Malaria aicog 2013
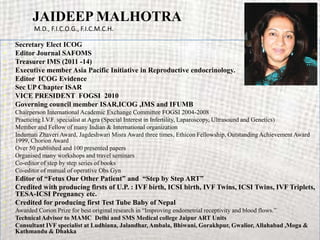
- 1. JAIDEEP MALHOTRA M.D., F.I.C.O.G., F.I.C.M.C.H. • Secretary Elect ICOG • Editor Journal SAFOMS • Treasurer IMS (2011 -14) • Executive member Asia Pacific Initiative in Reproductive endocrinology. • Editor ICOG Evidence • Sec UP Chapter ISAR • VICE PRESIDENT FOGSI 2010 • Governing council member ISAR,ICOG ,IMS and IFUMB • Chairperson International Academic Exchange Committee FOGSI 2004-2008 • Practicing I.V.F. specialist at Agra (Special Interest in Infertility, Laparoscopy, Ultrasound and Genetics) • Member and Fellow of many Indian & International organization • Indumati Zhaveri Award, Jagdeshwari Misra Award three times, Ethicon Fellowship, Outstanding Achievement Award 1999, Chorion Award • Over 50 published and 100 presented papers • Organised many workshops and travel seminars • Co-editor of step by step series of books • Co-editor of manual of operative Obs Gyn • Editor of “Fetus Our Other Patient” and “Step by Step ART” • Credited with producing firsts of U.P. : IVF birth, ICSI birth, IVF Twins, ICSI Twins, IVF Triplets, TESA-ICSI Pregnancy etc. • Credited for producing first Test Tube Baby of Nepal • Awarded Corion Prize for best original research in “Improving endometrial receptivity and blood flows.” • Technical Advisor to MAMC Delhi and SMS Medical college Jaipur ART Units • Consultant IVF specialist at Ludhiana, Jalandhar, Ambala, Bhiwani, Gorakhpur, Gwalior, Allahabad ,Moga & Kathmandu & Dhakka
- 2. Malaria and Pregnancy Dr Jaideep Malhotra Dr Narendra Malhotra
- 3. Malaria Menance • World wide 107 countries with 2.5 billion people, developing countries worst affected. • 40 % of world’s population in shadow of Malaria. • Of the 2.5 million reported cases in the South East Asia, India alone contributes about 70% of the total cases. • Deaths- Under estimated/Unknown,1.1 to 2.7 million per year • Gender related mortality - Females more • Malaria in Pregnancy: - – Mutually aggravating – Mortality is double – Primigravidae - 60-70% – Highest prevalence in second half. – Plasmodium Falciparum – More common.
- 4. Malaria Life Cycle Oocyst Sporozoites Mosquito Salivary Zygote Gland Gametocytes Liver stage Plasmodium falciparum Plasmodium vivax Red Blood Cell Cycle Plasmodium ovale Plasmodium malariae
- 5. Why are Malaria and Pregnancy mutually aggravating? • The physiological changes of pregnancy and the pathological changes due to malaria have a synergistic effect on the course of each other, thus making life difficult for the mother, the child and the treating physician. • P. falciparum malaria can run a turbulent and dramatic course in pregnant women. • The non- immune, primigravidae are usually the most affected. • In areas where malaria is endemic, 20-40% of all babies born may have a low birth weight.
- 6. Malaria in Pregnancy : • More common. – Malaria is more common in pregnancy compared to the general population probably due to Immuno suppression and loss of acquired immunity to malaria. • More atypical. – In pregnancy, malaria tends to be more atypical in presentation probably due to the hormonal , immunological and haematological changes of pregnancy. • More severe. – Probably for the same reason, the parasitemia tends to be 10 times higher and as a result, all the complications of falciparum malaria are more common in pregnancy compared to the non-pregnant population.
- 7. Malaria in Pregnancy : • More fatal – P. falciparum malaria in pregnancy being more severe, the mortality is also double (13 % ) compared to the non-pregnant population (6.5%). • Selective treatment – Some anti malarials are contra indicated in pregnancy and some may cause severe adverse effects. – Therefore the treatment may become difficult, particularly in cases of severe P. falciparum malaria. • Other problems – Management of complications of malaria may be difficult due to the various physiological changes of pregnancy. – Careful attention has to be paid towards fluid management, temperature control, etc. – Decisions regarding induction of labour may be difficult and complex. – Foetal loss, IUGR, and premature labour are common.
- 8. Turbulent Course in pregnancy • Particularly the first and second pregnancies. • These complications are more common and severe in hyperendemic areas for falciparum malaria. • Physiologic changes of pregnancy contribute to the aggravation of malarial infection. – Changes in the hormonal milieu, – Increase in the body fluid volume, – Decrease in haemoglobin level and other changes add to the severity.
- 9. Pathology of Malaria in Pregnancy • There is a generalised immunosuppression in pregnancy with reduction in gamma globulin synthesis and inhibition of reticulo endothelial system, resulting in – Decrease in the levels of anti malarial antibodies and loss of acquired immunity to malaria. – This makes the pregnant woman more prone for malarial infection and the parasitemia tends to be much higher.
- 10. Changes in Placenta • Placenta is the preferred site of sequestration and development of malarial parasite. • Intervillous spaces are filled with parasites and macrophages, interfering with oxygen and nutrient transport to the foetus. • Villous hypertrophy and fibrinoid necrosis of villi (complete or partial) have been observed. • All the placental tissues exhibit malarial pigments (with or even without parasites).
- 11. Placental Parasitemia by Pregnancy Number Parasite density/mm3 30 1-999 1000-9,999 >10,000 25 % parasitemic 20 15 10 5 772 402 479 0 First Pregnancies Second Pregnancies Three or more pregnancies Source: van Eijk AM et al 2001. Malaria During Pregnancy 11
- 12. Clinical features Atypical manifestations of malaria are more common in pregnancy, particularly in the 2nd half of pregnancy. • Fever : – Patient may have different patterns of fever - from afebrile to continuous fever, low grade to hyper pyrexia. – In 2nd half of pregnancy, there may be more frequent paroxysms due to Immunosuppression. • Anemia : – In developing countries, where malaria is most common, anemia is a common feature of pregnancy. – Malnutrition and helminthiasis are the commonest causes of anemia. – In such a situation, malaria will compound the problem. – Anemia may even be the presenting feature of malaria and therefore all cases of anemia should be tested for M.P. – Anemia as a presenting feature is more common in partially immune multigravidae living in hyper endemic areas.
- 13. Clinical features Atypical manifestations of malaria are more common in pregnancy, particularly in the 2nd half of pregnancy. • Splenomegaly : – Enlargement of the spleen may be variable. It may be absent or small in 2nd half of pregnancy. – A pre-existing enlarged spleen may regress in size in pregnancy. • Complications : – Complications tend to be more common and more severe in pregnancy. – A patient may present with complications of malaria or they may develop suddenly. – Acute pulmonary edema, – hypoglycemia – anemia are more common in pregnancy. – Jaundice, convulsions, altered sensorium, coma, vomiting / diarrhoea and other complications may be seen.
- 14. Effects on the Pregnant Woman Primigravidae in All parities in Effects Stable malaria Unstable malaria areas areas High fever + +++ Placental infection +++ + Puerperal sepsis ++ ++ Complicated malaria Severe anemia +++ +++ Cerebral malaria - ++ Hypoglycemia - ++ Pulmonary edema - ++ Acute renal failure - ++ Increased maternal mortality + ++ ( +++ =Very Common, ++ =Common, + =Infrequent, -- =Rare)
- 15. Complications of Malaria in Pregnancy Anemia • Malaria can cause or aggravate anaemia due to: – Hemolysis of parasitised red blood cells. – Increased demands of pregnancy. – Profound hemolysis can aggravate folate deficiency. • Anemia due to malaria is more common and severe between 16-29 weeks. • It can develop suddenly, in case of severe malaria with high grades of parasitemia. • Pre existing iron and folate deficiency can exacerbate the anemia of malaria and vice versa.
- 16. Complications of Malaria in Pregnancy Acute pulmonary oedema • Acute pulmonary oedema is also a more common complication of malaria in pregnancy compared to the non-pregnant population. • It may be the presenting feature or can develop suddenly after several days. It is more common in 2nd and 3rd trimesters. • It can develop suddenly in immediate post-partum period. This is due to – Auto transfusion of placental blood with high proportion of parasitised RBC’s – Sudden increase in peripheral vascular resistance after delivery. • It is aggravated by pre existing anaemia and hemodynamic changes of pregnancy. • Acute pulmonary oedema carries a very high mortality.
- 17. Complications of Malaria in Pregnancy Hypoglycaemia • This is another complication of malaria that is peculiarly more common in pregnancy. • The following factors contribute to hypoglycemia: – Increased demands of hypercatabolic state and infecting parasites. – Hypoglycaemic response to starvation. – Increased response of pancreatic islets to secretory stimuli (like quinine) leads to hyperinsulinemia and hypoglycemia..
- 18. Complications of Malaria in Pregnancy Hypoglycaemia • Hypoglycaemia in these patients can remain asymptomatic and may not be detected, because: – all the symptoms of hypoglycemia are also caused by malaria viz. tachycardia, sweating, giddiness etc. – Some patients may have abnormal behaviour, convulsions, altered sensorium, sudden loss of consciousness etc. – These symptoms of hypoglycemia may be easily confused with cerebral malaria. – Therefore, in all pregnant women with falciparum malaria, particularly those receiving quinine, blood sugar should be monitored every 4-6 hours.
- 19. Complications of Malaria in Pregnancy Hypoglycaemia: • Hypoglycaemia can be recurrent and therefore constant monitoring is needed. • In some, it can be associated with lactic acidosis and in such cases mortality is very high. • Maternal hypoglycemia can cause foetal distress without any signs.
- 20. Complications of Malaria in Pregnancy Immunosuppression • Immunosuppression in pregnancy poses special problems. • It makes malaria more common and more severe. And to add to the woes, malaria itself suppresses immune response. • Hormonal changes of pregnancy, reduced synthesis of immunoglobulins, reduced function of reticulo endothelial system are the causes for Immunosuppression in pregnancy.
- 21. Complications of Malaria in Pregnancy Immunosuppression • This results in loss of acquired immunity to malaria, making the pregnant more prone for malaria. • Malaria becomes more severe with higher parasitemia. • Patient may have more frequent paroxysms of fever and frequent relapses. • Secondary infections (U.T.I. and pneumonias) and algid malaria (septicaemic shock) are more common in pregnancy due to Immunosuppression.
- 22. Cerebral malaria Quite common Diagnosis can be difficult Coma scoring Exclude other causes of coma Needs Intensive care 1. ABC of coma care 2. Prompt institution of antimalarials 3. Treatment of hyperpyrexia 4. Management of other complications 5. Treatment of associated infections
- 23. Effects on the Fetus and Newborn Primigravidae in All parities in Effects Stable malaria Unstable malaria areas areas Low birth weight IUGR +++ + Prematurity + ++ Abortion - ++ Stillbirth - ++ Congenital malaria - + Fetal anemia ? + Infant mortality + ++ ( +++=Very Common, ++=Common, +=Infrequent, -- =Rare)
- 24. Risks for the foetus • Malaria in pregnancy is detrimental to the foetus due to: - – high grades of fever, – placental insufficiency, – hypoglycaemia, – anaemia and other complications. • Both P. vivax and P. falciparum malaria can pose problems for the foetus, with the latter being more serious.
- 25. Risks for the foetus • The prenatal and neonatal mortality may vary from 15 to 70%. – neonatal mortality due to P. vivax malaria during pregnancy was 15.7% while that due to P. falciparum was 33%. – Spontaneous abortion, – pre mature birth, – still birth, – placental insufficiency – I.U.G.R. (temporary / chronic), – low birth weight, – foetal distress are the different problems observed in the growing foetus. – Transplacental spread of the infection to the foetus can result in congenital malaria.
- 26. Frequency of Low Birth Weight by Placental Malaria Infection 35 30 % Low Birth Weight 25 20 With placental 15 parasites 10 Without placental parasites 5 0 First Second Three or more Pregnancy Pregnancy pregnancies Source: Steketee 2001.
- 27. Risks for the foetus Congenital malaria • It is very rare and occurs in < 5% of affected pregnancies. Placental barrier and maternal Ig G antibodies which cross the placenta may protect the foetus to some extent. • However, it is much more common in non-immune population and the incidence goes up during epidemics of malaria. • Fetal plasma Quinine and Chloroquine levels are about one third of simultaneous maternal levels and this subtherapeutic drug level does not cure the infection in the foetus.
- 28. Risks for the foetus Congenital malaria • All four species can cause congenital malaria, but it is proportionately more with P. malariae. • The new born child can manifest with fever, irritability, feeding problems, hepato splenomegaly, anaemia, jaundice etc. • The diagnosis can be confirmed by a smear for M.P. from cord blood or heel prick, anytime within a week after birth (or even later if post-partum, mosquito- borne infection is not likely). • Differential diagnoses include Rh. incompatibility, infections with C.M.V., Herpes, Rubella, Toxoplasmosis, and syphilis.
- 29. Diagnosis • High level of awareness • Peripheral blood smear (Gold standard) thick smear: rapid diagnosis thin : species identification • other advantages - platelets, anaemia, toxic picture If negative : repeat blood test 6 hourly for 6 times • Antigen detection techniques : (PfHPR-2) • Fluorescent staining • PCR based assay • Antibody test • Placental blood smear
- 30. Why parasites are not detected at times in peripheral smear ? a. sequestration deep vascular bed b. partially treated patients c. prophylactic antimalarial Tt d. inexperienced microscopist e. poor quality staining
- 31. Antigen capture tests * Pf-ICT test * Parasight-F test/ Malacheck etc Principle: dipstick antigen capture assay employs a monoclonal antibody detecting the Pf.HRP-2 antigen in the blood Rapid, simple, sensitive test Species specificity Antibody detection test - RIA - ELISA antibodies persists for a long time, so not helpful in acute infection
- 32. PCR test Sensitive can identify different species Takes 48- 72 hours Expensive Available in selected places only DNA Probes QBC test Spinning blood in a specialised capillary tubes in which parasite DNA is stained with acridine orange. Detected by ultraviolet microscope Sensitive and specific (?) in Experienced hands
- 33. Indicators of Poor Prognosis • Hyper parasitemia: - 5% erythrocytes infested. • Peripheral schizotaemia. • Leucocytosis 12,000/ cmm. • Hb 7.1 gm%. • PCV 20 %. • Blood urea 60 mg / dL • Creatinine 3 mg / dL., • Blood glucose 40 mg / dL. • High lactate and low sugar in CSF. • Low antithrombin III level.
- 34. Management of Malaria in Pregnancy • Management of malaria in pregnancy involves the following three aspects and equal importance should be attached to all the three. 1. Treatment of malaria 2. Management of complications 3. Management of labour
- 35. Treatment of Malaria in Pregnancy Should Be Energetic, Anticipatory and Careful. Energetic: • Don't waste any time. • It is better to admit all cases of P. falciparum malaria. • Assess severity- – General condition, pallor, jaundice, B.P., temperature, haemoglobin, Parasite count, S.G.P.T., S .bilirubin, S.creatinine, Blood sugar.
- 36. Treatment of Malaria in Pregnancy Should Be Energetic, Anticipatory and Careful. Anticipatory: • Malaria in pregnancy can cause sudden and dramatic complications. Therefore, one should always be looking for any complications by regular monitoring. • Monitor maternal and foetal vital parameters 2 hourly. • R.B.S. 4-6 hourly; haemoglobin and parasite count 12 hourly; S. creatinine; S. bilirubin and Intake / Output chart daily.
- 37. Treatment of Malaria in Pregnancy Should Be Energetic, Anticipatory and Careful. Careful: • The physiologic changes of pregnancy pose special problems in management of malaria. • In addition, certain drugs are contra indicated in pregnancy or may cause more severe adverse effects. All these factors should be taken into consideration while treating these patients. • Choose drugs according to severity of the disease/ sensitivity pattern in the locality. • Avoid drugs that are contra indicated • Avoid over / under dosing of drugs • Avoid fluid overload / dehydration • Maintain adequate intake of calories.
- 38. Treatment of Malaria in Pregnancy Choice of Anti malarials in pregnancy • All trimesters: – First line - Chloroquine; Quinine; – Second line - Artesunate / Artemether / Arteether • 2nd / 3rd trimester: with caution – Pyrimethamine + sulphadoxine; Mefloquine • Contra indicated: – Primaquine; Tetracycline; Doxycycline; Halofantrine
- 39. Treatment of Malaria in Pregnancy Dose of Anti malarials • Chloroquine: – 600mg (base) start, 300mg after 6 hours, 24 hours & 48 hours • Quinine: – IV - 20mg/kg infusion over 4 hours, repeat 8 hourly. – Maintenance: 10mg over 4 hours, 8 hourly. Follow with oral medication after clinically stable. • Oral – 600mg 8hourly ( maximum 2 gm / day) for 7 days. • Presently fixed dose combinations of • Artesunate + amodiaquine • Blister pack of artesunate +mefloquine
- 40. Treatment of Malaria in Pregnancy Dose of Anti malarials Artemisinin compounds(rapid Schizonticidal) • Artesunate(Falcigo): – Oral-100mg BD on day 1, then 50mg BD for 4-6 days (Total dose 10mg/kg). – IM / IV-120mg on Day 1 followed by 60mg daily for 4 days. In severe cases an additional dose of 60mg after 6 hours on Day 1. • Artemether(Larither): – Six amp (480mg) IM in 5 / 3 days. 1x2x1+1x1x4 OR 1x2x3. – 80mg BD X3 days • Arteether(Emal inj): – One amp (150mg) IM / day for3 consecutive days.
- 41. Dose of Antimalarials • Pyrimethamine 25mg+sulphadoxine 500mg tablets: – Three tablets single dose. • Mefloquine: – 15mg / kg body wt., up to 1 Gm in a single dose. OR • Tablets of 250mg, 3 tab start, then 2 tab after 6-8 hours. With body wt >60kg, a third dose of 1 tab after 6-8 hours.
- 42. NIMR guidelines 2010 • ACT should be given for treatment of P. falciparum malaria in: • second and third trimesters of pregnancy, • while quinine is recommended in the first trimester. • P. vivax malaria can be treated with chloroquine • ACT containing mefloquine should be avoided in cerebral malaria due to neuropsychiatric complications.
- 43. General recommendations for the management of uncomplicated malaria • Avoid starting treatment on an empty stomach. • The first dose should be given under observation. • Dose should be repeated if vomiting occurs within 30 minutes. • The patient should be asked to report back, if there is no improvement after 48 hours or if the situation deteriorates. • The patient should also be examined for concomitant illnesses.
- 44. SEVERE MALARIA • Impaired consciousness/coma • Repeated generalized convulsions • Renal failure (Serum Creatinine >3 mg/dl) • Jaundice (Serum Bilirubin >3 mg/dl) • Severe anaemia (Hb <5 g/dl) • Pulmonary oedema/acute respiratory distress syndrome • Hypoglycaemia (Plasma Glucose <40 mg/dl) • Metabolic acidosis • Circulatory collapse/shock (Systolic BP <80 mm Hg, <50 mmHg in children) • Abnormal bleeding and Disseminated intravascular coagulation(DIC) • Haemoglobinuria • Hyperpyrexia (Temperature >106o F or >42o C) • Hyperparasitaemia (>5% parasitized RBCs )
- 45. Management of complications • Acute Pulmonary Oedema: – Careful fluid management; back rest; oxygen; diuretics; ventilation if needed. • Hypoglycaemia: – 25-50% Dextrose, 50-100 ml I.V., followed by 10% dextrose continuous infusion. – If fluid overload is a problem, then Inj. Glucagon 0.5-1 mg can be given intra muscularly. – Blood sugar should be monitored every 4-6 hours for recurrent hypoglycemia. • Anemia: – Packed cells should be transfused if haemoglobin is <5 g%. • Renal failure: – Renal failure could be pre-renal due to unrecognised dehydration or renal due to severe parasitemia. – Treatment involves careful fluid management, diuretics, and dialysis if needed.
- 46. Management of complications • Septicaemic shock: – Secondary bacterial infections like urinary tract infection, pneumonia etc. are more common in pregnancy associated with malaria. – Some of these patients may develop septicaemic shock, the so called 'algid malaria'. – Treatment involves administration of 3rd generation cephalosporins, fluid replacement, monitoring of vital parameters and intake and output. • Exchange transfusion: – Exchange transfusion is indicated in cases of severe falciparum malaria to reduce the parasite load. – It is especially useful in cases of very high parasitemia (helps in clearing) and impending pulmonary oedema (helps to reduce fluid load).
- 47. Management of Labour • Anaemia, hypoglycaemia, pulmonary oedema, and secondary infections due to malaria in pregnancy lead to problems for both the mother and the foetus. • Severe falciparum malaria in term pregnancy carries a very high mortality. • Maternal and foetal distress may go unrecognised in these patients. • Therefore, careful monitoring of maternal and foetal parameters is extremely important. • Pregnant women with severe malaria are better managed in an intensive care unit.
- 48. Management of Labour • Falciparum malaria induces uterine contractions, resulting in premature labour. The frequency and intensity of contractions appear to be related to the height of the fever. • Fetal distress is common and often unrecognised. Therefore only monitoring of uterine contractions and fetal heart rate may reveal asymptomatic labour and foetal distress. • All efforts should be made to rapidly bring the temperature under control, – By tepid sponging (cold sponging causes cutaneous vasoconstriction and can result in core hyperpyrexia). – Anti pyretics like paracetamol etc.
- 49. Management of Labour • Careful fluid management is also very important. Dehydration as well as fluid overload should be avoided, because both could be detrimental to the mother and/or the foetus. • In cases of very high parasitemia, exchange transfusion may have to be carried out. • If the situation demands, induction of labour may have to be considered. • Once the patient is in labour, foetal or matenal distress may indicate the need to shorten the 2nd stage by forceps or vacuum extraction. • If needed, even caesarean section must be considered.
- 50. Treatment of Vivax Malaria in Pregnancy Radical cure • Use of Primaquine & Proguanil are not safe in pregnancy and also in lactating mothers. • Therefore to prevent the relapse of vivax malaria, suppressive chemoprophylaxis with Chloroquine is recommended. • Tablet Chloroquine 300 mg (base) weekly should be administered to all such patients until stoppage of lactation. • At that point, a complete treatment with full therapeutic dose of Chloroquine and Primaquine (7.5mg b.I.d. or 15mg daily, for 14 days) should be administered. • However in case of resistance, Primaquine or Proguanil may be given with caution in 2nd half of pregnancy.
- 51. TREATMENT OF MIXED PLASMODIUM INFECTIONS • In patients with confirmed or suspected mixed infections i.e. P. falciparum with either P. vivax or P. ovale, the standard therapy for uncomplicated or severe P. falciparum malaria (either quinine or artemether-lumefantrine) plus a follow-up course of primaquine is recommended. • A mixed infection of P. falciparum and P. malariae should be managed as for P. falciparum malaria. The severity of the P. falciparum infection should dictate choice of initial therapy. Doubt frequently exists about the presence of P. falciparum in addition to other Plasmodium species. • The patient should then be treated for P. falciparum, as this is the species most frequently associated with severe infections and complications.
- 52. COMMON ERRORS IN MANAGEMENT OF SEVERE MALARIA 1. Failure to diagnose associated complications such as bacterial infections, eclampsia, Gram negative septicemia etc 2. Missed hypoglycaemia 3. Misjudgement of severity 4. Errors of fluid and electrolytic replacement 5. Errors in anti-malarial chemotherapy 6. Delay in starting treatment Unjustified withholding of antimalarial drug for the fear of toxicity e.g. Quinine in pregnant women, in hypoglycaemia -Inadequate dosage administration -Failure to control the rate of IV infusion 7. Delay in considering obstetrics intervention pregnant women suffering from malaria 8. Missed / late diagnosis of ARDS, acute pulmonary oedema 9. Use of inappropriate ancillary therapies e.g. steroids 10. Delay in starting dialysis
- 53. Components of Malaria Control During Pregnancy 1.Quality focused antenatal care and health education 2.Intermittent preventive treatment (IPT) 3.Use of insecticide-treated nets (ITNs) 4.Case management of malaria disease
- 54. Health Education on Malaria During Pregnancy: What To Tell Patients • Pregnant women (especially primigravida, secundigravida and HIV-infected women) are at higher risk of malaria • Malaria: – Is transmitted through mosquito bites – Can cause severe anemia, with adverse consequences for mother and baby – Can cause abortions, stillbirths and result in low birth weight newborns – Can be prevented through the use of IPT and ITNs during pregnancy – Can be easily treated if recognized early but complicated malaria requires specialized treatment
- 56. Use of Insecticide-Treated Nets (ITNs) ITNs: • Have been shown to result in reduction of newborns born with low birth weight or prematurely • Reduce transmission by physically preventing vector mosquitoes from landing on sleeping persons • Repel and kill mosquitoes that come in contact with the net • Kill other insects like cockroaches, lice, ticks and bed bugs • Should be used by pregnant women as early during pregnancy as possible and use should be encouraged throughout pregnancy and in the postpartum period
- 57. Impact of ITNs on Maternal and Newborn Health Among Gravidae 1-4, ITNs were associated with: • During pregnancy – 38% reduction in peripheral parasitemia – 21% reduction in all causes of anemia (Hb < 11 g/dl) – 47% reduction in severe malarial anemia • At delivery – 23% reduction in placental malaria – 28% reduction in LBW – 25% reduction in any adverse birth outcome • No trend towards decreasing efficacy with increasing transmission rate Source: Shulman 2001. 58
- 58. Intermittent Preventive Treatment (IPT) • An approach for effectively preventing and controlling malaria during pregnancy • Based on an assumption that every pregnant woman in a malaria-endemic area is infected with malaria • Recommends that every pregnant women receive at least two treatment doses of an effective antimalarial drug • Sulfadoxine-pyrimethamine (SP) currently considered the most effective drug for IPT
- 59. Chemoprophylaxis in Pregnancy • Malaria being potentially fatal to both the mother and the foetus, this should be an important part of antenatal care in areas of high transmission. – All pregnant women, who remain in the malarious area during their pregnancy, should be protected with chemoprophylaxis. • Choice of anti malarials for chemo prophylaxis: – Chloroquine being the safest drug in pregnancy, should be the first choice. – However, its use may be restricted due to the wide spread resistance to this drug. – In areas with known resistance to Chloroquine • Pyrimethamine + Sulpha, Mefloquine or Proguanil can be used. • But these drugs should be started only after 1st trimester only.
- 60. Fetal Growth Velocity Fetal growth velocity Last month 10 16 20 30 Conception Weeks of gestation Birth Source: WHO 2002. 61 Malaria During Pregnancy
- 61. Fetal Growth Velocity Fetal growth velocity Quickening Last month 10 16 20 30 Conception Weeks of gestation Birth Source: WHO 2002. 62 Malaria During Pregnancy
- 62. Rationale for the Timing of the Doses Fetal growth velocity Rx Rx Quickening Last month 10 16 20 30 Conception Weeks of gestation Birth Source: WHO 2002. 63 Malaria During Pregnancy
- 63. Key Issues About Timing of Doses • SP should be avoided during the first 16 weeks of pregnancy which is the period of initial development of the fetus • It is best to clear the placenta of parasites during the period of maximum fetal growth • IPT allows the mother to recover from anemia by clearing peripheral parasitaemia 64
- 64. Chemoprophylaxis in Pregnancy DOSAGE • Chloroquine: - 300mg base, administered once every week. • Pyrimethamine-25mg + Sulphadoxine-500mg: - One tablet once weekly. • Mefloquine: -250mg weekly. – Dose may have to be increased in the last trimester, in view of the accelerated clearance of the drug. • Proguanil: - 150-200mg / day.
- 65. Effect of Intermittent Preventive Treatment with SP Case Two-dose Monthly management SP SP p N=472 N=432 N=431 Mean Hb. 9.9 10.2 10.4 < 0.05 Maternal 27% 9% 7% 0.004 parasitemia Placental 27% 12% 9% < 0.001 parasitemia LBW 14% 8% 8% 0.01 Source: Steketee 2001.
- 66. Case Management: Drug Efficacy • Effective drugs are needed for P. falciparum malaria as it can be fatal to both mother and child • Drug of choice depends on the geographic drug resistance profile: – Chloroquine is the drug of choice in few areas where it is still effective – SP often next choice – Quinine is the drug of choice for complicated malaria
- 67. Resistance to Drugs • Resistance of P. falciparum to antimalarial drugs is an ever increasing problem • To minimize the problem of drug resistance, encourage women to complete their course of antimalarial drugs, even when they feel better • Drug resistance is inevitable; • WHO recommends these combinations,incase of drug resistance. • Artemether–lumefantrine, • Artesunate– amodiaquine, • Artesunate–mefloquine, • Artesunate–sulfadoxine–pyrimethamine, area dependent • Dihydroartemisinin–piperaquine.
- 68. Drugs That Should Not Be Used During Pregnancy • Tetracycline – Cause abnormalities of skeletal and muscular growth, tooth development, lens/cornea • Doxycycline – Risk of cosmetic staining of primary teeth is undetermined – Excreted into breast milk • Primaquine – Harmful to newborns who are relatively Glucose-6- Phosphatase-Dehydrogenase (G6PD) deficient • Halofantrine – No conclusive studies in pregnant women – Has been shown to cause unwanted effects, including death of the fetus, in animals
- 69. Conclusions • Widely prevalent 36% population exposed • Preventing mosquito bite • Chemoprophylaxis • Drug resistance is a problem. • Energetic anticipatory management • Maternal and neonatal morbidity and mortality high.
