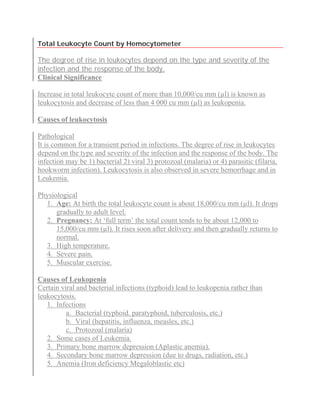
Total Leukocyte Count By Hemocytometer
- 1. Total Leukocyte Count by Hemocytometer The degree of rise in leukocytes depend on the type and severity of the infection and the response of the body. Clinical Significance Increase in total leukocyte count of more than 10,000/cu mm (µl) is known as leukocytosis and decrease of less than 4 000 cu mm (µl) as leukopenia. Causes of leukocytosis Pathological It is common for a transient period in infections. The degree of rise in leukocytes depend on the type and severity of the infection and the response of the body. The infection may be 1) bacterial 2) viral 3) protozoal (malaria) or 4) parasitic (filaria, hookworm infection). Leukocytosis is also observed in severe hemorrhage and in Leukemia. Physiological 1. Age: At birth the total leukocyte count is about 18,000/cu mm (µl). It drops gradually to adult level. 2. Pregnancy: At ‘full term’ the total count tends to be about 12,000 to 15,000/cu mm (µl). It rises soon after delivery and then gradually returns to normal. 3. High temperature. 4. Severe pain. 5. Muscular exercise. Causes of Leukopenia Certain viral and bacterial infections (typhoid) lead to leukopenia rather than leukocytosis. 1. Infections a. Bacterial (typhoid. paratyphoid, tuberculosis, etc.) b. Viral (hepatitis, influenza, measles, etc.) c. Protozoal (malaria) 2. Some cases of Leukemia. 3. Primary bone marrow depression (Aplastic anemia). 4. Secondary bone marrow depression (due to drugs, radiation, etc.) 5. Anemia (Iron deficiency Megaloblastic etc)
- 2. Normal values • Adults : 4,000-10,000/cu mm (µl) • At birth : 10,000-25,000/cu mm (µl) • 1 to 3 years : 6,000-18,000/cu mm (µl) • 4 to 7 years : 6,000-15,000/cu mm (µl) • 8 to 12 years: 4,500-13,500/cu mm (µl) Specimens 1. Double oxalated or EDTA blood 2. Capillary blood (specimen need not be a fasting sample). Requirements 1. Microscope 2. Improved Neubauer Chamber 3. WBC pipette 4. WBC diluting fluid: It is prepared as follows: a) Glacial acetic acid: 2.0 ml b) 1 % (w/v) gentian violet: 1.0 ml c) Distilled water: 97 ml This solution is stable at room temperature (25°C ± 5°C). A pinch of thymol may be added as preservative. Principle The glacial acetic acid lyses the red cells while the gentian violet slightly stains the nuclei of the leukocytes. The blood specimen is diluted 1:20 in a WBC pipette with the diluting fluid and the cells are counted under low power of the micro scope by using a counting chamber. The number of cells in undiluted blood are reported per cu mm (µl) of whole blood. Procedure 1. Draw blood up to 0.5 mark of a WBC pipette. 2. Carefully, wipe excess blood outside the pipette by using cotton. Draw diluting fluid up to 11 mark.
- 3. 3. Mix the contents in the pipette and after five minutes by discarding few drops, fill the counting chamber and allow the cells to settle for two to three minutes. — Since Bulb pipettes are not recommended following procedure is per formed — Make a 1:20 dilution of blood by adding 20 µl of blood to (1 38 ml of diluting fluid in a glass tube (10 * 75 mm) Cork the tube tightly and mix the suspension by rotating in a cell-suspension mixer for at least 1 minute. Fill the Neubauer counting chamber by means of a Pasteur pipette or glass capillary. 4. Focus on one of the ‘W’ marked areas (each having 16 small squares) by turning objective to low power. (10 X). 5. Count cells in all four W marked corner. 6. Calculations Number of white cells/cu mm (µl) of whole blood = (number of white cells counted * dilution) / (area counted * depth of fluid) Where: Dilution = 20 Area counted 4 * 1 sq.mm = 4 sq.mm Depth of fluid = 0.1 mm (constant) Hence number of white cells per cu mm (µl) of whole blood = (No. of cells counted * 20) / (4 * 0.1) = No of cells counted * 50 · No. of leukocyte per liter of blood = No.of cells per cu mm(ml) * 106 or use the following formula WBC count / liter = [No. of cells counted (per 1mm2 area) / volume counted (µl)] * dilution * 106 Note: The precautions taken are exactly the same as for REC counting technique. The sources of error are also same as for RBC counting technique. However; in the case of WBC counting extra care is taken during the preparation and storage of WBC diluting fluid. It should be perfectly free from dust particles and yeast cells, otherwise falsely high counts are obtained due to the presence of yeast cells and dust particles. Error of the total white cell count 1) The inherent distribution error = λ1/2, here λ = total number of cells in each area. 2) The error as high as 20% may make difference between 5.0 and 6.0 x 109 cells per liter, which is of little practical significance.
- 4. 3) The error can be reduced by counting more cells. If 400 cells are counted the error is reduced to 5%. 4) Error may also be caused due to dirt clumped RBC debris or due to clumping of leukocytes. Study of blood smear for differential leukocyte count and cell morphology Introduction Differential count is the percent distribution of various white cells in the peripheral blood. It is determined from a blood smear stained with a polychromatic stain and after examination of the stained smear by using oil immersion objective (total magnification 1000 X). The number of each type of white cell is then expressed as a percentage of the total number of cells. The stained blood smear also helps to study abnormal morphology of leukocytes and red cells. Study of blood smear helps in the diagnosis of various anemias, leukemias and detection of blood parasites. Three major steps involved in differential count are – a. preparation of blood smear b. staining of the blood smear and c. microscopic examination of the stained smear. The different types of leukocytes seen in a normal peripheral blood film may be divided into three broad groups — 1. Granulocytes 2. Monocytes and 3. Lymphocytes. 1) Granulocytes: There are three types of granulocytes which derive their names from the staining reaction of the granules present in the cytoplasm. These cells are a) Neutrophils or polymorphonuclears b) Eosinophils and c) Basophils. (a) Neutrophils (Polymorphonuclears): The average diameter is 10 to 12 µm. The nucleus is usually divided into 1-4 lobes. The cell derives its name from the color of the granules. The number of lobes give an indication of the age of the cell. (b) Eosinophils: The diameter is about the same as the neutrophil. The cytoplasm contains large, oval or round, red-orange (eosinophilic) granules. The nucleus shows fewer lobes, on an average only two. (c) Basophils or mast cells: The diameter is 8 to 10 µm. The nucleus is not easily seen due to the presence of large, round, deep blue or black granules.
- 5. 2) Monocyte: The diameter is about 16 to 22µm. The nucleus is kidney shaped or horse shoe shaped. Sometimes it may be round or oval. It stains pale violet and has fine chromatic arrangement. The cytoplasm is plentiful and stains pale greyish blue and contains a number of very fine pinkish-blue granules. 3) Lymphocyte: Two forms observed are — a) Large lymphocyte and b) Small lymphocyte. (a) Large lymphocytes: It is about 12 to 15µm in diameter. This has abundant clearpale blue cytoplasm and a large round or slightly in dented nucleus with dense chromatin. (b) Small lymphocyte: These are small round cells about 10 to 12µm in diameter. It has very little blue cytoplasm and often little more than just a rim around the nucleus. The nucleus is dark, round and sometimes indented. Differential leukocyte count technique Differential white cell counts are usually performed by visual examination of blood films which are pre pared on glass slides by “spread” technique. Following are the requirements for reliable results – 1. The film should not be very thin and the tail of the film should be smooth. To achieve this, the film should be made with a rapid movement using a smooth glass (slide) spreader. 2. In a good blood film, there is some overlap of the red cells, diminishing to separation near the tail. 3. If rough-edged spreader is used or if the film is too thin, many of the white cells (sometimes more than 50%), accumulate at the edges and in the tail. The distribution of white cells appears irregular. Polymorphonuclear neutrophils and monocytes predominate at the margins and the tail, and lymphocytes appear mainly at the middle of the film. The separation of cells depends upon differences in stickiness, size and specific gravity among the different classes of cells. 4. Some parasites (Borrelia, trypanosomes and microfilariae) can be detected in a fresh wet blood film by their motility, but for species identification a permanent preparation is necessary. A thick film is mainly employed for detecting parasites in the blood. Reporting the differential white cell count
- 6. 1) The differential count should be expressed as the percentage of each type of cell. It also should be related to the total leukocyte count and then the results should be reported in absolute numbers (x 109/l) 2) Nucleated red blood cells (NRBC) are reported as NRBC / 100 WBC. Since most of the auto mated blood cell counters include NRBC in WBC count, it is necessary to subtract total NRBC from total WBC count to get true value of total WBC count. 3) Band neutrophils (with two nucleated lobes) are counted separately. They normally constitute less than 6% of the neutrophils. An increase in band neutrophils may be observed in inflammatory process (in absence of an absolute leukocytosis).
