of incomplete muscle paralysis.38 The most important adverse effect of propofol is drug-induced hypotension, which occurs by reducing systemic vascular resistance and, possibly, by depressing inotropy.63 Hypotension usually responds to a rapid bolus of crystalloid fluids and can be prevented by expanding intravascular volume before giving propofol or by pretreating patients with ephedrine.72 Some patients with allergies to soy or eggs may experience hypersensitivity reactions to propofol. Propofol has no analgesic properties. For hemodynamically stable patients who have either a contraindication to succinylcholine or receive non-depolarizing neuromuscular blockers for paralysis, propofol may be the induction agent of choice. Many clinicians use propofol as an induction drug for patients with isolated head injury or status epilepticus. Ketamine, a phencyclidine derivative, is a rapidly acting dissociative anesthetic agent that has potent amnestic, analgesic, and sympathomimetic qualities. Ketamine acts by causing a functional disorganization of the neural pathways running between the cortex, thalamus, and limbic system.49 It does so by selectively inhibiting the cortex and thalamus while stimulating the limbic system. Ketamine is also a unique induction agent because it does not abate airway-protective reflexes or spontaneous ventilation. 49 The central sympathomimetic effects of ketamine can produce cardiac ischemia by increasing cardiac output and BP, thereby increasing myocardial V˙ o2. Patients can experience “emergence phenomena” as they resurface from the dissociative state induced by ketamine. This frightening event, characterized by hallucinations and extreme emotional distress, can be attenuated or prevented with benzodiazepine drugs. Because ketamine is a potent cerebral vasodilator, intracranial hypertension is a contraindication for its use. Other side effects include salivation and bronchorrhea, both of which can be prevented with the administration of an anticholinergic agent such as glycopyrrolate or scopolamine. The bronchodilator properties of ketamine make it suitable for patients with bronchospasm due to status asthmaticus or COPD. No outcome studies exist, however, to demonstrate improved outcomes in these clinical settings. The sympathomimetic effects of ketamine warrant avoiding its use in patients with acute coronary syndromes, intracranial hypertension, or raised intraocular pressure. Sodium thiopental is a thiobarbiturate with a rapid 30-s onset of action and a short half-life. Its use for RSI is limited because it is a controlled substance and propofol has similar characteristics. Barbiturates in general decrease cerebral V˙ o2, cerebral blood flow, and intracranial pressure. They are associated, however, with hypotension secondary to the inhibition of CNS sympathetic outflow, which results in decreased myocardial contractility, systemic vascular resistance, and central venous return.63,73 Hypovolemia accentuates barbituate-induced hypotension. Sodium thiopental, therefore, should not be used as an induction agent in patients who have hypovolemic or distributive shock. The central sympatholytic effect induced by barbiturates has a positive effect in its blunting of the pressor response to intubation. 58,74,75 Barbituates cause allergic reactions in 2% of patients, and also induce laryngospasm, hypersalivation, and bronchospasm.63 Just as barbiturates are generally not used in the ICU for sedation purposes, they are not used to the same extent for emergency airway management. Sodium thiopental is rarely used in the ICU for emergency intubation, although it has applications for normotensive, normovolemic patients who have status epilepticus or require intubation prior to entering barbiturate coma for the control of intracranial hypertension. Scopolamine is a muscarinic anticholinergic agent with a short half-life that has sedative and amnestic effects, but no analgesic properties. It can cause tachycardia but otherwise produces no hemodynamic consequences.74 Scopolamine induces less tachycardia, however, compared with other available muscarinic agents ( eg , atropine and glycopyrrolate). 49 This hemodynamic profile makes scopolamine a preferred induction agent for patients with uncompensated shock when RSI is used. Adverse effects include psychotic reactions in addition to tachycardia and occur related to the dose administered. 49 Scopolamine causes profound papillary dilation, complicating neurologic evaluations. NMBAs NMBAs are used to facilitate laryngoscopy and tracheal intubation by causing profound relaxation of skeletal muscle. There are two classes of NMBAs, depolarizing and non-depolarizing (Table 4). Both classes act at the motor end plate. These drug classes differ in that depolarizing agents activate the acetylcholine receptor, whereas non-depolarizing agents competitively inhibit the acetylcholine receptor. NMBAs have no direct effect on BP.
- Nonneuromuscular Blocking Effects^ Succinylcholine can have a profound cardiovascular effect; can increase intraocular, intragastric, and intracranial pressure; and can be associated with hyperkalemia, myoglobinemia, and malignant hyperthermia. Dysrhythmias.^ Succinylcholine exerts variable and paradoxical effects on the cardiovascular system. Given IV, succinylcholine produces initial bradycardia and hypotension, followed after 15–30 s by tachycardia and hypertension. In the infant and small child, profound sustained sinus bradycardia (50–60 bpm) is often observed ( 1 ); rarely asystole occurs. Nodal rhythm and ventricular ectopic beats are seen in approximately 80% of children given a single IV injection of succinylcholine; such dysrhythmias are rarely seen after IM injection. In adults and in children, the incidence of bradycardias and other dysrhythmias are more frequent after a second dose of succinylcholine. Atropine offers protection against these bradyarrhythmias in all age groups. Pulmonary Edema and Hemorrhage.^ We have seen several young children who developed fulminant pulmonary edema within minutes after IM succinylcholine ( 2 ). It responded to continuous positive pressure ventilation. We speculate that this may represent a hemodynamic form of pulmonary edema from acute elevation of systemic vascular resistance and an acute decrease in pulmonary vascular resistance. Intragastric Pressure.^ Succinylcholine may increase intragastric pressure. The increase is directly related to the intensity of muscle fasciculations and, in adults, pressures as high as 40 cm H2O have been recorded. When the intragastric pressure exceeds 20 cm H2O, the cardioesophageal sphincter mechanism may become incompetent and regurgitation and aspiration may occur. Intraocular Pressure.^ Succinylcholine increases intraocular pressure (IOP) in both children and adults ( 3 ). Although dilation of choroidal vessels is a contributory factor, the major increase in IOP is caused by contraction of extraocular muscles. The IOP begins to increase within 60 s, peaks at 2–3 min, then decreases to control in 5–7 min after succinylcholine administration. In the presence of a penetrating wound of the eye, the increased IOP can result in extrusion of vitreous and possible loss of vision. In the patient with glaucoma, there may be a falsely elevated IOP, which may lead to unnecessary surgery if tonometry is performed within 5–7 min after succinylcholine. Hyperkalemia and Myoglobinemia.^ In normal adults, succinylcholine increases plasma potassium concentration by 0.3–0.5 mmol/L ( 4 ). More modest increases are seen in children ( 5 ). Alarming levels, as high as 11 mmol/L, along with cardiovascular collapse, have been reported with succinylcholine in a variety of situations including burns, massive trauma, stroke, and spinal cord injury. Myoglobinemia and elevation of plasma creatine phosphokinase concentration are commonly seen in prepubertal children after succinylcholine even in the absence of fasciculations ( 6,7 ). However, the myoglobinemia appears to be of minimal clinical importance. Hyperkalemic Cardiac Arrest and Occult Myopathies.^ In 1992, the Malignant Hyperthermia Association of the United States and the North American Malignant Hyperthermia Registry received reports of cardiac arrest in apparently healthy children given succinylcholine ( 8 ). Many of these children were boys with undiagnosed Duchenne dystrophy or unspecified myopathy, and most of the arrests were associated hyperkalemia. The label for succinylcholine was revised in November 1993 and March 1995 to restrict the elective use of succinylcholine in children ( 9 ). Cardiac dysrhythmias occurred abruptly at a median of 18 min and included wide complex bradycardia, ventricular tachycardia with hypotension, ventricular fibrillation, and asystole. Peaked T waves were rare although hyperkalemia was common (serum K+ 7.4 ± 2.8 mmol/L). Massive rhabdomyolysis was rare. Malignant Hyperthermia (MH) and Masseter Spasm.^ The incidence of MH in patients anesthetized with volatile anesthetics and given succinylcholine has been estimated at 1:4,000 to 1:40,000. The typical patient develops profound rigidity or violent fasciculation, increase in heart rate, a rapid increase in temperature, and in increase in Petco2. Trismus is rare and it is uncertain whether isolated trismus is uniformly associated with MH, but trismus or masseter spasm accompanied by rigidity of the entire body may be associated with a high incidence of MH. There is a high incidence of less intense masseter muscle rigidity after succinylcholine administration in children, but the clinical implications of this condition are not clear. A transient increase in jaw stiffness or in the resting tension of jaw muscles is a normal response to succinylcholine, and is more frequent in children anesthetized with halothane than with thiopental.
- Sugammadex is a novel selective relaxant binding drug (SRBA) which antagonizes or reverses steroidal nondepolarizing NMBDs, especially rocuronium. Sugammadex is likely the most exciting drug in clinical neuromuscular pharmacology since the introduction of atracurium and vecuronium in the middle 1980s. Of special interest is its novel and innovative mechanism of action. For over 30 yr, this author and several other investigators had many lengthy conversations and small meetings
- Figure 4. Panel A shows the recovery of the twitch height and train-of-four (TOF) ratio after administration of 1.2 mg/kg rocuronium followed 3 min later by 16 mg/kg sugammadex, both given IV. Recovery to a first twitch height (T1) of 90% and a TOF ratio of 0.94 occurred 110 s later. The onset-offset time with this sequence (i.e., the time from the end of the injection of rocuronium to a T1 recovery to 90%) was 4 min 47 s. Panel B shows the effects of administering 1.0 mg/kg succinylcholine (Sch) with spontaneous recovery to a T1 of 90% occurring after 9 min and 23 s. Abstract Sugammadex is a revolutionary investigational reversal drug currently undergoing Phase III testing whose introduction into clinical practice may change the face of clinical neuromuscular pharmacology. A modified -cyclodextrin, sugammadex exerts its effect by forming very tight water-soluble complexes at a 1:1 ratio with steroidal neuromuscular blocking drugs (rocuroniumvecuroniumpancuronium). During rocuronium-induced neuromuscular blockade, the IV administration of sugammadex creates a concentration gradient favoring the movement of rocuronium molecules from the neuromuscular junction back into the plasma, which results in a fast recovery of neuromuscular function. Sugammadex is biologically inactive, does not bind to plasma proteins, and appears to be safe and well tolerated. Additionally, it has no effect on acetylcholinesterase or any receptor system in the body. The compound’s efficacy as an antagonist does not appear to rely on renal excretion of the cyclodextrin-relaxant complex. Human and animal studies have demonstrated that sugammadex can reverse very deep neuromuscular blockade induced by rocuronium without muscle weakness. Its future clinical use should decrease the incidence of postoperative muscle weakness, and thus contribute to increased patient safety. Sugammadex will also facilitate the use of rocuronium for rapid sequence induction of anesthesia by providing a faster onset-offset profile than that seen with 1.0 mg/kg succinylcholine. Furthermore, no additional anticholinesterase or anticholinergic drugs would be needed for antagonism of residual neuromuscular blockade, which would mean the end of the cardiovascular and other side effects of these compounds. The clinical use of sugammadex promises to eliminate many of the shortcomings in our current practice with regard to the antagonism of rocuronium and possibly other steroidal neuromuscular blockers. (Anesth Analg 2007;104:575–81) Sugammadex is a novel and unique compound designed as an antagonist of rocuronium and possibly other steroidal neuromuscular blockers. This investigational drug is currently in Phase IIIa multicenter trial in the United States, and is likely to be introduced to the market in the future. In this article, I address the unique characteristics of sugammadex and offer a vision for how this drug is likely to change anesthesia practice. HISTORICAL PERSPECTIVE The cornerstone of modern neuromuscular pharmacology was laid more than seven decades ago when the chemical theory of the role of acetylcholine in neuromuscular transmission was established by Dale (1,2). The first successful administration of curare to produce surgical relaxation in an anesthetized patient had occurred in 1912, when Arthur La¨wen, a German surgeon from Leipzig, used a partially purified preparation of the substance (3). La¨wen’s findings were subsequently ignored for nearly three decades until January 23, 1942, when Enid Johnson, following Harold Griffith’s instructions, administered a total of 5 mL of curare IV to a 20-year-old man who had been anesthetized with cyclopropane via a facemask for an appendectomy. The anesthesia lasted for 70 min and was later described as being “nothing less than dramatic” (4). It was without a doubt, a revolutionary step and a milestone that changed anesthetic practice. However, when this technique was initially used, patients were not fully paralyzed, and the pharmacological antagonism of the residual neuromuscular blockade of curare was hardly considered (5). Tracheal intubation and controlled ventilation were also uncommon in routine clinical practice. The clinical use of neuromuscular blockers in anesthesia has come a long way since then. Since the 1980s, we have witnessed the introduction of many new From the Department of Anesthesiology and Pain Medicine, Unit 409, Anderson Cancer Center, The University of Texas M. D., Houston, Texas. Accepted for publication August 24, 2006. Address for correspondence and reprint requests to Mohamed Naguib, MB, BCh, MSc, FFARCSI, MD, Department of Anesthesiology and Pain Medicine, Unit 409, The University of Texas M. D., Anderson Cancer Center, 1400 Holcombe Boulevard, Houston, TX 77030. Address e-mail to naguib@mdanderson.org. Copyright © 2007 International Anesthesia Research Society DOI: 10.1213/01.ane.0000244594.63318.fc Vol. 104, EFFECT OF SUGAMMADEX ON OTHER DRUGS Sugammadex is ineffective against succinylcholine and benzylisoquinolinium neuromuscular blockers, such as mivacurium, atracurium, and cisatracurium (44), because it cannot form inclusion complexes with these drugs. Therefore, if neuromuscular blockade must be re-established after using sugammadex, succinylcholine or one of the benzylisoquinolinium neuromuscular blockers should be considered. Under these conditions, what would be the potency of cisatracurium and succinylcholine? Sugammadex binds at a 1:1 ratio to rocuronium and vecuronium, but for effective reversal, all rocuronium or vecuronium molecules do not have to be complexed with sugammadex. The margin of safety of the neuromuscular transmission is such that only 20%–25% of postsynaptic receptors need to be free for transmission to occur (47). Therefore, sugammadex only has to reduce the occupation of these receptors from 100% to 70% to obtain complete reversal. After induction of neuromuscular blockade with rocuronium and complete reversal with sugammadex in anesthetized guinea pigs, the administration of cisatracurium caused a more intense neuromuscular blockade with a faster than normal onset (48). Kopman et al. (49) also demonstrated that the ED50 of mivacurium was 56% less if calculated after full recovery from mivacuriuminduced neuromuscular blockade than after the initial blockade. When succinylcholine rather than cisatracurium was administered, complete blockade could also be induced; however, its onset was delayed in the guinea pig (48). Pretreatment with nondepolarizing neuromuscular blockers had a marked antagonistic effect on the development of the subsequent depolarizing blockade produced by succinylcholine (50). The interaction of sugammadex with other molecules has been tested with isothermal titration microcalorimetry. This technique measures the heat production when two molecules form a complex. The ability of sugammadex to form complexes with other steroidal and nonsteroidal compounds, such as cortisone, atropine, and verapamil, is probably clinically insignificant and is approximately 120–700 times less than that of rocuronium (51). Steroidal molecules form complexes with sugammadex, but with a much lower affinity, because the high affinity of sugammadex for rocuronium and vecuronium is caused by the interaction between the negatively charged carboxyethyl side chains of sugammadex and the positively charged quaternary nitrogen of rocuronium and vecuronium. As endogenous steroidal hormones and steroidal drugs lack the quaternary nitrogen of the steroidal blockers, they show a much lower affinity. Furthermore, steroidal hormones are also bound tightly to specific protein carriers; for example, the sex hormones are bound with very high affinity to globulin. The possible effects of the sugammadex-induced improved solubility of propofol, midazolam, and bupivacaine on the pharmacodynamics/pharmacokinetics of these compounds have not yet been studied.
- Figure 2. Radiograph crystal structure of a rocuronium molecule (A) and a sugammadex molecule (B). Reproduced from Ref. 38, with permissison from ©Lippincott Williams & Wilkins. Figure 3. Encapsulation of rocuronium molecule (blue) by a sugammadex molecule (green) at 1:1 ratio. Modified from Ref. 38, with permission from ©Lippincott Williams & Wilkins.
- La manoeuvre pression cricoïdienne (PC) a été décrite initialement par Monro en 1774 pour prévenir l’entrée d’air dans l’estomac au cours des manoeuvres de ventilation. Cette manoeuvre a été reprise en 1961 par Sellick pour prévenir le risque d’inhalation du contenu gastrique chez les patients considérés comme ayant un estomac plein lors de l’induction anesthésique [1]. Cette manoeuvre est maintenant recommandée dans toutes les procédures d’anesthésie pour estomac plein sans avoir à ce jour fait scientifiquement preuve de son efficacité sur le plan clinique. Dans l’étude initiale de Sellick, trois cas de régurgitation ont été rapportés après relâchement de la pression. Schwartz et al. décrivent en 1995 douze cas d’inhalation sur 238 intubations endotrachéales réalisées en réanimation : neuf cas d’inhalation sont survenus alors que la PC était appliquée [29]. De nombreux autres cas ont été rapportés mais toujours dans des séries non comparatives ou des études à trop faibles échantillons pour pouvoir conclure. Ces accidents d’inhalations pulmonaires peuvent survenir dans un tiers des cas au cours de l’induction mais aussi dans 30 % des cas au cours de l’entretien de l’anesthésie ou au réveil du patient. Ainsi, la PC ne protège finalement qu’au cours de l’induction anesthésique. Devant la rareté du phénomène, la manoeuvre de Sellick n’a pu montrer son efficacité dans la prévention de la régurgitation. Il serait en effet nécessaire de recruter plus de 50 000 patients pour retrouver un avantage statistiquement significatif entre un groupe avec PC versus un groupe sans PC. Il existe de ce fait autant d’études en faveur de l’utilisation de la pression cricoïdienne que d’études contre. Toutes ces études sont centrées sur la réalisation ou les effets secondaires de la PC, aucune sur son efficacité Il en ressort que si la manoeuvre de Sellick est utilisée, il faut en connaître parfaitement les règles de réalisation: Elle s’effectue en appliquant une pression sur le cartilage cricoïde avec le pouce et l’index. Cette pression entraîne un contact entre le cartilage cricoïde et le corps vertébral de C6 dans sa partie antérieure, obturant ainsi l’oesophage et diminuant le risque de régurgitation. Pour obtenir une efficacité maximale de cette manoeuvre, il est nécessaire que la tête soit en hyperextension, augmentant ainsi la convexité antérieure du rachis cervical afin que la pression soit effective sur le cartilage cricoïde et puisse être transmise de façon optimale pour obturer l’oesophage. Par ailleurs, c’est dans ces conditions que la pression a une intensité maximale : en effet, une force de 44 Newtons (environ 4,5 kg) est nécessaire pour obturer efficacement l’oesophage chez 50 % des adultes [4]. La manoeuvre de Sellick doit être réalisée pendant toute la période précédant l’intubation. Les contre-indications à la réalisation de la manoeuvre de Sellick sont l’existence de vomissements actifs, la présence d’un corps étranger et les lésions des voies aériennes, en particulier au niveau de la jonction cricotrachéale. Cette manoeuvre peut entraîner une disjonction cricotrachéale complète avec l’impossibilité de ventiler le patient. La suspicion de fracture instable du rachis cervical notamment au niveau C5-C6 doit inciter à la plus grande prudence. Dans ce cas, la manoeuvre pourra éventuellement être réalisée à deux mains, la deuxième main servant de contre-appui pour prévenir la mobilisation du rachis cervical. Mais, en aucun cas, une mesure prophylactique, quelle qu’en soit la nature, ne prévient l’inhalation bronchique ; c’est pourquoi l’intubation trachéale dans ce contexte doit être bien codifiée et reposer essentiellement sur deux techniques : l’intubation vigile et, surtout, l’induction en séquence rapide.
