December 2012 NLE Tips Funda
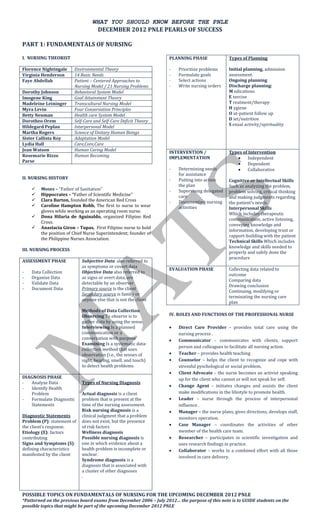
- 1. WHAT YOU SHOULD KNOW BEFORE THE PNLE DECEMBER 2012 PNLE PEARLS OF SUCCESS PART 1: FUNDAMENTALS OF NURSING I. NURSING THEORIST PLANNING PHASE Types of Planning Florence Nightingale Environmental Theory - Prioritize problems Initial planning, admission Virginia Henderson 14 Basic Needs - Formulate goals assessment. Faye Abdellah Patient – Centered Approaches to - Select actions Ongoing planning Nursing Model / 21 Nursing Problems - Write nursing orders Discharge planning: Dorothy Johnson Behavioral System Model M edications Imogene King Goal Attainment Theory E xercise Madeleine Leininger Transcultural Nursing Model T reatment/therapy Myra Levin Four Conservation Principles H ygiene Betty Neuman Health care System Model O ut-patient follow up Dorotheo Orem Self-Care and Self-Care Deficit Theory D iet/nutrition Hildegard Peplau Interpersonal Model S exual activity/spirituality Martha Rogers Science of Unitary Human Beings Sister Callista Roy Adaptation Model Lydia Hall Care,Core,Cure Jean Watson Human Caring Model INTERVENTION / Types of Intervention Rosemarie Rizzo Human Becoming IMPLEMENTATION Independent Parse Dependent - Determining needs Collaborative for assistance II. NURSING HISTORY Putting into action - Cognitive or Intellectual Skills the plan Such as analyzing the problem, Moses – “Father of Sanitation” Supervising delegated - problem solving, critical thinking Hippocrates – “Father of Scientific Medicine” care and making judgments regarding Clara Barton, founded the American Red Cross Documenting nursing - the patient's needs. Caroline Hampton Robb, The first to nurse to wear activities Interpersonal Skills gloves while working as an operating room nurse. Which includes therapeutic Dona Hilaria de Aguinaldo, organized Filipino Red communication, active listening, Cross. conveying knowledge and Anastacia Giron – Tupas, First Filipino nurse to hold information, developing trust or the position of Chief Nurse Superintendent; founder of rapport-building with the patient the Philippine Nurses Association. Technical Skills Which includes knowledge and skills needed to III. NURSING PROCESS properly and safely done the procedure ASSESSMENT PHASE Subjective Data also referred to as symptoms or covert data EVALUATION PHASE Collecting data related to - Data Collection Objective Data also referred to outcome - Organize Data as signs or overt data, are Comparing data - Validate Data detectable by an observer Drawing conclusion - Document Data Primary source is the client Continuing, modifying or Secondary source is family or terminating the nursing care anyone else that is not the client plan Methods of Data Collection Observing To observe is to IV. ROLES AND FUNCTIONS OF THE PROFESSIONAL NURSE gather data by using the sense. Interviewing Is a planned Direct Care Provider - provides total care using the communication or a nursing process . conversation with purpose Communicator – communicates with clients, support Examining Is a systematic data- person and colleagues to facilitate all nursing action. collection method that uses observation (i.e., the senses of Teacher – provides health teaching sight, hearing, smell, and touch) Counselor – helps the client to recognize and cope with to detect health problems. stressful pyschological or social problem, Client Advocate – the nurse becomes an activist speaking DIAGNOSIS PHASE up for the client who cannot or will not speak for self. - Analyze Data Types of Nursing Diagnosis Change Agent – initiates changes and assists the client - Identify Health Problem Actual diagnosis is a client make modifications in the lifestyle to promote health. - Formulate Diagnostic problem that is present at the Leader – nurse through the process of interpersonal Statements time of the nursing assessment. influence . Risk nursing diagnosis is a Manager – the nurse plans, gives directions, develops staff, Diagnostic Statements clinical judgment that a problem monitors operation. Problem (P): statement of does not exist, but the presence the client’s response. of risk factors Case Manager – coordinates the activities of other Etiology (E): factors Wellness diagnosis member of the health care team. contributing Possible nursing diagnosis is Researcher – participates in scientific investigation and Signs and Symptoms (S): one in which evidence about a uses research findings in practice. defining characteristics health problem is incomplete or Collaborator – works in a combined effort with all those manifested by the client unclear. involved in care delivery. Syndrome diagnosis is a diagnosis that is associated with a cluster of other diagnoses . POSSIBLE TOPICS ON FUNDAMENTALS OF NURSING FOR THE UPCOMING DECEMBER 2012 PNLE *Patterned on the previous board exams from December 2006 – July 2012… the purpose of this note is to GUIDE students on the possible topics that might be part of the upcoming December 2012 PNLE
- 2. WHAT YOU SHOULD KNOW BEFORE THE PNLE DECEMBER 2012 PNLE PEARLS OF SUCCESS PART 1: FUNDAMENTALS OF NURSING V. HEALTH / DISEASE / ILLNESS C. Airborne Transmission Health is the complete physical, mental, social (totality) 1. Droplet of nuclei well-being and not merely the absence of disease or 2. Dust particle in the air containing the infectious infirmity. agent 3. Organisms shed into environment from skin, hair, FOUR MODELS OF HEALTH BY SMITH wounds or perineal area. 1. Clinical Model Man is viewed as a Physiologic Being D. Vector borne Transmission, arthropods such as If there are no signs and symptoms of a disease, then flies, mosquitoes, ticks and others. you are healthy 2. Role Performance Model As long as you are able to perform SOCIETAL VII. ISOLATION PRECAUTIONS functions and ROLES you are healthy 3. Adaptive Model Standard Precautions / Universal Precautions Health is viewed in terms of capacity to ADAPT Applies to ALL BODY FLUIDS Failure to adapt is disease Includes: 4. Eudaemonistic Model 1. HAND WASHING Because health is viewed in terms of Actualization 2. Personal Protective Equipment (sequence of removing PPE’s) Disease is a pathologic change in the structure or function gloves-mask-gown-eyewear-cap of the mind and body 3. Safe use of sharps Illness is a highly subjective feeling of being sick or ill 4. Removing spills of blood and body fluids 5. Cleaning and disinfecting equipment STAGES OF ILLNESS AND HEALTH-SEEKING BEHAVIOR BY Transmission Based Precautions SUCHMAN • Airborne precautions Symptom Experience A single room under negative pressure Client realizes there is a problem ventilation with a wash hand basin Client responds emotionally The door must be kept closed at all times except Sick Role Assumption during necessary entrances and exits. Self-medication / Self-treatment Disposable paper towels Communication to others A high efficiency mask, if available, should be Assuming a Dependent Role worn when entering the room of a patient with Accepts the diagnosis known or suspected tuberculosis. Follows prescribed treatment Achieving recovery and rehabilitation • Droplet precautions Gives up the dependent role and assumes Put on a standard mask prior to entering the normal activities and responsibilities isolation room. Hands must be washed with an antiseptic preparation and must be dried thoroughly with VI. CHAIN OF INFECTION a disposable paper towel or washed with a waterless alcohol hand rub/gel: 1. AFTER contact with the patient or potentially contaminated items, 2. AFTER removing gloves, and 3. BEFORE taking care of another patient. • Contact precautions Non-sterile, disposable gloves are needed when there is contact with an infected site, with dressings, or with secretions. A mask when performing procedures that may generate aerosols or when performing suctioning is recommended. Hands washing (see droplet precautions) VIII. NUTRITION Food Sources ► MODE OF TRANSMISSION it indicates the potential of the disease; conveyance of the agent to the host; it can be by Protein Meat, fish, eggs, milk, poultry, cheese, common source transmission, contact source, air-borne beans, mongo transmission. Carbohydrates Grains, Legumes, Potatoes, Cereals, Breads There are four main routes of transmission Fats / Lipids Saturated: coconut oil, and palm kernel A. By Contact Transmission oil, dairy products (especially butter, , 1. Direct contact ( person to person ) cream, and cheese), meat (beef), dark 2. Indirect contact ( usually an inanimate object) meat of poultry, and poultry skin, 3. Droplet contact ( from coughing, sneezing, or chocolate talking, or talking by an infected person) Unsaturated: Avocado, Nuts, Vegetable B. By Vehicle Route ( through contaminated items) oils such as soybean, canola, and olive oils 1. Food – salmonellosis Vit. A Eggs, carrots, squash, all green leafy 2. Water – shigellosis, legionellosis vegetables 3. Drugs – bacteremia resulting from infusion of a Vit. D Fish, liver, egg, milk, margarine contaminated infusion product Note: excess vit.D may lead to fetal cardiac 4. Blood – hepatitis B, problem Vit. E Green leafy vegetables, fish, corn POSSIBLE TOPICS ON FUNDAMENTALS OF NURSING FOR THE UPCOMING DECEMBER 2012 PNLE *Patterned on the previous board exams from December 2006 – July 2012… the purpose of this note is to GUIDE students on the possible topics that might be part of the upcoming December 2012 PNLE
- 3. WHAT YOU SHOULD KNOW BEFORE THE PNLE DECEMBER 2012 PNLE PEARLS OF SUCCESS PART 1: FUNDAMENTALS OF NURSING Vit.K Leafy green vegetables, particularly the BREAST dark green ones such as: Spinach, Broccoli, Malunggay, Avocado Vit. C Tomatoes, guava, papaya, citrus fruits Folic Acid Asparagus, organ meat, green leafy vegetables Vit. B ( foods rich in protein ) Calcium and Milk, cheese, green leafy vegetables, Phosphorus whole grains, seafood, tofu Iron Pork liver, lean meat, kamote leaves, soybeans, seaweeds, mongo Iodine Iodized salt, seafood, milk, egg, bread IX. NURSING SKILLS ABDOMEN: Place the client in a supine position with the knees slightly flexed to relax abdominal muscles. A. Hygiene (Inspection,Auscultation,Percussion,Auscultation) A complete bed bath consists of washing a dependent client’s entire body in bed; a complete bed bath with assistance involves helping the client to wash. C. Vital Signs A partial bed bath consists of or buttocks that may cause discomfort or odor if le washing only parts of the client’s Temperature (NV 36 – 37.5 C) body such as feet ft unwashed. Elderly people are at risk of hypothermia A tub bath or shower provides a more thorough Hard work or strenuous exercise can increase cleansing than a bed bath; the amount of nursing body temperature assistance is determined by the client’s age and health Oral: most accessible 2-3 mins. * 15 minutes and safety consideration. interval after ingestion of hot or cold drinks A therapeutic bath is ordered by a physician for a Rectal: most accurate 2-3 mins. specific purpose. Axillary: most safest 6-9 mins. Therapeutic baths include: Sitz bath – to reduce inflammation and clean the Pulse (NV 60-100 bpm) perineal area. Wave of blood created by contraction of the left Tepid sponge bath – to reduce fever. ventricle of the heart Medicated tub bath – to relieve skin irritation. Radial: best site for adult Brachial: best site for children Nursing Consideration Apical: best site for 3 years old below Avoid unnecessary exposure and chilling. Respiration (NV 12/16-20) Expose, wash, rinse and dry only a part of the body at one time. Normal Breath Sound Avoid draft Use correct temperature of water. Vesicular Soft, low pitch Lung periphery Observe the patient’s body closely for physical signs such as rashes, swelling, discoloration, sore, burns etc. Broncho- Medium pitch Larger airway Give special attention to the following body areas; vesicular blowing behind the ears, axilla, under the breast, umbilicus, Bronchial Loud, high pitch Trachea pubic region, groin and spaces between the fingers and toes. Abnormal Breath Sound Do the bath quickly but unhurriedly, use even, smooth but firm strokes. Crackles Dependent lobes Random, sudden Use adequate amount of water and change as reinflation of alveoli frequently as necessary. fluids If possible, do such procedure as vaginal douche, Rhonchi Trachea, bronchi Fluids, mucus enema, shampoo, oral care etc. before bath. Wheezes All lung fields Severely narrowed bronchus B. Physical Assessment Pleural Lateral lung field Inflamed Pleura Provide privacy. Friction Rub Make sure that all needed instruments are available before starting the physical assessment Be systematic and organized when assessing the client. Blood Pressure (NV 120/80 mm/hg) Inspection, Palpation, Percussion, Auscultation. This is the force exerted by the blood against a EYES: Visual acuity is tested using a snellen chart. The vessel wall room used for this test should be well lighted The pressure rises with age. EARS: Weber’s Test assesses bone conduction, this is a A rest of 30 minutes is indicated before the blood test of sound lateralization, Rinne Test compares bone pressure can be readily assessed after stressful conduction with air condition. activity. NECK: Let the client sit on a chair while the examiner Interval of 30 minutes is needed after smoking or stands behind him. drinking caffeine. THORAX: The client should be sitting upright without After menopause, women generally have higher support and uncovered to the waist. blood pressures than before. HEART: Anatomic areas for auscultation of the heart Pressure is usually lowest early in the morning, Aortic valve – Right 2nd ICS sternal border. when the metabolic rate is lowest, then rises Pulmonic Valve – Left 2nd ICS sternal border. throughout the day and peaks in the late afternoon Tricuspid Valve – – Left 5th ICS sternal border. or early evening Mitral Valve – Left 5th ICS midclavicular line POSSIBLE TOPICS ON FUNDAMENTALS OF NURSING FOR THE UPCOMING DECEMBER 2012 PNLE *Patterned on the previous board exams from December 2006 – July 2012… the purpose of this note is to GUIDE students on the possible topics that might be part of the upcoming December 2012 PNLE
- 4. WHAT YOU SHOULD KNOW BEFORE THE PNLE DECEMBER 2012 PNLE PEARLS OF SUCCESS PART 1: FUNDAMENTALS OF NURSING Common Errors in Blood Pressure Assessment D. Urinary Catheterization Errors Effect Use appropriate size of catheter Bladder cuff too narrow Erroneously high Male: Fr 16-18 Bladder cuff too wide Erroneously high Female: Fr 12-14 Place the client in appropriate position: Arm unsupported Erroneously high Male: Supine, legs abducted and extended Insufficient rest before the Erroneously high Female: Dorsal recumbent assessment Locate the urinary meatus properly: Repeating assessment too Erroneously high Male: at the tip of the glans penis quickly Female: between the clitoris and vaginal orifice Cuff wrapped too loosely or Erroneously low Lubricate catheter with water soluble lubricant before unevenly insertion Deflating cuff too quickly Erroneously low systolic and Male: 6 – 7 inches high diastolic reading Female: 1 – 2 inches Deflating cuff too slowly Erroneously high diastolic Length of catheter insertion: reading Male: 6 – 9 inches Failure to use the same arm Inconsistent measurements Female: 3 -4 inches consistently Anchor catheter properly: Arm above level of the heart Erroneously low Male: laterally or upward over the lower abdomen / Assessing immediately after a Erroneously high upper thigh meal or while client smokes Female: inner aspect of the thigh Failure to identify Erroneously low systolic auscultatory gap pressure pressure and erroneously low Nursing Interventions to Induce Voiding/Urination diastolic Provide privacy Assist the patient in the anatomical position of voiding D. Medication Administration Serve clean, warm and dry bedpan (female) or urinal (male) FIVE RIGHTS Allow the client to listen to the sound of running water The Right Drug with Dangle fingers in warm water The Right Dose through Pour warm water over the perineum The Right Route at Promote relaxation The Right Time to Provide adequate time for voiding The Right Patient Last resort: URINARY CATHETERIZATION Standard Order, Carried out until cancelled by another order. E. Nasogastric Tube (NGT) PRN Order, As needed, or only when necessary. Stat Order, Carried out immediately and for one time Gavage (feeding) / Lavage (suctioning) only. Select the nostril that has greater airflow. Always clarify doubtful /unclear order Assist the client to a high fowler’s position Do not leave medicine with the client to take by himself NEX technique (nose-ear-xiphoid) Do not give drug that shows physical changes or Checking the patency: deterioration Aspirate stomach contents and check the pH, Report an error in medication immediately to the nurse which should be acidic in charge. Introduce 10-30 ml of air into the NGT and Check medication 3 times before taking to the client: auscultate at the epigastric area, gurgling sound is o When taking the medication from the storage area heard o Before placing medication into the medicine The most accurate method of assessing the rack/glass placement of NGT is X-ray study o Before placing medicine to the storage area Before feeding assess residual feeding contents. To assess The nurse who prepares the medication must be absorption of the last feeding, if 50 ml or more, verify if the responsible for administering and recording it. Never feeding will be given. endorse it to another nurse. Height of feeding is 12 inches above the point of Always observe asepsis in preparing and administering insertion. drugs. Ask the client to remain in position for at least 30 min Ascertain client’s identity before administering Common Problems of Tube Feedings medications. Check room or bed or card, call out client’s Vomiting name, check I.D., wrist band Aspiration Care must be taken to prevent instilling medication Diarrhea directly into cornea. Hyperglycemia ORAL: If patient vomits within 20 – 30 minutes of taking the drug, notify the physician. Do not re-administer the F. Enema Administration drug without doctor’s orders. SUBLINGUAL ROUTE – drugs that is placed under the Position the client: tongue, where it dissolves. Adult: Left lateral BUCCAL ROUTE – a medication is held in the mouth Infant/small children: Dorsal recumbent against the mucous membranes of the cheek until the drugs Lubricate the tube about 5 cm ( 2 in ) dissolves Insert 7 – 10 cm ( 3 to 4 inches) or rectal tube gently EYES MEDS: Apply ointment along inside edge of the in rotating motion lower eyelid from inner to outer canthus. Raise the solution container and open the clamp to EAR MEDS: allow fluid to flow Infants: draw the auricle gently downward and High Enema: 12-18 inches above the rectum backward. Low Enema: 12 inches above the rectum Adults: lift pinna upward and backward If the client complains of fullness or pain, use the Intradermal: Parallel to the skin, do not massage clamp to stop the flow for 30 sec. and then restart the Subcutaneous: 45 degree above the skin, if obese 90 flow at a slower rate degree Encourage the client to retain the enema, ask the Intramuscular: 90 degree above the skin, aspirate to client to remain lying down check if blood vessel was hit. POSSIBLE TOPICS ON FUNDAMENTALS OF NURSING FOR THE UPCOMING DECEMBER 2012 PNLE *Patterned on the previous board exams from December 2006 – July 2012… the purpose of this note is to GUIDE students on the possible topics that might be part of the upcoming December 2012 PNLE
- 5. WHAT YOU SHOULD KNOW BEFORE THE PNLE DECEMBER 2012 PNLE PEARLS OF SUCCESS PART 1: FUNDAMENTALS OF NURSING Check for cross matching and blood typing. To ensure G. Colostomy Care compatibility Obtain and record baseline VS, Note: If patient has Stoma should appear red, similar to the mucosal linin fever do not transfuse of the inner cheek Practice strict, ASEPSIS Slight bleeding initially when the stoma is touched is At least 2 nurses check the label of the blood normal, but other bleeding should be reported. transfusion, Check the following: Change colostomy appliance if it is 1/3 full. - Serial Number Use warm water, mild soap (optional), and cotton - Blood component balls or a washcloth and towel to clean the skin and - Blood type stoma. - Rh factor Apply skin barrier over the skin around the stoma to - Expiration date prevent skin breakdown. - Screening test Changing is best in the morning before breakfast. Check the blood for gas bubbles and any unusual color Control Odor: (deodorizer, charcoal disk and prevent or cloudiness. Note: Gas bubbles indicate bacterial odor causing foods) growth, Unusual color or cloudiness indicate hemolysis Type of Discharge Warm blood at room temperature before transfusion. Ileostomy Liquid fecal drainage Identify client properly, two nurses check the client’s Drainage is constant and cannot identification be regulated Gauge of needle: #18 Contains some digestive enzymes Drop Factor: KVO Odor is minimal bec of fewer Duration: RBC – 4 hours; bacteria are present Platelets, FFP – 20 minutes Ascending Colostomy Liquid fecal drainage When reactions occurs: STOP transfusion Drainage is constant and cannot KVO with PNSS be regulated Send remaining blood, a sample of client blood Odor is a problem requiring and urine sample to the laboratory. control Notify the physician Transverse Malodorous, mushy drainage Monitor VS Colostomy Monitor I & O Descending Solid fecal drainage Common BT reactions: Colostomy Hemolytic: flank /back pain Sigmoidostomy Normal fecal characteristics Anaphylactic: rashes, itching, DOB (worst) Febrile: fever and chills Circulatory Overload: DOB, crackles H. Suctioning Sepsis: Fever and chills Suction only when necessary not routinely Use the smallest suction catheter if possible K. Assistive Device Client should be in semi or high Fowler’s position Use sterile gloves, sterile suction catheter Canes Hyperventilate client with 100% oxygen before and COAL (cane opposite affected leg) after suctioning Angel is 20-30 degrees Insert catheter with gloved hand (3-5“ length of Walkers catheter insertion) without applying suction. Three Hand bar below the client’s waist and the elbow is passes of the catheter is the maximum, with 10 slightly flexed. seconds per pass. Crutches Apply suction only during withdrawal of catheter Length of the Crutches: Subtract 40 cm or 16 The suction pressure should be limited to less than inches to the height of the client obtain the 120 mmHg approximate crutch length. When withdrawing catheter rotate while applying 20 to 30 degrees of flexion at the elbow. intermittent suction Four point gait: Suctioning should take only 10 seconds (maximum of * right crutch, the left foot, the left crutch, right 15 seconds) foot. Two point gait: * left foot and right crutch, right foot and left I. Tracheostomy Care crutch Three point gait: Assist the client to a semi-Fowler’s or Fowlers * left foot and both crutches, right foot. position. Hydrogen peroxide moisten and loosens dried Swing Through Gait: . * Advance both crutches, Lift both feet and swing secretions forward, Land the feet in front of crutches. Rinse the inner cannula thoroughly in the sterile Going up the stairs: (good goes to heaven, bad normal saline. goes to hell) When changing the ties: tie one end of the new tie to the eye of the flange while leaving old ties in place. Put two fingers under the tapes before tying it. L. Chest Physiotheraphy ( CPT ) Steam Inhalation J. Blood Transfusion Place the client in Semi-Fowler’s position Cover the client’s eyes with washcloth to prevent irritation Compatible Incompatible Place the steam inhalator in a flat, stable surface. A A/O AB / B Place the spout 12 – 18 inches away from the B B/O AB / A client’s nose or adjust distance as necessary AB A / B / AB / O To be effective, render steam inhalation therapy O O A / B / AB for 15 – 20 minutes POSSIBLE TOPICS ON FUNDAMENTALS OF NURSING FOR THE UPCOMING DECEMBER 2012 PNLE *Patterned on the previous board exams from December 2006 – July 2012… the purpose of this note is to GUIDE students on the possible topics that might be part of the upcoming December 2012 PNLE
- 6. WHAT YOU SHOULD KNOW BEFORE THE PNLE DECEMBER 2012 PNLE PEARLS OF SUCCESS PART 1: FUNDAMENTALS OF NURSING If there is NO fluctuation in the water seal bottle, Postural drainage it may mean TWO things Use of gravity to aid in the drainage of secretions. Either the lungs have expanded or the system Patient is placed in various positions to promote is NOT functioning appropriately. flow of drainage from different lung segments In this situation, the nurse refers the using gravity. observation to the physician, who will order for Areas with secretions are placed higher than lung an X-ray to confirm the suspicion. segments to promote drainage. In the event that the water seal bottle breaks, Patient should maintain each position for 5-15 the nurse temporarily kinks the tube and must minutes depending on tolerability. obtain a receptacle or container with sterile water and immerse the tubing. She should obtain another set of sterile bottle as M. Closed Chest Drainage ( Thoracostomy Tube ) replacement. She should NEVER CLAMP the tube for a longer time to avoid tension Types of Bottle Drainage pneumothorax. One-bottle system In the event the tube accidentally is pulled The bottle serves as drainage and water-seal out, the nurse obtains vaselinized gauze and Immerse tip of the tube in 2-3 cm of sterile NSS covers the stoma. to create water-seal. She should immediately contact the physician. Keep bottle at least 2-3 feet below the level of the chest Observe for fluctuation of fluid along the tube. N. Oxygen Therapy The fluctuation synchronizes with the respiration. Nasal Cannula (24% - 45% ) at flow rate of 2 – 6 L/min. Observe for intermittent bubbling of fluid; Simple Face Mask (40% - 60%) at liter flows of 5 - 8 continues bubbling means presence of air-leak L/min Partial Rebreather Mask (60% - 90%) at liter flows of In the absence of fluctuation: 6 – 10 L/min. Suspect obstruction of the device Non-Rebreather Mask (95% - 100%) at liter flows of Assess the patient first, then if patient is stable 10 – 15 L/min. Check for kinks along tubing; Oxygen is colorless, odorless, tasteless and a dry gas that Milk tubing towards the bottle (If the hospital support combustion, therefore leakage cannot be allows the nurse to milk the tube) detected. If there is no obstruction, consider lung re- Place cautionary signs reading “ No SMOKING: Oxygen expansion; (validated by chest x-ray) in Use” Air vent should be open to air. Avoid materials that generate static electricity, such as woolen blankets and synthetic fibers. Two-bottle system Set up the oxygen equipment and the humidifier filled If not connected to the suction apparatus with distilled/sterile water. The first bottle is drainage bottle; The second bottle is water-seal bottle CANNULA: Put over the client’s face, with the outlet Observe for fluctuation of fluid along the tube prongs fitting into the nares. (water-seal bottle or the second bottle) and FACE MASK: Fit the mask to the contours of the client’s intermittent bubbling with each respiration. face, apply it from the nose downward Three-bottle system The first bottle is the drainage bottle; The second bottle is water seal bottle The third bottle is suction control bottle. Observe for intermittent bubbling and fluctuation with respiration in the water- seal bottle Continuous GENTLE bubbling in the suction control bottle. Suspect a leak if there is continuous bubbling in the WATER seal bottle or if there is VIGOROUS bubbling in the suction control bottle. The nurse should look for the leak and report the observation at once. Never clamp the tubing unnecessarily. POSSIBLE TOPICS ON FUNDAMENTALS OF NURSING FOR THE UPCOMING DECEMBER 2012 PNLE *Patterned on the previous board exams from December 2006 – July 2012… the purpose of this note is to GUIDE students on the possible topics that might be part of the upcoming December 2012 PNLE
