MELA Sciences - Winter Clinical Dermatology Conference
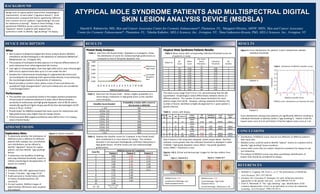
- 1. BACKGROUND ATYPICAL MOLE SYNDROME PATIENTS AND MULTISPECTRAL DIGITAL SKIN LESION ANALYSIS DEVICE (MSDSLA) Harold S. Rabinovitz, MD, Skin and Cancer Associates Center for Cosmetic Enhancement®, Plantation, FL; Margaret Oliviero, ARNP, MSN, Skin and Cancer Associates Center for Cosmetic Enhancement®, Plantation, FL; Nikolai Kabelev, MELA Sciences, Inc., Irvington, NY; Dina Gutkowicz-Krusin, PhD, MELA Sciences, Inc., Irvington, NY DEVICE DESCRIPTION RESULTS What: Pivotal Study Analyses: Performance: The classifier was successfully tested in the largest positive prospective clinical study of melanoma detection to date, which demonstrated a sensitivity to melanomas and high grade dysplastic nevi of 98.3% with a statistically significant higher biopsy specificity than dermatologists (9.9% versus 3.7% (p = 0.022).1 Pivotal study1 for MSDSLA showed that mean scores for melanomas and high grade lesions were higher than for benign lesions. Performed with 98% negative predictive value (NPV) and a 7.6:1 biopsy ratio in Pivotal Study.1 AIMS/METHODS Exploratory Aims: To determine whether the distribution of MSDSLA scores is different for different patients with multiple nevi, and whether such distributions can be utilized to identify “signature” lesions for a given patient, and thus identify “ugly duckling” lesions. To determine the feasibility of defining and using individual thresholds based on relative morphological disorganization of lesions on a patient. Methods: 10 Patients with 200+ pigmented lesions. 5 males, 5 females : Age range 31-62. 9 with personal or family history of MM, or history of basal/squamous cell carcinoma. For each patient, MSDSLA images of approximately 100 lesions were acquired and analyzed . Figure 1. Patient Examples Atypical Mole Syndrome Patients Results: Table 1. Data from the Pivotal Study1, displayed as a histogram, shows the distribution of scores for melanomas/high grade lesions as compared to that of low grade dysplastic nevi. Frequency of occurrence Non-invasive multispectral digital skin lesion analysis device, MSDSLA, intended to aid dermatologists in the detection of melanoma (MelaFind®, MelaSciences, Inc., Irvington, NY). The purpose of multispectral data capture is to improve differentiation of early melanoma from other pigmented skin lesions. Uses light of 10 wavelengths, from blue light (430 nm) to near infrared light (950 nm) to capture lesion data up to 2.5 mm under the skin. Samples the 3-dimensional morphology of a pigmented skin lesion and surrounding skin by analyzing multi-spectral data directly, or by enhancing the morphological patterns characteristic of melanoma. Result provides a numeric value, where scores of zero and above are considered “High Disorganization” and scores below zero are considered “Low Disorganization.” RESULTS Table 4. Mean scores with corresponding individual threshold scores for all patients in study. Patient ID 0.800 No. Cases Mean Score 1 2 3 4 5 6 7 8 9 10 1.000 97 102 103 102 104 101 95 99 102 103 0.56 1.29 1.61 0.22 0.78 0.45 0.92 0.75 1.54 0.63 Melanoma + High Grade 0.600 0.400 Low Grade Dysplastic Nevi 0.200 0.000 -6 -5 -4 -3 -2 -1 0 1 2 3 4 5 6 7 8 9 10 MSDSLA Classifier Score Table 2. Data from the Pivotal Study1. Shows a higher probability of a lesion being a melanoma or high grade lesion as the classifier score increases. Probability a lesion with a score in Classifier Score Bracket this bracket is MM/HG < -2.0 5% -2.0 to -1.0 3% -1.0 to 0.0 1% 0.0 to 1.0 3% 1.0 to 2.0 7% 2.0 to 3.0 10% 3.0 to 4.0 23% 4.0 to 5.0 28% 5.0 to 6.0 26% > 6.0 42% Table 3. Displays the classifier scores for 3 patients in the Pivotal Study1 who contributed 6 or more lesions for biopsy. The numbers denoted in red represent histologically confirmed melanomas or high-grade lesions. All other lesions are non-melanoma/high grade lesions. MSDSLA Scores for 3 patients Case No. Patient 1 Patient 2 Patient 3 1 4.83 5.26 6.11 2 2.52 4.42 2.74 3 2.42 3.76 2.19 4 1.85 2.95 1.54 5 1.81 2.72 1.30 6 1.81 2.43 0.11 7 1.71 2.40 8 1.31 2.26 9 1.17 1.99 10 1.15 1.63 11 1.06 0.68, 0.08, -0.06, 12 - 16 -0.21, -0.80 No. Cases above Threshold = 0 70 91 95 60 72 67 79 75 89 68 Individual Threshold No. Outliers 3.06 3.86 4.12 2.97 4.19 3.43 4.15 3.73 4.63 4.06 2 3 1 3 0 4 1 3 0 2 Figure 3. Score distributions for patients 3 and 4. Dotted lines indicate individual thresholds Table 6. Distribution of MSDSLA Classifier Scores 0.6 0.5 Patient 3 Age Lesion # 2 F 31 13 2 2 F F 31 31 22 98 6 7 M F 31 54 34 104 Lesion Location Upper back Upper back Leg Lower Back Forearm MF Score Individual Threshold Local Path Central Path 2.59 3.86 NDHG NDLG 2.45 4.73 3.86 3.86 NDLG NDLG NDLG NDLG 0.33 5.95 3.43 4.15 NDLG NDHG NDLG MMIS Only 5 lesions in the study were biopsied, results shown above. Red font indicates scores greater than the individual threshold as displayed in table 4 (NDHG = high grade dysplastic nevus; NDLG = low grade dysplastic nevus; MMIS = melanoma in situ). Figures 1 & 2. Clinical and dermoscopic images for the two outliers from Table 5 Figure 1. Patient ID 2 0.3 0.2 0 -4 -2 0 2 4 Figure 2. Patient ID 7 MSDSLA score distributions are Gaussian (KS test). Score distributions among some patients are significantly different resulting in individual thresholds to identify outliers (“ugly ducklings”). Patient 4 had the lowest mean score of 0.22 and Patient 3 had the highest mean score at 1.61 CONCLUSIONS Distributions of MSDSLA scores may be very different on different patients with many nevi. MSDSLA scores could be used to identify “typical” lesions on a patient and to identify “ugly duckling” lesions (outliers). Lesions with scores that are outliers should be considered for biopsy to rule out melanoma. The analysis of MSDSLA scores may allow quantitative identification of outliers that should be considered for biopsy. REFERENCES MSDSLA Score: 4.73 MSDSLA Score: 5.95 Local/Central Pathology: Low Grade Dysplastic Nevus Local Pathology: High Grade Dysplastic Nevus Central Pathology: Melanoma in situ 6 MSDSLA Classifier Score Patient 4 Table 5. Lesions with biopsy. Sex 0.4 0.1 The mean scores range from 0.22 to 1.61, demonstrating that the qM (quantitative morphological value) differentiates between lesions on different patients. The number of cases above threshold 0 for each patient ranges from 60-95. However, utilizing individual thresholds, the number of lesions identified as highly disorganized for a given patient is greatly reduced. Patient ID Distribution Benign nevi on a given patient have similar morphological characteristics to each other2 (“signature lesions”). Grob and Bonerandi proposed that lesions significantly different from common nevi on a patient (“ugly ducklings”) be used for melanoma screening3. Based on these findings, it was questioned if MSDSLA can be used to identify these “signature” lesions in patients with atypical mole syndrome in order to identify “ugly ducklings” for biopsy. 1. Monheit G, Cognetta AB, Ferris L, et al. The performance of MelaFind. Arch Dermatol. 2011;147:188-94. 2. Goodson AG, Grossman D. Strategies for early melanoma detection: approaches to the patient with nevi. JAAD 2009;60:719-38. 3. Grob JJ, Bonerandi JJ. The “ugly duckling” sign: identification of the common characteristics of nevi in an individual as a basis for melanoma screening. Arch Dermatol. 1998;134:103-4.
- 2. Atypical Mole Syndrome Patients and Multispectral Digital Skin Lesion Analysis Device (MSDSLA) Harold Rabinovitz, MD; Margaret Oliviero, ARNP; Nikolai Kabelev; Dina Gutkowicz-Krusin, PhD Introduction: A multispectral digital skin lesion analysis device (MSDSLA) (MelaFind®: MELA Sciences, Inc., Irvington, NY), uses light imaging technology and analysis software to provide a numeric value that characterizes the 3 dimensional morphological disorganization of clinically atypical pigmented skin lesions. Classifier scores of zero and above indicate “High Disorganization” and classifier scores below zero indicate “Low Disorganization.” Objective: Since benign nevi on a given patient share similar morphological characteristics, it was investigated whether MSDSLA scores can be used to identify “typical” lesions on individual patients, and conversely be used to identify “ugly ducklings”. A pivotal study for the MSDSLA device showed that classifier scores for melanomas and high-grade lesions tended to be higher than scores for benign lesions on patients with multiple nevi. Methods: Patients (N=10) with at least 200 nevi were selected by an examining dermatologist who was also a pigmented skin lesion expert in a clinical setting; approximately 100 lesions on each patient were evaluated with MSDSLA. Five patients were male, and five patients were female; nine had a personal or family history of melanoma or a personal history of non-melanoma skin cancer. MSDSLA score distributions for all patients and for each individual patient were analyzed using the Kolmogorov-Smirnov test to determine normal distribution of scores. Tentative individual thresholds were then proposed so that the probability of finding scores greater than the threshold value for each individual was less than 1% for a normal distribution of scores. Results: MSDSLA score distribution was Gaussian; score distributions among some patients were significantly different. Individual thresholds for each patient were calculated using mean score plus 2.33 standard deviations; individual thresholds ranged from 2.8 for one patient to 4.5 for another patient. Seventy-six percent of lesions were above the threshold (“0”) used for the general population as opposed to only 2.1% of lesions above the proposed individual thresholds as calculated for each patient. Conclusions: Distribution of MSDSLA scores may be very different on different patients with many nevi. MSDSLA scores may be used to identify “typical” lesions on a patient and to also identify “ugly duckling” lesions (outliers). Individual thresholds for these types of patients may be determined through baseline imaging with MSDSLA (10-15 lesions). Lesions with scores that are outliers should be considered for biopsy to rule out melanoma. The analysis of MSDSLA scores may allow quantitative identification of outlier lesions that should be considered for biopsy. Monheit, G et al. The Performance of MelaFind: A Prospective Multicenter Study. Arch Dermatol Oct 2010: E1-E7
- 3. Case Study: Use of a Multispectral Digital Skin Lesion Analysis Device (MSDSLA) in Pediatrics and Young Adults Dr. med. Marcella Kollmann-Hemmerich, Munich, Germany BACKGROUND Introduction Two reader studies were conducted presenting high resolution images and case histories for 130 pigmented skin lesions to dermatologists in the U.S. (n = 110)5 and in Germany5 (n = 101). After reviewing the case, dermatologists were asked to provide their lesion management decisions. C A S E S T U D I E S – Y O U N G A D U LT S READER STUDY REVIEW Differentiation of early melanomas from benign lesions in young adults (16 – 25) can be difficult clinically. Incidence of melanoma in children and adolescents has increased at an annual rate of 2.0% per year from 1973 to 2009.1 Biopsy ratio of up to 80 to 1 have been observed in younger patients. 2 Melanoma is the most common cancer in young adults aged 20 to 30. 3 MSDSLA can be used to help dermatologists decide which lesions may be suspicious for melanoma by providing information about the structure of a lesion from under the skin (MelaFind; MELA Sciences, Inc.). Pivotal Study The pivotal study for MSDSLA (MelaFind®: Irvington, NY) established that it was a safe and effective device by demonstrating high sensitivity to melanomas and high grade dysplastic nevi (98.3%) and better specificity than study clinicians (9.9% vs. 3.7%, p = 0.022).4 In the pivotal study, 183 lesions from young adult patients aged 16 to 25 were enrolled; of these, 13 were melanomas or high grade lesions, 11 of which were correctly considered MSDSLA “High Disorganization.” Of the 11 melanomas enrolled from young adults, all were invasive, except one melanoma in situ, with median Breslow thickness of 0.50 mm. Sensitivity of both U.S. and German dermatologists were 72% and 70%, respectively. 5 melanomas from young adult patients, all invasive, were randomly selected for review by these 211 dermatologists (Table 1). CASE STUDY # 1: MSDSLA Dermoscopic Image 17 year old female; regular skin visits CASE STUDY # 2: 24 year old male Lesion appeared within 4 months of excision and grew within that time > 50 nevi (none dysplastic) No family history of melanoma No risk factors for melanoma Fitzpatrick Skin Type II-III Lesion Location Lesion clinically unsuspicious over 3 yrs Clinical diagnosis: Spitz/Reed Nevus Pathology: melanoma in situ MSDSLA score: 3.5 Pathology: melanoma in situ MSDSLA Multispectral Images: MSDSLA Multispectral Images: 430 nm Clinical Dermoscopic Patient Age 500 nm 510 nm 600 nm 430 nm 460 nm 500 nm 510 nm 600 nm 660 nm Breslow (mm) 460 nm 700 nm 780 nm 880 nm 950 nm 660 nm 700 nm 780 nm 880 nm 950 nm % of dermatologists electing NOT to biopsy Table 1. Characteristics of Young Adults (pivotal study) Histology: Histology: % (N = 136) Female Male Asian or Pacific Highlander White RACE Other Mean Median AGE Standard Deviation I II FITZPATRICK SKIN TYPE III IV HISTORY OF DYSPLASTIC NEVI* 66.2% 33.8% 3.7% 95.6% 0.7% 21 21 2.8 5.1% 51.5% 36.0% 7.4% 29.0% HISTORY OF MELANOMA FAMILY HISTORY OF MELANOMA** 20.2% BLONDE/RED HAIR 0.32 24 1.9% 0.17 24 48.6% 0.60 18 57.3% 7.4% 40.4% SEX BLUE/GREEN EYES NUMBER OF NEVI USE OF TANNING BED CONCLUSIONS *five values were “unknown”; ** twelve values were “unknown” 37.5% 36.8% 13.2% 12.5% 40.4% 23.5% 14.7% 21.3% REFERENCES 1 Wong 0.70 17 46.0% 1. Melanomas on young adult patients can be difficult to detect. 63.2% 1-10 11-30 31-50 > 50 Never 1-10 times 11-24 times > 24 times Lesion Location MSDSLA score: 3.3 Table 2. Melanomas from young adults on reader studies A total of 136 young adults were enrolled on the pivotal study; none had a history of pigmented basal or squamous cell carcinoma. Table 1 shows characteristics of these young adults. Baseline Characteristics MSDSLA Dermoscopic Image 0.28 0.15 25 25 78.1% 76.2% 2. MSDSLA can be helpful in assisting in the detection of early melanomas within young adults, a population where melanoma incidence is on the rise. JR. Pediatrics. 2013;doi:10.1542/peds.2012-2520 2 English et al. Med J Aust. 2004 P, Borden EC. Malignant Melanoma: Treatments Emerging, but early detection is still key. Cleveland Clinic Journal of Medicine July 2002; Vo. 69 # 7: 529-545. 3 Masci 4 Monheit G, Cognetta AB, Ferris L, et al. The performance of MelaFind: a prospective multicenter study. Arch Dermatol. 2011;147:188-94. 5 Chen SC, Wells R and Adrian J. (2011, February). Performance of an adjuvant melanoma detection tool compared to physicians. Poster presented at the American Academy of Dermatology, New Orleans, LA. 6 Hauschild, Axel. Protocol 20101: To Excise or Not?: Comparing Clinical Management Decisions for Melanoma Between Dermatologists with and without the Aid of MelaFind. University of Kiel, Kiel, Germany. Unpublished data; August 2012. Funded in part by a grant from MELA Sciences, Inc.
- 4. Analysis of Pigmented Skin Lesions in Young Adults with A Multispectral Digital Skin Lesion Analysis Device (MSDSLA) Marcella Kollmann, MD Background: The incidence of melanoma is increasing worldwide, particularly in young adults, a group in which melanoma detection can be problematic. MelaFind®, a multispectral digital skin lesion analysis device (MSDSLA), is a non-invasive and objective instrument that dermatologists can use to help determine whether a pigmented skin lesion is suspicious and should be biopsied to rule out melanoma (MelaFind ®, MELA Sciences, Inc., Irvington, NY). A previous clinical trial had established the safety and effectiveness of this device using sensitivity and specificity as metrics. This device is presently in use at various dermatologist practices in the United States and in Germany. Objective: To investigate the utility of a multispectral digital skin lesion analysis device in the diagnosis of suspicious pigmented skin lesions in young adults. Methods: Data reviewed for these analyses were as follows: 1) real-world case study data from a 17 year-old female and a 24 year-old male evaluated with MSDSLA in clinical practice, 2) MSDSLA and clinical data on 183 lesions evaluated from young adults (ages 16 to 25) enrolled onto the pivotal study for the device1, and 3) six melanomas from young adults who participated in the pivotal study which were subsequently reviewed in a reader study format by 211 U.S. and German dermatologists. Results: In clinical practice, the MSDSLA device assisted in the detection of a melanoma in a male patient aged 17 and one in a female patient aged 24. In the pivotal study1, 183 lesions from young adult patients were examined; of these, 13 were melanomas or high-grade lesions, 11 of which were correctly considered by the MSDSLA as possessing “High Disorganization”. Six of the 13 melanomas from young adult patients in the pivotal study1 were also reviewed in two separate, but similar, reader studies consisting of 110 U.S. dermatologists and 101 German dermatologists who provided their lesion management decisions for atypical lesions based upon review of high-resolution clinical and dermoscopic images as well as detailed patient and lesion information. Average false negative rates of the combined 211 dermatologists for these melanomas were as follows (median Breslow in parenthesis): 48.6% (0.17 mm), 57.3% (0.60 mm), 1.9% (0.32 mm), 76.2% (0.15 mm), 46.0% (0.70 mm), and 78.1% (0.28 mm). Conclusions: Melanomas on young adult patients can be difficult to detect. MSDSLA may be helpful in the detection of early melanomas within young adults, a population where the incidence of melanoma is on the rise. Monheit, G et al. The Performance of MelaFind: A Prospective Multicenter Study. Arch Dermatol Oct 2010: E1-E7
- 5. Assessing the Predictive Probability of Melanoma and Other High Risk Pigmented Lesions Using Data Provided by a Multispectral Digital Skin Lesion Analysis Device Jane Yoo, MD MPP*; Natalie Tucker, BS**; Darrell S. Rigel, MD MS*** *Dept. of Dermatology, Albert Einstein School of Medicine, Bronx, NY; **MELA Sciences, Irvington, NY; ***Dept. of Dermatology, NYU School of Medicine, NYC, NY Introduction Risk prediction models are often used as research tools to help identify individuals at high risk of specific cancers in the general population. Developing statistical models that evaluate the probability of developing cancer over a defined period of time allows for earlier or more frequent screening and counseling as well as earlier intervention and treatment. While many different diagnostic tools for melanoma have emerged in the past decade, very few have quantified their predictive capacity for melanoma or other high risk pigmented lesions. MSDSLA Classifier Score Description A Mulltispectral Digital Skin Lesion Analysis device (MSDSLA), (MelaFind®, MelaSciences, Inc., Irvington, NY) combines multispectral data acquisition and novel feature generation with automatic quantitative analysis. The automatic quantitative analysis utilizes a lesion classifier score derived from 75 features to evaluate the degree of 3-dimensional morphological disorganization of pigmented skin lesions. MSDSLA was successfully tested in the largest positive prospective clinical study of melanoma detection to date, which demonstrated a sensitivity to melanomas and high grade dysplastic nevi of 98.3% with a statistically significant higher biopsy specificity than dermatologists (9.9% versus 3.7%, p = 0.022)1. In this study, the classifier scores ranged from 5.25 to +9.00. Of note, scores below zero are considered to be indicative of “low disorganization” and scores of zero and above are considered indicative of “high disorganization.” Methods Data from 1632 pigmented lesions analyzed by MSDSLA were used to perform a logistic regression analysis using Stata v12 (College Station, Tx).1 Final pathological diagnoses were assigned to four distinct categories: 1) High grade dysplastic nevus (HGDN), 2) Atypical melanocytic hyperplasia (AMH), 3) Malignant melanoma (MM) or, 4) Other The MSDSLA device assigns classifier scores to pigmented lesions, which were considered as dependent variables. Using the MSDSLA derived classifier score (a numerical value based on analytical values from a lesion’s level of structural disorder), we repeat logistical regression models to determine the probability distribution for Malignant Melanoma and for lesions that might be considered suitable for biopsy (Melanoma or Atypical Melanocytic Hyperplasia or High Grade Dysplastic Nevus). Results Case Examples Results Melanoma model: Melanoma/AMH/HGDN model: P = probability of melanoma = e (-3.8+0.53x) / 1+e (-3.8+0.53x) P = probability of MM/AMH/HGDN = e (-3.3+0.49x) / 1+e (-3.3+0.49x) or p/1-p=odds of melanoma or p / 1-p= odds of MM/AMH/HGDN For every one unit increase in the MSDSLA classifier score, the odds of favoring the presence of melanoma increased by 1.7. Melanoma Prediction Model For every one unit increase in the MSDSLA classifier score, the odds of favoring the presence of MM/AMH/HGDN increased by 1.6. Melanoma/AMH/HGDN Prediction Model Classifier Score Probability of MM Std. Error 95% Confidence Interval Classifier Score Probability MM/AMH/HGDN Std. Error 95% Confidence Interval -10 0.01% 0.01% -0.00%, 0.03% -10 0.03% 0.02% -0.00%, 0.06% -9 0.02% 0.01% -0.00%, 0.04% -9 0.05% 0.03% -0.00%, 0.10% -8 0.03% 0.02% -0.00%, 0.07% -8 0.07% 0.04% -0.00%, 0.15% -7 0.05% 0.03% -0.00%, 0.11% -7 0.12% 0.06% 0.01%, 0.23% -6 0.09% 0.04% 0.00%, 0.18% -6 0.20% 0.08% 0.03%, 0.36% -5 0.15% 0.07% 0.02%, 0.29% -5 0.32% 0.12% 0.08%, 0.56% -4 0.26% 0.10% 0.06%, 0.46% -4 0.52% 0.17% 0.17%, 0.86% -3 0.45% 0.15% 0.15%, 0.74% -3 0.84% 0.24% 0.36%, 1.32% -2 0.76% 0.22% 0.33%, 1.19% -2 1.35% 0.33% 0.70%, 2.01% -1 1.29% 0.31% 0.69%, 1.89% -1 2.18% 0.44% 1.33%, 3.04% 0 2.17% 0.41% 1.37%, 2.98% 0 3.50% 0.55% 1 3.65% 0.53% 2.62%, 4.69% 1 5.57% 0.65% 6.08% 0.65% 4.79%, 7.36% 2 8.75% 0.76% 7.27%, 10.23% where p is the calculated probability of melanoma and x1x 2 xi are explanatory variables. The model logit(p) = a + bx is equivalent to p = probability of melanoma (or of lesion of interest considered for biopsy) = e(a+bx) / 1+ e(a+bx) 3 9.94% 0.87% 8.23%, 11.66% 3 13.49% 0.98% 11.57%, 15.41% 4 15.85% 1.43% 13.04%, 18.66% 4 20.22% 1.58% 17.13%, 23.32% 5 24.32% 2.56% 19.31%, 29.34% 5 29.19% 2.67% 23.96%, 34.42% 6 35.42% 4.14% 27.30%, 43.53% 6 40.13% 4.04% 32.21%, 48.04% 7 48.34% 5.69% 37.18%, 59.49% 7 52.14% 5.26% 41.84%, 62.45% 8 61.49% 6.56% 48.62%, 74.35% 8 63.92% 5.88% 52.40%, 75.44% 9 73.15% 6.44% 60.53%, 85.76% 9 74.23% 5.74% 62.97%, 85.48% 10 82.29% 5.52% 71.47%, 93.12% 10 82.40% 5.02% 72.57%, 92.24% Clinical image Dermoscopic image Case Example # 2: Clinical diagnosis before MSDSLA: Not melanoma (Biopsied because of patient concern) Histological diagnosis: Melanoma in-situ Classifier Score: 4.21 Probability of melanoma: 17.4% Probability of MM/AMH/HGDN: 21.91% Clinical image 4.29%, 6.85% 2 Clinical diagnosis before MSDSLA: Likely melanoma (67-99%) Histological diagnosis: Invasive melanoma Breslow thickness: 0.36 mm Classifier Score: 8.15 Probability of melanoma: 63.33% Probability of MM/AMH/HGDN: 65.55% 2.42%, 4.58% logit(p) = a + b1 x1+ b 2 x 2 + ….+ bixi Case Example #1: Calculation The logistic regression model used in this study: 1. Monheit, G et al. The Performance of MelaFind: A Prospective Multicenter Study. Arch Dermatol 2011 Feb; 147 (2):188-94. Dermoscopic image Case Example #3: Clinical Diagnosis before MSDSLA: Likely melanoma (67-99%) Histological diagnosis: Low Grade Dysplastic Nevus Classifier Score: -1.56 Probability of melanoma: 1% Probability of MM/AMH/HGDN: 1.67% Clinical image Dermoscopic image Conclusions By performing a univariate logistic regression analysis, we were able to calculate the predictive probability of melanoma or a high risk pigmented lesion for consideration for biopsy based on data obtained from a multispectral digital skin lesion analysis device. This is the first study, to our knowledge, that has evaluated a dermatological technological instrument for its potential quantitative predictive capacity for presence of melanoma and other high risk pigmented lesions.
- 6. Assessing the Predictive Probability of Melanoma and Other High Risk Pigmented Lesions Using Data Provided by a Multispectral Digital Skin Lesion Analysis Device Jane Yoo, MD MPP*, Natalie Tucker**, Darrell S. Rigel, MD MS*** * Dept of Dermatology, Albert Einstein School of Medicine, Bronx, NY; ** MelaSciences, Irvington, NY; *** Clinical Professor of Dermatology, NYU School of Medicine, NYC, NY Introduction: Risk prediction models are often used as research tools to help identify individuals at high risk of specific cancers in the general population. Developing statistical models that evaluate the probability of developing cancer over a defined period of time allows for earlier or more frequent screening and counseling as well as earlier intervention and treatment. While many different diagnostic tools for melanoma have emerged in the past decade, very few have quantified their predictive capacity for melanoma or other high risk pigmented lesions. Methods: Data from 1,632 pigmented lesions analyzed by a Multispectral Digital Skin Lesion Analysis device (MSDSLA) (MelaFind®, MelaSciences, Inc., Irvington, NY) were used to perform a logistical regression analysis. The MSDSLA device assigns classifier scores to pigmented lesions. Final pathological diagnoses were assigned to four distinct categories: high grade dysplastic nevus, atypical melanocytic hyperplasia, malignant melanoma or other and used as the dependent variable. Using the MSDSLA derived classifier score (a numerical value based on analytical values from lesion’s level of structural disorder) we derived logistical regression models to determine the probability distribution for Malignant Melanoma and for lesions that might be considered suitable for biopsy (Melanoma or Atypical Melanocytic Hyperplasia or High Grade Dysplastic Nevus). The Logistic regression model used was: logit(p) =a + b1 x1+ b 2 x 2 + ….+ bixi where p is the calculated probability of melanoma and x1x 2 xi are explanatory variables. The model logit(p)=a+bx is equivalent to p=probability of melanoma (or of lesion considered for biopsy) = e^(a+bx) / 1+e^(a+bx) Results: For the Melanoma model: p=probability of melanoma = e (-3.1+0.49x) / 1+e (-3.1+0.49x) or p / 1-p= odds of melanoma For every one increase in unit in the MSDSLA classifier score, the odds of favoring the presence of melanoma increased by 1.3. For the Melanoma/AMH/HGDN model: p=probability of MM/AMH/HGDN = e (-3.8+0.53x) / 1+e (-3.8+0.53x) or p/1-p=odds of MM/AMH/HGDN For every one unit increase the MSDSLA classifier score, the odds of favoring the presence of MM/AMH/HGDN increased by 1.7. Conclusion: By performing a multifactorial logistical regression analysis, we were able to calculate the predictive probability of a pigmented lesion for melanoma or for consideration for biopsy based on data obtained from a multispectral digital skin lesion analysis skin lesion analysis device. This is the first study, to our knowledge, that has evaluated a dermatological technological instrument for its potential quantitative predictive capacity for presence of melanoma and other high risk pigmented lesions. Monheit, G et al. The Performance of MelaFind: A Prospective Multicenter Study. Arch Dermatol Oct 2010: E1-E7
- 7. Physical Properties, Novel Features and Clinical Validation of a Multispectral Digital Skin Lesion Analysis Device for Melanoma Detection Darrell S. Rigel, MD, MS, NYU School of Medicine, New York, NY; Laura Ferris, MD, PhD, University of Pittsburgh, Pittsburgh, PA; Arthur Sober, MD, Harvard University, Boston, MA; Clay J. Cockerell, MD, University of Texas Southwestern, Dallas, TX Multispectral Images and Analysis Description • MSDSLA is a non-invasive and objective computer vision system intended to aid dermatologists in the detection of melanoma (MelaFind®, Mela Sciences, Inc., Irvington, NY). • MSDSLA acquires multi-spectral data in 10 different spectral bands from blue light (430 nm) to near-infrared (950 nm).1 • MSDSLA uses information not visible to the human eye to characterize the morphological disorganization of pigmented skin lesions that are clinically ambiguous. Classifier Score By Lesion Type E X A M P L ES – M S D S L A D ATA LESION TYPE (N = 1632) Histologically Benign* Non-melanoma skin cancers High grade lesions Melanomas Path ology: In vasive M elan om a *excludes C lin ic a l O ve r vie w C lin ic a l C lo s e - u p Contribution • The purpose of multispectral data capture is to improve differentiation of cutaneous melanoma from other pigmented skin lesions. • Early melanomas may mimic benign look-alikes and present a challenge to clinicians. • MSDSLA provides information about the entire three dimensional structure of the lesion up to 2.5 mm in depth. • MSDSLA utilizes 20-micron resolution allowing it to discern clusters of 3 melanocytes. Classifier Score Description • MSDSLA combines multispectral data acquisition and novel feature generation with automatic quantitative analysis. • The lesion classifier uses 75 features (some with correlations) to evaluate the degree of 3-dimensional morphological disorganization of pigmented skin lesions. • This classifier was successfully tested in the largest positive prospective clinical study of melanoma detection to-date, which demonstrated a sensitivity to melanomas and high grade dysplastic nevi of 98.3% with a statistically significant higher biopsy specificity than dermatologists (9.9% versus 3.7%, p = 0.022).2 • In this study, the classifier scores ranged from -5.25 to +9.00; scores below zero were considered to be “low disorganization” and scores of zero and above were considered “high disorganization.” 1Gutkowicz-Krusin D, Elbaum M, Jacobs A, Keem S, Kopf AW, Kamino H, Wang S, Rubin P, Rabinovitz H, Oliviero M. Precision of automatic measurements of pigmented skin lesion parameters with a MelaFind(TM) multispectral digital dermoscope Melanoma Res. 2000 Dec;10(6):563-70. 2Monheit, G et al. The Performance of MelaFind: A Prospective Multicenter Study. Arch Dermatol 2011 Feb; 147 (2): 188-94 MEAN CLASSIFIER SCORE MEDIAN CLASSIFIER SCORE 1.74 2.64 2.68 3.47 1.61 2.56 2.51 3.49 melanomas, high grade lesions and non-melanoma skin cancers Table 1. The mean and median scores by lesion type, as observed on the pivotal study. Benign lesions had a mean score of 1.74, non-melanoma skin cancers 2.64, high grade lesions 2.68 and melanomas 3.47. D e r m o s c o p ic Classifier Score By Clinical Characteristics Path ology: Low Gr ad e Dysp lastic Nevu s Function • MSDSLA samples the 3-dimensional morphology of a pigmented skin lesion and surrounding skin by analyzing multi-spectral data directly or by enhancing the morphological patterns characteristic of melanoma. • Lesions are dark at short wavelengths due to strong absorption by superficial melanin. • With increasing wavelengths, images of a benign nevus tend to become uniformly brighter while images of a melanoma tend to show more irregular morphology. N 1424 33 48 127 NUMBER CLINICAL/HISTORICAL CHARACTERISTICS C lin ic a l C lo s e - u p MEAN CLASSIFIER SCORE MEDIAN CLASSIFIER SCORE 0 C lin ic a l O ve r vie w N 11 0.84 0.25 1 86 0.96 1.07 2 194 1.40 1.44 3 408 1.50 1.44 4 421 1.94 1.72 5 260 2.36 2.32 6 156 2.67 2.40 7 80 3.00 2.44 8 16 4.03 4.13 D e r m o s c o p ic MSDSLA visual representations of this invasive melanoma and low grade dysplastic nevus are displayed below MULTISPECTRAL ASYMMETRY TEXTURE STRUCTURE BAND WAVELENGTH DEPTH MELANOMA Band 0 NEVUS MELANOMA NEVUSMELANOMA NEVUS MELANOMA NEVUS 430 nm 0.4mm (blue/violet) Band 1 460 nm (blue) 0.7mm Band 2 500 nm (green) 0.8mm Band 3 510 nm (green) Table 2. For all lesions enrolled into the study, clinical or historical characteristics observed by the examining dermatologists were recorded. The more clinical or historical characteristics present, the higher the mean and median raw classifier scores. Characteristics include Asymmetry, Border Irregularity, Color Variegation, Diameter greater than 6 mm, Evolution, Patient’s Concern, Regression and/or Ugly Duckling. 0.9mm Performance by Varying Thresholds Band 6 Band 7 600 nm (red) 700 nm (red) 1.9mm 780 nm 2.0mm (near infrared) Band 8 880 nm 2.2mm (near infrared) Band 9 950 nm 2.5mm (near infrared) MelaFind discerns 5000 features, 75 of which are taken together to generate information about the morphological disorganization of a lesion. Multispectral data is transformed to enhance various features for analysis, such as asymmetry, texture and structure (displayed above) Benign lesion is more uniform, structured and robust in appearance for selected features displayed, from the blue to near infrared bands ≥ -3 100.0% (97.9-100%) 0.8% (0.4-1.4%) ≥ -2 99.4% (96.9-100%) 1.3% (0.8-2.0%) 98.9% (95.9-99.9%) 3.6% (2.7-4.7%) ≥0 98.3% (95.1-99.6%) 10.8% (9.2-12.5%) ≥1 1.7mm SPECIFICITY (95% CI) 93.1% (88.3-96.4%) 29.8% (27.4-32.2%) ≥2 75.4% (78.4-81.6%) 60.0% (57.4-62.5%) ≥3 54.3% (46.6-61.8%) 81.8% (79.7-83.8%) ≥4 Band 5 600 nm 1.3mm (yellow-green) SENSITIVITY (95% CI) ≥ -1 Band 4 THRESHOLD 30.9% (24.1-38.3%) 91.4% (89.9-92.8%) ≥5 15.4% (10.4-21.7%) 96.1% (95.0-97.0%) ≥6 7.4% (4.0-12.4%) 98.8% (98.2-99.4%) Table 3. The sensitivity and specificity at varying thresholds and 95% confidence intervals. As the threshold moves toward a higher classifier score, the sensitivity decreases and specificity increases. Conversely, as a negative classifier score threshold is set, the sensitivity increases and the specificity decreases. CONCLUSIONS: In this study, the classifier scores ranged from -5.25 to +9.00; scores below zero were considered to be “low disorganization” and scores of zero and above were considered “high disorganization.” The average classifier score of melanomas, high grade lesions, and non-melanoma/high grade lesions were 3.5, 2.7, 2.6, and 1.6, respectively, providing further clinical validation of the novel MSDSLA features.
- 8. Physical Properties, Novel Features and Clinical Validation of a Multispectral Digital Skin Lesion Analysis Device for Melanoma Detection Darrell S. Rigel, MD, MS; Laura Ferris, MD, PhD; Arthur Sober, MD; Clay Cockerell, MD Background: MSDSLA is a non-invasive and objective computer vision system intended to aid dermatologists in the detection of melanoma (MelaFind®, MelaSciences, Inc., Irvington, NY). Early melanomas may mimic benign look-alikes and therefore present a challenge to clinicians. By acquiring multi-spectral data in 10 different spectral bands from blue light (430 nm) to near infrared (950 nm), MSDSLA provides information about a lesion’s morphology up to 2.5 mm into the skin. MSDSLA uses this information, which is not interpretable to the human eye to characterize the morphological disorganization of pigmented skin lesions that are clinically ambiguous. Objectives: To retrospectively evaluate an automated quantitative analysis (“classifier score”) for pigmented lesions computed by a multi-spectral digital skin lesion analysis (MSDSLA) device relative to clinical characteristics and histopathology; this data was accrued in the largest positive prospective clinical study of melanoma detection to-date. Methods: MSDSLA samples the 3-dimensional morphology of a pigmented skin lesion and surrounding skin by analyzing information collected from 10 wavelengths of light or by enhancing morphological patterns characteristic of melanoma (examples are asymmetry, texture and structure). Pigmented skin lesions are darker at shorter wavelengths due to strong absorption by superficial melanin. MSDSLA provides images of the lesion at a depth of up to 2.5 mm. By using an algorithm that calculates 75 feature parameters, MSDSLA provides a numeric value characterizing the 3D morphological disorganization of pigmented skin lesions known as a “classifier score.” Scores of “0" and above are considered “high disorganization” and scores below “0” are considered “low disorganization”, in reference to the 3D morphological disorganization of the lesion. Results: Average classifier scores were higher for melanomas as compared with benign lesions (3.5 versus 1.7). Additionally, the average classifier scores tended to increase as the number of clinical or historical features of melanoma present in the lesion increased. The range of MSDSLA classifier scores observed in the pivotal study1 for all lesion types was between -5.2 to 9.0. The average classifier scores of melanomas, high-grade lesions, non-melanoma skin cancers and benign lesions were 3.5, 2.7, 2.6 and 1.7, respectively, providing further clinical validation of the MSDSLA. Conclusions: Data from the pivotal study shows that quantitative information about a lesion’s morphological disorganization (“classifier scores”), as computed by MSDSLA, correlates with the level of both histological and clinical irregularity. This information may be useful to dermatologists when deciding which clinically ambiguous lesions may need to be biopsied to rule out melanoma. Monheit, G et al. The Performance of MelaFind: A Prospective Multicenter Study. Arch Dermatol Oct 2010: E1-E7