Problem Oriented Pediatric Radiology
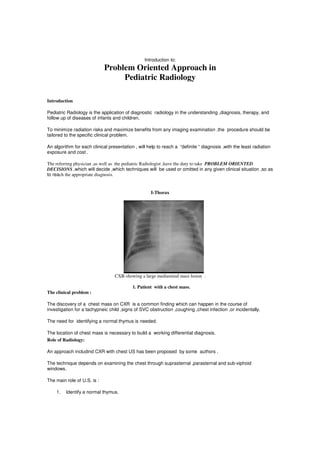
- 1. Introduction to: Problem Oriented Approach in Pediatric Radiology Introduction Pediatric Radiology is the application of diagnostic radiology in the understanding ,diagnosis, therapy, and follow up of diseases of infants and children. To minimize radiation risks and maximize benefits from any imaging examination ,the procedure should be tailored to the specific clinical problem. An algorithm for each clinical presentation , will help to reach a “definite “ diagnosis ,with the least radiation exposure and cost . The referring physician ,as well as the pediatric Radiologist ,have the duty to take PROBLEM ORIENTED DECISIONS ,which will decide ,which techniques will be used or omitted in any given clinical situation ,so as to reach the appropriate diagnosis. I-Thorax CXR-showing a large mediastinal mass lesion . 1. Patient with a chest mass. The clinical problem : The discovery of a chest mass on CXR is a common finding which can happen in the course of investigation for a tachypneic child ,signs of SVC obstruction ,coughing ,chest infection ,or incidentally. The need for identifying a normal thymus is needed. The location of chest mass is necessary to build a working differential diagnosis. Role of Radiology: An approach includind CXR with chest US has been proposed by some authors . The technique depends on examining the chest through suprasternal ,parasternal and sub-xiphoid windows. The main role of U.S. is : 1. Identify a normal thymus.
- 2. 2. Differentiate between a cystic or solid mass lesions. 3. Study of the cystic lesion –which is most likely bening-regarding its size ,wall ,contents ,etc.. Etiology Anterior Mediastinum Middle Mediastinum Posterior Mediastinum Congenital Thymic cyst Foregut cyst Foregut cyst. Morgagni Hernia Hiatal hernia-achalasia Lateral meningocele Bochdaleck Hernia Inflammatory Mediastinitis. Mediastinitis. +spinal inflammatory Lymohadenopathy Lymphadenopathy diseases Neoplastic Lymphoma-Leukemia Lymphoma-Leukemia Neurogenic Germ Cell tumor. tumours(neural crest or Teratoma peripheral nerve Tumors ).lymphoma- Leukemia- Phaechromocytoma. Traumatic Haematoma Hematoma. Spinal fracture Thymic Hemorrhage Diaphragmatic rupture Vascular Annomalous vessel Aneurysm. Aortic aneurysm Great vessels anomaly Dilated azygous vein Miscelaneous Histiocytosis Pancreatic pseudocyst- Extramedullary Sarcoidosis Histiocytosis-sarcoidosis Haematopoiesis. 4. Evaluate the solid lesion regarding its site ,size ,borders ,presence or absence of necrosis ,vascularity ,etc.. 5. guide for interventional procedure (biopsy or aspiration for peripheral lesion Etiology: I-Mediastinal masses. II-Chest wall masses: -Normal structures at pleural surface Location Causes Soft tissue tumors Lymphangioma Cystic Hygroma Extrapleural – intrathoracic Mesenchymoma-Lipoma Rhabdomyosarcoma Bony thorax tumors Generalized bone diseases :Neurofibromatosis-Multiple hereditary exostosis, Benign causes:fibrous dysplasia-osteochondroma-eosinophilic granuloma- Aneurysmal bone cyst. Malignant:Ewing Sarcoma- PNET-chondrosarcoma-Osteosarcoma
- 3. Metastatic: Neuroblastoma-Leukemia III-Lung Masses : Location Causes Pleural Metastasis-Leukemia- Lymphoma-Askin tumor Primary: Parenchymal Benign:Bronchogenic cyst- Sequestration-Round pneumonia-hamartoma- bronchial adenoma. Malignant:Sarcoma- Pulmonary Blastoma Secondary: Benign:Papillomatosis Malignant:Wilm’s tumor,Osteosarcoma,etc. B-Flow of thinking : 5 questions to ask. 1.Location 2.Density 3.enhancement 4.Morphology 5. Associations (Wall/med/lung) (air/fat/calcification) ( border/size/shape) (displacement/bony Destruction)
- 4. 2. Patient with upper Airway Obstruction CXR:Church steeple sign denoting Croup A-Etiology : The differential diagnosis of upper air way obstruction depends upon :the age of presentation (neonatal ?older children),associated findings (fever/nasal obstruction/stridor),history of foreign body inhalation. Mechanism Causes Choanal atresia -micrognathia-ectopic thyroid-laryngomalacia-laryngeal ,subglottic tracheal Congenital stenosis-nasal encephalocele. Adenoids- retropharyngeal abscess-croup-epiglottitis- Inflammatory Laryngeal,aryepiglottic,retention,or epiglottic cysts-cystic hygroma-hemangioma-papilloma- Rhabdomyosarcoma-dermoid / teratoma-Nasopharyngeal mass(Angiofibroma) Masses Foreign body-hematoam-radiation-thrermal injury. Traumatic Tracheomalacia-vascular ring-angioneurotic edema Miscellaneous Role of Imaging: 1.Croup: Pathophysiology: The cells of the respiratory epithelium are infected following viral inhalation. Inflammation is diffuse in the involved airway. X-ray diagnosis: Frontal neck radiograph: The lateral walls of the subglottic larynx normally are convex or shouldered . Wall edema in croup narrows this space with loss of lateral convexity, creating a steeple shape below the vocal cords The narrowing may extend for 5-10 mm below the vocal cords. 2.Epiglottitis: Pathophysiology: Epiglottitis causes inflammation and swelling of the epiglottis, vallecula, arytenoids, and aryepiglottic folds. As the tissues swell, they protrude downward and over the glottic opening, making breathing difficult.
- 5. X-ray diagnosis: In epiglottitis, images show diffuse soft-tissue swelling with enlargement of the epiglottis and also of the normally thin aryepiglottic folds. One should look for an enlarged epiglottis (thumbprint sign), thickened aryepiglottic folds, and ballooning of the hypopharynx, usually with normal subglottic structures . CXR:Bilateral consolidation patches-Broncho-pneumonia 3. Patient with chest Infection A-Etiology : 1. Viral(Adeno virus-Haemophylis Influenza –Respiratory syncitial virus) 2. Bacterial (streptococcal-Staphylococcal-Klebsiella) 3. Fungal(aspergillosis) 4. Tuberculous. 5. Mycoplasma. 6. Amebic. B-Complications: 1. Empyema. 2. Pulmonary abscess. 3. Bronchopleural fistula. 4. Septic embolization.
- 6. Large pleural collection in left hemithorax –post staph pneumonia-Empyema. Ultrasonic examination revealing loculated pleural effusion. 4. Patient with recurrent/chronic pulmonary problems A-Etiology : Extensive list for the causes of chronic /recurrent lung infections are present. Mechanism Causes CNS malformation-cerebral tumors- 1. Aspiration Tracheo-esophageal fistula-Reflux Congenital lobar emphysema- 2.Anomaly Sequestration-Tracheobronchial tree anomalies(tracheal bronchus- stenosis-atresia)-bronchogenic cyst. Astham- Loeffler pneumonia-allergic 3.Allergy. alveolitis Cystic fibrosis 4.Systemic disease. Prematurity-AIDS-Neutropenia 5.Immunodeficiency. Foreign body-Drugs-radiation- 6.Physical agents. Bronchopulmonary dysplasia
- 7. Leukemia-Lymphoma-Histiocytosis 7.Neoplasm. Left to right shunt -PA stenosis- 8.CVS vascular ring TB-Mycoplasma-Bronchiectasis 9.specific Infections. Interstitial Pneumonia-Collagen 10.Miscellaneous vascular disease-Alveolar proteinosis-sarcoidosis. B-Role of Radiology : The role of radiology is 3 folds : 1 .Evaluate the present X-ray. Look for : The presence and distribution of opacities,Pleural involvement ,Lymph nodal swellings ,pulmonary vascularity ,soft tissue involvement , bony structures . 2.Review of previous films. Look for: Are the lesion stable in the same location (Sequestration ?) Are they present always in upper lobe (aspiration ? ) Are they changing in location (Immunodeficiency ?) 3.Perform esophagogram. Look for : 1. Reflux of gastric contents. 2. Abnormal peristalsis-Compression of esophagus by a mass ,vascular ring. 3. Tracheo-esophageal fistula. 4. Hiatal Hernia
- 8. Left basal pulmonary lesion with systemic aterial supply (2)..Pulmonary sequestration 5.Neonate with respiratory distress CXR :RDS –Bilateral Opacification with air bronchogram. Etiology: 1. Respiratory distress syndrome. 2. Congenital Diaphragmatic Hernia.
- 9. 3. Congenital Cystic Adenomatoid Malformation. 4. Congenital Lobar Emphysema. 5. Lung agenesis /hypoplasia. 6. Tracheal stenosis/atresia. 7. Pulmonary sling. 8. Vascular ring. Role of imaging 1.Congenital Cystic adenomatoid Malformation: Pathogenesis and pathophysiologic features: CAM is believed to result from focal arrest in fetal lung development before the seventh week of gestation secondary to a variety of pulmonary insults. Types: Type I lesions, the most common, are composed of 1 or more cysts measuring 2-10 cm in diameter. Type II lesions are characterized by small relatively uniform cysts resembling bronchioles Type III lesions consist of microscopic, adenomatoid cysts, and are grossly a solid mass without obvious cyst formation. Radiographic findings: The pattern in the lung demonstrates multiple radiolucent areas that vary greatly in size and shape. Cysts are separated from each other by strands of opaque pulmonary tissue. The involved lung may appear honeycombed or spongy, but occasionally, 1 large cyst may overshadow the others. Air trapping within cystic spaces can cause rapid enlargement of the CAM CT findings: Areas of small cysts (<2 cm in diameter) appearing with other abnormalities (a larger cystic area, consolidation, or low attenuation) are the most frequent findings. Multiple large cystic lesions (>2 cm in diameter) are seen alone or with other abnormalities (areas of small cysts, consolidation, or low attenuation). Low-attenuation areas are clusters of microcysts. Air-fluid levels can be seen in some cysts. These lesions may be predominantly type I, type II, or a combination of both.
- 10. MRI findings:In CAM, prenatal MRI findings on T2-weighted images have been reported. CAMs appear as intrapulmonary masses with increased signal intensity on T2-weighted images. Type III CAM lesions have moderately high signal intensity. Ultrasonic diagnosis: Partially cystic partially echogenic masses are characteristic of type I or type II lesions. The size or dimension of the cysts distinguishes the 2 types. Type III lesions may be large and entirely echogenic. Chest X-ray revealing multiple basal lung cysts (CCAM) CT chest :right basal cystic lesions-CCAM 2.Congenital lobar emphysema: Pathophysiology: Overdistension of the airspaces within a pulmonary lobe is associated with air trapping and compressive changes in the remainder of the lung . Mediastinal shift away from the increased volume results in compression of the contralateral lung. CLE almost always involves one lobe, with rates of occurrence as follows: Left upper lobe - 41% Right middle lobe - 34% Right upper lobe - 21% X-ray findings: A large, hyperlucent lung with attenuated but defined vascularity is observed. Compressed remaining lung on that side, flattened hemidiaphragm, and widened intercostal spaces also are seen. An involved lung is seen herniated across the anterior midline.On a lateral view, the heart is displaced posteriorly with retrosternal lucency representing an anteriorly herniated lobe .
- 11. CXR:large right basal cystic lesion. CT rvealed area of hyperlucency :Congental Lobar Emphysema CT findings: CT scan shows a hyperlucent, hyperexpanded lobe (attenuated but intact pattern of organized vascularity) with midline substernal lobar herniation and compression of the remaining lung. Usually, the mediastinum is significantly shifted away from the side of the abnormal lobe . 3.Respiratory distress syndrome : Pathophysiology: RDS is the result of anatomic pulmonary immaturity and a deficiency of surfactant. Pulmonary surfactant synthesis, in type II pneumocytes, begins at 24-28 weeks of gestation, and gradually increases until full gestation. Pulmonary surfactant decreases surface tension in the alveolus during expiration, allowing the alveolus to remain partly expanded, thereby maintaining a functional residual capacity. In premature infants, an absence of surfactant results in poor pulmonary compliance, atelectasis, decreased gas exchange, and severe hypoxia and acidosis. X-ray diagnosis: The radiologic spectrum of RDS ranges from mild to severe and is generally correlated with the severity of the clinical findings.In the early stages of the disease, notable air bronchograms are lacking because the major bronchi lie in the more anterior portions of the lungs and because alveolar atelectasis tends to involve the dependent areas of the lungs, which are posterior in recumbent infants. However, a bubble appearance, which represents overdistended bronchioles and alveolar ducts, can be observed. As RDS progresses, the reticulogranular pattern becomes prominent due to coalescence of the small atelectatic areas. This coalescence leads to larger areas of increased lung opacity. As the anterior portions of the lung become involved with microatelectasis, the granularity becomes uniformly distributed, and air bronchograms can be seen. With increasing severity of disease, progressive opacification of the anterior portions of the lungs cause obscuration of cardiac silhouette and the formation of prominent air bronchograms. With severe disease, the lungs appear opaque and display prominent air bronchograms, with total obscuration of cardiomediastinal silhouette.
- 12. CXR :respiratory distress syndrome Complications: 1.Pulmonary interstitial emphysema: PIE can be symmetrical, asymmetrical, or localized to 1 portion of a lung. Peripheral PIE can produce subpleural blebs and ultimately rupture into pleural space to produce pneumothorax (usually tension pneumothorax), or they can extend centrally to produce pneumomediastinum or pneumopericardium. Because infants are supine and because air rises to the highest point of the thorax, the pneumothorax is located paramediastinally, resulting in the sharp mediastinum sign, whereby the mediastinum/heart is sharply outlined by adjacent free air rather than aerated lung tissue. CXR :Pulmonary interstitial emphysema 2.Bronchopulmonary dysplasia: After days of ventilatory support, interstitial fibrosis results from the cumulative effect of therapeutic insult to the pulmonary parenchyma. This fibrosis is often accompanied by exudative necrosis and a honeycomb appearance of the lungs on chest radiography. The honeycomb appearance represents focally distended alveolar groups in a scarred, and immature lungs.
- 13. CT chest : ARDS in NICU patient with difficult extubation II –Body 1. Vomiting Digestive origin Extra digestive origin Frequent Rare Infectious Otitis media - Labyrinthitis-Pneumonia-UTI Congenital Microgastria Neurological Cerebral hypertophic Pyloric tumors,hydrocephalus,Abscess,hematoma stenosis Antral Dyskinesia Antral Diaphragm Toxic Lead poisoning-Chemotherapy-Vitamin A&D poisoning Intussusception. Midgut volvulus Metabolic Fructosemia-Galactosemia-Tyrosinemia- Adrenal insufficiency Hirschprung disease Preduodenal portal Psychic Anorexia vein Gastroenteritis Ladd’s Band Acute Appendicitis Gastric or duodenal Ulcer 1.Congenital Hypertrophic Pyloric stenosis: Pathophysiology: Full-thickness biopsies demonstrate both hypertrophy and hyperplasia of the circular muscle layer of the pylorus. Sex: Male-to-female ratio is 4-6:1. Age: HPS most commonly is seen in infants aged 3-6 weeks Imaging: 1. Ultrasonic diagnosis ; US examination showing CHPS: note thich muscular layer and elongated canal
- 14. Target sign on transverse images of the pylorus Muscle thickness of >3mm Pyloric channel length greater than 17 mm Pyloric thickness (serosa to serosa) of 15 mm or greater Failure of the channel to open during a minimum of 15 minutes of scanning Retrograde or hyperperistaltic contractions Antral nipple sign, a prolapse of redundant mucosa into the antrum (creating a pseudomass) 2.Intussusception: Role of imaging : Abdominal radiograph: Look for dilated small bowel and absence of gas in the region of the cecum . Occasionally, a mass impression within the colonic gas indicates an intraluminal mass created by the intussuscepting loop. Abdominal radiograph :intususception transverse colon Ultrasound Transverse: Ultrasound (US) shows a mass with a swirled appearance of alternating sonolucent and hyperechoic bowel wall of the loop-within-a-loop. Longitudinal: US of the mass shows a submarine sandwich-like appearance of the intussuscipiens and the intussusceptum. There appear to be multiple layers, which represent the walls of the intussuscepted bowel loops .
- 15. Ultrasonic examination showing Donut sign of intususception 3.Mid gut Volvulus: Malrotation is caused by incomplete rotation (<270° of counterclockwise rotation occurring in weeks 5-12). This group of disorders can be divided into different categories: Nonrotation (0° to <90° of counterclockwise rotation occurring before 6 weeks) Reverse rotation (abnormal rotation >90° and <180° causing obstruction or reversal of the normal duodenal/SMA relationship, occurring in weeks 6-10) Malrotation most often associated with malfixation (>180° and <270° of counterclockwise rotation, occurring after 10 weeks) Clinical Details: Malrotation with midgut volvulus classically presents in the neonate with bilious vomiting and high intestinal obstruction.. Older children with malrotation may show failure to thrive, chronic recurrent abdominal pain, malabsorption, or other vague presentations. Radiological diagnosis: 1.UGI studies: Findings of a UGI series in malrotation include the following: DJJ displaced downward and to the right on the frontal view An abnormal course of the duodenum on lateral view An abnormal position of the jejunum (lying on right side of abdomen) . In malrotation with midgut volvulus, findings also include the following: A dilated, fluid-filled duodenum A proximal small bowel obstruction A "corkscrew" pattern (proximal jejunum spiraling downward in right or mid upper abdomen in midgut volvulus. Mural edema, thick folds
- 16. UGI Typical corkscrew appearance of midgut volvulus 2. Ulrasound: The "whirlpool sign" on color Doppler shows mesentery and flow within the SMV wrapping around the SMA (in a clockwise direction), indicating malrotation with volvulus. A dilated, fluid-filled duodenum frequently is seen in patients with obstruction without volvulus. However sensitivity and specificity are low compared to the UGI series; therefore, a UGI examination is mandatory to confirm the diagnosis whirlpool sign" on color Doppler . 2- Abdominal mass Etiology: Abdominal or pelvic masses are comon paediatric clinical problems. The radiologist must be aware of the clinical presentation of the patient as well as his age. The radiological examination depend mainly on: 1. Abdominal X-ray without preparation. 2. Ultrasonography. Orientations: 1. Topographic localization .
- 17. 2. Structural orientaion. 3. Associated lesions. Abdominal Lesions : I-Intraperitoneal Lesions : Causes before 6 months : Haemangioendothelioma- Pepper Syndrome Causes at any age : 1. Hepatic masses :hepatoblastoma. 2. Splenic masses :cysts 3. Cystic masses: 4. Ovarian masses. 5. Lymphomatous masses II-Retroperitoneal Lesions : Pillars of diagnosis : 1. Age. 2. structure (ultrasonic and CT) 3. Renal or adrenal origin. Causes : A-Renal : Unilateral : Wilm’s tumour ,mesoblastic nehroma,Multiloclar cystic nephroma. Bilateral : Angiomyolipoma,nephroblastomatosis,lymphoma ,metastasis. B-Adrenal:neurblastoma. C-Lymphadenopahties : Pelvic lesions I-Neonatal period : Girls :Ovarian cyst-Hydrometrocolpos. Boys :PUV causing bladder distension. Any sex:Teratoma-Meningoceles-pelvic neuroblastoma. II-Post neonatal period: 1. Ovarian cyst. 2. Rhabdomyosarcoma. 3. Urinary bladder diverticulum. 4. Pelvic Abscess.
- 18. 5. Bony tumours. 6. Nodal swellings. 1.Neuroblastoma: Pathophysiology: Neuroblastomas arise from primitive neural crest cells that differentiate to form the sympathetic nervous system. Imaging: Ultrasound: Ultrasonography can be used as a screening tool for detecting abdominal or pelvic masses in children Neuroblastomas appear as an inhomogeneously echogenic mass on sonograms. Calcifications typically appear as focal brightly echogenic areas in the mass CT findings: CT is the modality most commonly used to diagnose and stage neuroblastomas. CT can show the organ of origin, extent of the tumor, lymphadenopathy, metastases, and calcifications. About 80-90% of neuroblastomas show stippled calcifications on CT. Neuroblastomas often encase or compress adjacent blood vessels. Neuroblastomas rarely invade into the lumen of blood vessels. The tumors often appear lobulated and typically have a heterogeneous appearance on contrast-enhanced CT. There are areas of low attenuation in the mass secondary to necrosis and hemorrhage. CT is good for detecting lung metastases and focal liver metastases (which appear as focal hypoattenuating and poorly enhancing masses). Bone-window settings should always also be examined to assess for skeletal metastases. MRI findings: Neuroblastomas are typically hypointense on T1-weighted images and hyperintense on T2-weighted images. When contrast material is administered, the tumor exhibits inhomogeneous enhancement. Calcifications appear as signal voids on MRIs. Hemorrhagic areas often appear bright on T1-weighted images. Bone-marrow disease appears bright (hyperintense) and heterogeneous on T2-weighted images and dark (hypointense) on T1-weighted images. Diffuse liver metastases appear bright on T2-weighted MRIs. Nuclear medicine: Iodine-131 metaiodobenzylguanidine (MIBG) and iodine-123 MIBG are used to identify sites of primary neuroblastomas. Tumors that contain sympathetic tissue, such as neuroblastomas, ganglioneuroblastomas, ganglioneuromas, medullary thyroid carcinomas, pheochromocytomas, and carcinoids, take up MIBG. Another isotope that can be used in detecting primary neuroblastomas is indium-111 pentetreotide, which is a somatostatin analog.
- 19. Axial T2-weighted MRI demonstrates extradural extension into the spinal canal. 3-Patient with Urinary Tract Infection Definition : Pure growth of > 100 000 organism/ml urine Etiology: 1. Vesicoureteric reflux. 2. Obstructive uropathy. 3. Reflux nephropathy and scar formation. 4-Neonate with Abdominal wall defects Etiology : 1. Omphalocele. 2. Gastroschisis. 3. Cloacal exstrophy (Omphalocele-Exstrophy of urinary bladder-Imperforate anus- meningeomyelocele ) 4. Pentalogy of Cantrell :Omphalocle-Ectopic heart-Bifid sternum-Anterior diaphragmatic hernia- Pericardial defect ) 1.Gastroschisis: Pathophysiology: Controversy exists regarding the cause of gastroschisis. Some authorities suggest that the defect is caused by abnormal involution of the right umbilical vein, resulting in rupture of the anterior abdominal wall at a point of weakness. Others suggest that gastroschisis results from rupture of an exomphalos. Another theory for etiology of gastroschisis is premature interruption of the right omphalomesenteric artery, which results in ischemic injury to the anterior abdominal wall through which herniation of abdominal contents occurs.
- 20. Effects: Because the herniated bowel is bathed by amniotic fluid, both maternal serum and amniotic fluid AFP levels are elevated, more so than in exomphalos. Later in pregnancy, bowel obstruction, peritonitis, bowel perforation, and fetal growth restriction may occur secondary to nutrient loss through exposed bowel. Ultrasound findings: Findings include exteriorized bowel in relation to the anterior abdominal wall, multiple loops of bowel, and a thickened bowel floating freely in the amniotic fluid. The bowel can be identified by its characteristic sonographic pattern. Because no covering is present around the bowel loops; the bowel loops of a gastroschisis result in a mass with irregular edges. Usually, the small and large bowels are herniated, but, occasionally, the stomach, liver, gallbladder, spleen, uterus, adnexa, and urinary bladder may be herniated. Signs of intestinal obstruction may be depicted; examples of these include multiple distended loops of bowel (both intraperitoneal and extraperitoneal), bowel loops greater than 17 mm in diameter, and increased peristalsis. Polyhydramnios may ensue in high intestinal obstructions. A bowel diameter of greater than 17 mm usually represents significant bowel dilation, and diameters greater than 11 mm are usually associated with a greater number of postnatal bowel complications. A right paramedian paraumbilical abdominal wall defect is revealed, usually of 2-5 cm.Insertion of the umbilical cord is normal. Typically, no ascites is noted. Bowel perforation can cause calcification and an intramesenteric extra-abdominal pseudocyst 2.Omphalocele: Pathophysiology: Various theories have been postulated; these include failure of the bowel to return into the abdomen by 10-12 weeks, failure of lateral mesodermal body folds to migrate centrally, and persistence of the body stalk beyond 12 weeks' gestation. Associated anomalies are common (45-88%). Chromosomal anomalies (40-60%): These include trisomies 18,13, and 21 Cardiac defects (16-47%): These include ventricular and atrial septal defects, tetralogy of Fallot, pulmonary artery stenosis, coarctation of the aorta, Genitourinary anomalies (40%): These include bladder extrophy and omphalocele, bladder extrophy, imperforate anus and spinal anomalies . Neural tube and head and neck anomalies: These include neural tube defects, holoprosencephaly, encephalocele, Gastrointestinal anomalies (40%): These include diaphragmatic hernia, malrotation, intestinal duplications, atresias, and ascites, Musculoskeletal anomalies (10-30%): This includes scoliosis, hemivertebra, and camptomelic dwarfism,.
- 21. Maternal/fetal developmental abnormalities: These include oligohydramnios, polyhydramnios, intrauterine growth restriction (IUGR), Beckwith-Wiedemann syndrome (5-10%) Ultrasound findings :An omphalocele is diagnosed when a fetal anterior midline abdominal mass is demonstrated. The mass consists of abdominal contents that have herniated through a midline central defect at the base of umbilical cord insertion. The mean size of the defect is 2.5-5 cm. The mass has a smooth surface and contains abdominal viscera, usually the liver and including the bowel and stomach. The membrane is not always visible. Wharton jelly may be detectable as a hypoechoic lining between the layers of the covering of the membrane. The umbilical cord attaches to the apex of the herniated mass.Fetal ascites is common and seen within the herniated sac. Polyhydramnios, and occasionally oligohydramnios, may be present. 3.Prune Belly Syndrome: The child with prune belly syndrome typically is male with a thin or lax abdominal wall and a long and dilated prostatic urethra from prostatic hypoplasia. A large, vertically oriented, thick-walled bladder; a urachal remnant from the dome of the bladder; and tortuous and dilated ureters. Varying amounts of hydronephrosis and varying degrees of renal dysplasia are seen. All have cryptorchidism. Radiographic & ultrasonic findings: Chest: Hypoplastic lungs, flared lower ribs secondary to the distended abdomen are seen. Abdomen: Diffusely distended flanks are seen. Kidneys: Sonography of the kidneys shows diffusely hyperechoic parenchyma, small parenchymal cysts, clubbed dysplastic calyces, and markedly tortuous ureters, which is sufficient to make the diagnosis. The increased echogenicity of the parenchyma is an indicator of underlying dysplasia of the renal tissue during early differentiation and maturation. The bladder is usually large and thick-walled. Ureters: Ureters are markedly dilated and tortuous Bladder: The bladder is vertical and trabeculated, with a urachal remnant at the dome. Urethra: A wide and long posterior urethra is seen with a utricular remnant. Cryptorchidism: The testes are in the abdomen or inguinal canals.
- 22. 5-Neonate with Intestinal Obstruction Etiology: 1. Duodenal Obstruction(atresia,stenosis,web) 2. Jejunal/ileal atresia. 3. Malrotation and mid gut volvulus. 4. Meconium Ileus. 5. Meconium Plug (Small left colon ) 6. Hirschprung disease. 7. Anorectal malformation. I-Hirschsprung Disease : Pathophysiology: The congenital absence of ganglion cells in the distal alimentary tract is the pathologic sine qua non of HD. The aganglionosis present in HD results from a failure of cells derived from the neural crest to populate the embryonic colon during development. This failure results from a fundamental defect in the microenvironment of the bowel wall that prevents ingrowth of neuroblasts. So far, 8 genetic defects are known to be associated with HD, including mutations to the endothelin-B receptor gene and the RET proto- oncogene. Because of the polygenic nature of HD, the penetrance of the condition is variable; it leads to the variable manifestations of the disease. Anatomy: HD is regarded as a neurocristopathy because it involves a premature arrest of the craniocaudal migration of vagal neural crest cells in the hindgut at weeks 5-12 of gestation to form the enteric nervous system. As a consequence, both intramural ganglion cells in the Meissner (submucosal) and Auerbach (myenteric) plexuses are absent. The anus is always involved, and a variable length of distal intestine may be involved as well. The aganglionic, aperistaltic bowel segment effectively prevents the propulsion of the fecal stream, resulting in dilation and hypertrophy of the normal proximal colon. HD can be classified by the extension of the aganglionosis as follows: • Classical HD (75% of cases): The aganglionic segment does not extend beyond the upper sigmoid. • Long segment HD (20% of cases) • Total colonic aganglionosis (3-12% of cases) Some rare variants include the following: • Total intestinal aganglionosis
- 23. • Ultra-short-segment HD (involving the distal rectum below the pelvic floor and the anus. Clinical Details: Newborns with HD come to medical attention with the following symptoms: • Failure to pass meconium within the first 48 hours of life • Abdominal distension that is relieved by rectal stimulation or enemas • Vomiting • Neonatal enterocolitis Symptoms in older children and adults include the following: • Severe constipation • Abdominal distension • Bilious vomiting • Failure to thrive Children presenting with abdominal distension, explosive diarrhea, vomiting, fever, lethargy, rectal bleeding, or shock may possibly have HAEC. The risk for HAEC is greatest before HD is diagnosed or after the definitive pull-through operation. Also, children with Down syndrome have an increased risk for HAEC. X-ray findings: Radiographs of the neonatal abdomen may show multiple loops of dilated small bowel with air-fluid levels that can usually be determined to be a distal bowel obstruction. An empty rectum is a common finding. A cutoff sign in the rectosigmoid region, with an absence of air distally, is a useful finding in HAEC. HD is more definitively diagnosed by means of contrast enema examination, which can show the presence of a transition zone, irregular contractions, mucosal irregularity, delayed evacuation of contrast material, and other findings. The transition zone is the term applied to the region in which a marked change in caliber occurs, with the dilated normal colon above and the narrowed aganglionic colon below. This sign is highly reliable of HD, but a failure to visualize this sign does not rule out HD. The hallmark of the diagnosis is demonstration of the transition zone from the dilated bowel to the reduced- caliber bowel. Obviously, finding more than 1 sign increases the accuracy in diagnosis. Signs of HD after barium enema administration include the following: • Transition zone (often subtle during first week of life) • Abnormal, irregular contractions of aganglionic segment (rare) • Thickening and nodularity of colonic mucosa proximal to transition zone (rare) • Delayed evacuation of barium • Mixed barium-stool pattern on delayed radiographs • Distended bowel loops on plain radiographs that almost fill after contrast enema • Question mark–shaped colon in total colonic aganglionosis Ultrasonic Findings: Although sonography is not the first imaging tool for diagnosing HD, diagnosis is possible with real-time ultrasonography. Oestreich reported a case of unsuspected HD in a 1-month-old baby who went to the pediatrician for a check-up. A distended abdomen was noted. Sonography revealed the same pattern that is observed in the barium enema examination, that is, a dilated sigmoid narrowing to a narrow rectum. Sonography may also help in determining the dynamic or adynamic state of fluid-filled or solid-filled bowel loops.
- 24. Hirschsprung disease. Frontal abdominal radiograph showing marked dilatation of the small bowel with no gas in the rectum. Hirschsprung disease. Lateral view from a barium enema examination depicting the reduced diameter of the rectum and sigmoid.
- 25. Hirschsprung disease. A 24-hour-delayed radiograph obtained after a barium enema examination shows retention of barium and stool in the rectum. This is associated with a dilated stool-filled sigmoid. II-Meconium Plug Syndrome: Background: Meconium plug syndrome, also termed functional immaturity of the colon, is a transient disorder of the newborn colon characterized by delayed passage (>24-48 h) of meconium and intestinal dilatation. Contrast enema demonstrates the retained meconium as a filling defect or plug. that produces a double-contrast effect. Small left colon syndrome is a subset of meconium plug syndrome in which an enema demonstrates an apparent transition zone between the dilated and the normal-to-decreased caliber distal colon at the splenic flexure Pathophysiology: Early descriptions of meconium plug syndrome emphasized the contrast-enema appearance and ascribed a possible etiologic role to the retained meconium, which is often dislodged after the enema study. Currently, meconium plug syndrome is understood as a transient functional disorder of the colon resulting from immaturity of the myenteric plexus nerve cells or their hormonal receptors. This distinguishes it from Hirschsprung disease, which may have identical clinical and radiographic findings in which nerve cells are absent in the distal diseased portion of the colon. Anatomy: Anatomic changes in meconium plug syndrome vary. Usually, the colon is normal or may be mildly enlarged and filled with meconium. A change in the colon's diameter at the splenic flexure may be seen and is indistinguishable from that observed in Hirschsprung disease, although in the latter disorder the transition zone usually is in the rectosigmoid. In preterm infants weighing less than 1000 g, the entire colon may be small, producing an enema appearance similar to ileal atresia or meconium ileus. Clinical Details: Clinically, the hallmarks of the disorder are abdominal distention and failure to pass significant meconium in the first 24 hours of life. Bilious vomiting may occur. Symptoms often are present before the first feeding, which helps distinguish the disorder clinically from necrotizing enterocolitis. The incidence is increased in premature infants of diabetic mothers (especially the small left colon variant) and in infants whose mothers received magnesium sulfate for treatment of toxemia. Newborns with cystic
- 26. fibrosis also may present with meconium plug syndrome, although meconium ileus is more frequent and characteristic in these patients. Despite these associations, many patients have no apparent risk factor. Radipgraphic Findings: Plain films usually demonstrate multiple dilated loops of bowel with absence of rectal gas. The presence or absence of air-fluid levels in the bowel is not helpful. Findings are similar to those of structural colonic or distal small bowel obstruction and help to exclude malrotation with volvulus or obstructing Ladd bands, in which the blockage usually occurs at the duodenum. Contrast enema usually shows a moderately dilated colon filled with radiolucent material (the meconium plug). In the small left colon variant, a transition is seen from a relatively small to normal or increased caliber bowel in the region of the splenic flexure. lateral view from contrast enema in a newborn demonstrates a normal-to-decreased caliber "empty" distal colon and dilated proximal bowel containing multiple plugs. The child responded clinically and radiographically to a single enema III-Necrotizing Enterocolitis : Background: Necrotizing enterocolitis (NEC) is a serious gastrointestinal disease of unknown etiology in neonates. NEC is characterized by mucosal or transmucosal necrosis of part of the intestine. The very small, ill, infant who is born before term is most susceptible to NEC, and the incidence is increasing because of the improved survival rate in the high-risk group of infants born prematurely. Pathophysiology: Several factors contribute to the development of neonatal NEC. The underlying pathology is the accumulation of gas in the submucosal layers of the bowel wall, which progresses to necrosis. Outcomes include eventual necrosis of the bowel loops; perforation; systemic sepsis; and, sometimes, death. The regions of bowel most often affected are the right side of the colon and the distal ileum, although any portion of the bowel is susceptible. The major or most common contributor to NEC is sepsis; however, indwelling vascular catheters, assisted ventilation, respiratory acidosis, and hypoxemia all are contributing factors as well. NEC is primarily a complication of prematurity with possible hypoxemia, acidosis, hypotension, sepsis, and stress. The abnormality also occurs in ill full-term neonates, particularly those with a history of sepsis, hypoxia, asphyxia, or difficult resuscitation. Polycythemia, the use of hypertonic formulas or medicines, and a too-rapid establishment of feeding may cause mucosal injury. Epidemics of NEC are documented, and identified infectious agents include Clostridium perfringens, Escherichia coli, Staphylococcus epidermidis, and rotavirus.
- 27. Clinical Details: Onset occurs 2 weeks to several months after birth. Meconium is usually passed normally, and the initial signs of NEC include abdominal distention and gastric retention of fluid. Manifestations of the disease develop after enteric feedings begin. Obviously bloody stool is observed in approximately 25% of patients. The onset of NEC can be insidious, and sepsis may occur before an intestinal abnormality is noted. The spectrum of presentations ranges from mild forms, with guaiac-positive stool, to severe forms, with peritonitis, bowel perforation, shock, and death. Progression may be rapid; progression of the disease after 72 hours is usual. Pneumatosis is a late finding in NEC and usually indicates some necrosis of the bowel wall. The presence of irritability, distention, and bowel distention, especially when associated with bloody stool, is diagnostic of NEC. Radiographic Findings: A high index of suspicion is essential in the diagnosis of NEC. Abdominal radiographs may demonstrate multiple dilated loops of bowel that change little in their location and appearance with sequential studies. Pneumatosis intestinalis, or gas in the wall of bowel in a linear or bubbly pattern, is present in 50-75% of patients. Portal venous gas and gallbladder gas indicate serious disease. Pneumoperitoneum indicates a perforation. CT or water-soluble enema examination may be used to demonstrate pneumatosis or a site of perforation. Radiograph demonstrates multiple dilated loops in the large bowel and small bowel. Note pneumatosis intestinalis with bubbly and linear gas collections in the bowel wall. Anteroposterior image shows necrotizing enterocolitis with pneumatosis intestinalis.
- 28. Image shows free air secondary to bowel wall necrosis. Portal venous air is present in a patient with pneumatosis intestinalis. IV-Duodenal Atresia : Background: Duodenal atresia represents complete obliteration of the duodenal lumen. The duodenal diaphragm or web is thought to represent a mild form of atresia. Duodenal stenosis (incomplete obstruction of the duodenal lumen) is discussed with duodenal atresia because they represent a spectrum of similar intrauterine events. Annular pancreas occurs when pancreatic tissue surrounds the second portion of the duodenum. If the encirclement is complete, it may be associated with complete or incomplete duodenal obstruction. Since duodenal atresia or stenosis occurs in all cases of annular pancreas, consider the anomalous pancreas a secondary change rather than a primary cause of duodenal obstruction. Pathophysiology: The etiology of duodenal atresia and stenosis is unknown. Failure of recanalization of the duodenal lumen remains the favored theory compared with intrauterine vascular ischemia.
- 29. During the third week of embryonic development, the second portion of the duodenum at the junction of the foregut and midgut forms biliary and pancreatic buds derived of endoderm. During the next 4 weeks, these buds differentiate into the hepatobiliary system, with the development and subsequent fusion of the 2 pancreatic anlagen. Concurrently, the epithelium of the duodenum undergoes active proliferation, which, at times, completely obliterates the duodenal lumen. Vacuolization, followed by recanalization, reestablishes the hollow viscus. The second part of the duodenum is the last to recanalize. The early-forming biliary system consists of 2 channels arising from the embryonic duodenum. This structure creates a narrow segment of bowel, approximately 0.125 mm in length, that is interposed between the 2 biliary channels. This narrow region is the area most prone to problems, with recanalization and atresia formation. The ampulla of Vater usually is immediately adjacent to or traverses the medial wall of the diaphragm. The presence of a bifid biliary system, or the insertion of one duct above and one duct below the atresia, is rare and occurs when both biliary duct anlagen remain patent. The presence of bile above and below the atresia indicates a bifid biliary system. Clinical Details: Bile-stained vomitus in neonates aged 24 hours or younger is the typical presentation of atresia or severe stenosis. Minimal duodenal obstruction in mild stenosis or membrane may have few symptoms. In a few cases, the atresia is proximal to the ampulla of Vater and the vomitus is free of bile. Both duodenal anomalies can be associated with other GI and biliary tract abnormalities (malrotation, esophageal atresia, ectopic anus, annular pancreas, gallbladder or biliary atresia, vertebral anomalies). In addition, duodenal atresia can be associated with a duodenal diaphragm as well as congenital abnormalities in other systems. Examples include vertebral defects, anal atresia, tracheoesophageal fistula with esophageal atresia, and radial and renal anomalies (VATER) association and vertebral, anal, cardiac, tracheal, esophageal, renal, and limb (VACTERL) association. Anomalies of the kidneys can occur in VATER association. These are usually aplasia, dysplasia, hydronephrosis, ectopia, persistent urachus, vesicoureteral reflux, ureteropelvic obstruction, and other conditions. Radiographic Findings: The double-bubble sign represents dilatation of the stomach and duodenum. This configuration most commonly occurs with duodenal atresia and an annular pancreas. An annular pancreas is almost always associated with duodenal atresia. In a few cases of duodenal atresia, air can be observed distal to the area of obstruction. The anomalous hepatopancreatic ducts permit movement of air through a Y-shaped ductal system, with one limb proximal to the obstruction and one limb distal to the atresia. When duodenal atresia is combined with esophageal atresia, no air is observed in the stomach, and because the stomach is obstructed at both ends, the infant presents with a large, opaque upper midabdominal mass. If esophageal atresia is present with a distal fistula, air is present in the stomach and duodenum. Duodenal obstruction in the neonate may be partial or complete and secondary to intrinsic or extrinsic abnormalities. The duodenal bulb may be larger in duodenal atresia than in obstructions of the duodenum. Increased intramural pressure in duodenal obstruction can result in gastric pneumatosis.
- 30. Anteroposterior radiograph of abdomen depicts the double-bubble sign in duodenal atresia. 6-Patient with Jaundice Etiology: 1. Biliary atresia. 2. Caroli disease. 3. Choledochal cyst. 4. Cholecdochocele. 5. Cholelithiasis. 6. Diffuse hepatic parenchymal disease :Hepatitis-Fatty infiltration-Cirrhosis. 7. Hepatic Masses. 8. Hepatic veno-occlusive disease. I-Caroli Disease : Background: Caroli disease is a nonobstructive dilatation of the intrahepatic bile ducts. This is a rare congenital disorder that classically causes saccular ductal dilatation, which usually is segmental. Caroli disease is associated with recurrent bacterial cholangitis and stone formation. Caroli disease also is known as communicating cavernous ectasia or congenital cystic dilatation of the intrahepatic biliary tree. It is distinct from other diseases that cause ductal dilatation caused by obstruction. It is not one of the many choledochal cyst derivatives. Pathophysiology: Caroli disease involves congenital cystic dilatation of the intrahepatic biliary radicles of the liver. It is believed to have an autosomal-recessive inheritance pattern. It may be associated with autosomal-recessive polycystic kidney disease. The likely mechanism involves an in utero event that arrests ductal plate remodeling at the level of the larger intrahepatic bile ducts. Insufficient resorption of the ductal
- 31. plates leads to the formation of multiple primitive bile ducts surrounding the central portal vein. These enlarge, dilate, and become ectatic. This effect may be segmental. Two forms of Caroli disease exist: a simple or classic type and a second type that is associated with congenital hepatic fibrosis. Drawing shows the main right hepatic duct and the multiple segmental branch dilatations related to Caroli disease. Note the saccular dilatations that can occur, involving the right lobe of liver in this case. Clinical Details: Dr J Caroli of France first described this hereditary (congenital) disease in 1958. Signs and symptoms Patients may have bilirubinemia and abdominal pain. They generally are febrile. Other complaints, such as nausea and vomiting, may be nonspecific. Liver function test results may be abnormal and include elevated alkaline phosphatase levels. On examination, patients may have hepatomegaly, especially if they have hepatic fibrosis. Portal hypertension related to this may cause variceal bleeding. Elevation in white blood cell counts and positive blood culture results suggest sepsis and cholangitis. Patients may have long symptom- free periods. Malignancy occurs in approximately 7% of patients. Other etiologies for these symptoms should be excluded. The differential diagnosis can include sclerosing cholangitis, oriental cholangitis, choledochal cyst, and hydatid disease. Complications The complications of Caroli disease, especially recurrent bouts of cholangitis, may be present first. Intrahepatic calculi and abscesses are common. Stone passage can cause pancreatitis. CT Findings: Dilated segmental intrahepatic biliary radicles are present without involvement of the extrahepatic biliary tree. Preinfused scans may show hyper-attenuating sludge and stones or debris. Hypo-attenuating, tubular branching structures are identified; these communicate and extend from the porta hepatis toward the periphery. CT scan with IV contrast enhancement can show tiny dots, representing intraluminal portal veins, within the dilated intrahepatic bile ducts. This is termed the central dot sign. Take 3D images with or without the CT cholangiographic technique to help prove the relationship of the dilated structure to the ductal system, although this is better accomplished with MRCP (see below). CT can help depict abscesses and guide percutaneous drainage.
- 32. CT Complications such as cholangitis, choledocholithiasis, or cholangiocarcinoma may be present and can be identified with CT imaging. Portal hypertension can be present and result in hepatosplenomegaly with varices. Contrast-enhanced images obtained through the kidneys can show associated multiple renal cysts. MRI Findings: Dilated segmental intrahepatic biliary radicles can be identified with MRI, as with CT and ultrasonography. MRCP reveals similar findings and allows better review of the results, especially with a computer workstation. This noninvasive 3D technique is a good alternative to ERCP or direct cholangiography. This can confidently show the communication of the multiple cysts, which is mandatory for the differential diagnosis with cystic disease of the liver and multiple abscesses. Complications of Caroli disease also can be identified with MRI. Ultrasonic Findings: Ultrasonography is very helpful. It is the examination of choice. Dilated segmental intrahepatic biliary radicles are easily detected. No obstruction is present. The cystlike tubular anechoic spaces converge toward the porta hepatis. They are largest in the superior part of the liver. The intraluminal portal vein sign is related to the protrusion of the portal vein branches into the cyst wall. Color flow Doppler ultrasonography is helpful in showing blood flow in these branches but no flow is present in the bile- containing spaces. Portal branches bridge the cyst walls. Ultrasonography can also help in the diagnosis of complications and in the follow-up of patients with Caroli disease. Intraductal calculi are echogenic with acoustic shadowing. Ultrasonography-guided needle aspiration of bile from the cystlike lesions may be beneficial in the diagnosis of cholangitis and in confirming that the cysts communicate with the biliary tree. Congenital hepatic fibrosis is associated with Caroli disease and may be diagnosed with sonograms that show abnormal liver echogenicity. Ultrasonography-guided core biopsy may be performed, if necessary, to obtain liver samples for histologic evaluation to confirm this condition. In addition, polycystic renal disease, which is associated with Caroli disease, can be confirmed with sonography. Degree of Confidence: This is an excellent tool. A positive result has good predictive value and permits diagnosis with a high level of confidence. Caroli disease is the only condition in which dilated ducts surround the portal radicles; this finding at ultrasonography may obviate other invasive diagnostic techniques. 99mTc Isoyopic Findings: Hepatobiliary scintigraphy with technetium 99m iminodiacetic acid ( IDA) agents reveals large, irregular, multifocal collections of the radiotracer in the liver. A beaded appearance in the dilated ducts, if present, is somewhat pathognomonic. These collections correspond to the segmental dilatations, and no extrahepatic obstruction is present, although bile stasis and stone formation may result in atypical obstruction. On early images, if the ducts are dilated enough, they appear as photopenic branching areas within the liver. Single photon emission computed tomography (SPECT) may better outline the ductal pattern but it is most helpful in the evaluation of focal disease.
- 33. II-Choledochal Cyst : Background: Choledochal cysts are congenital anomalies of the bile ducts. They consist of cystic dilatations of the extrahepatic biliary tree, intrahepatic biliary radicles, or both. The first anatomic study of a choledochal cyst in the Western literature was published by Vater and Ezler in 1723. Douglas is credited with the first clinical report in a 17-year-old girl who presented with intermittent abdominal pain, jaundice, fever, and a palpable abdominal mass. Alonso-Lej et al provided the first systematic description of choledochal cysts in 1959 based on the clinical and anatomic findings in 96 cases. The resultant system classified choledochal cysts into 3 types and outlined therapeutic strategies for each. The classification system for choledochal cysts was further refined by Todani et al and currently includes 5 major types (Todani, 1977). Pathophysiology: The pathogenesis of choledochal cysts is most likely multifactorial. Some aspects of the disease are consistent with a congenital etiology, others with a congenital predisposition to acquiring the disease under the right conditions. The vast majority of patients with choledochal cysts have an anomalous junction of the common bile duct with the pancreatic duct (anomalous pancreatobiliary junction [APBJ]). An APBJ is characterized when the pancreatic duct enters the common bile duct 1 cm or more proximal to where the common bile duct reaches the ampulla of Vater. Anatomy: The following discussion of the pertinent anatomy of choledochal cysts is based on the Todani classification published in 1977. • Type I choledochal cysts are most common and represent 80-90% of the lesions. Type I cysts are dilatations of the entire common hepatic and common bile ducts or segments of each. They can be saccular or fusiform in configuration. Type I cysts can be divided into 3 subclassifications, including type IA cysts, which are typically saccular and involve the entire extrahepatic bile duct (common hepatic duct plus common bile duct) or the major portion of the duct. • Type II choledochal cysts are relatively isolated protrusions or diverticula that project from the common bile duct wall. They may be sessile or may be connected to the common bile duct by a narrow stalk. • Type III choledochal cysts are found in the intraduodenal portion of the common bile duct. Another term used for these cysts is choledochocele. • Type IVA cysts are characterized by multiple dilatations of the intrahepatic and extrahepatic biliary tree. Most frequently, a large solitary cyst of the extrahepatic duct is accompanied by multiple cysts of the intrahepatic ducts. Type IVB choledochal cysts consist of multiple dilatations that involve only the extrahepatic bile duct. • Type V choledochal cysts are defined by dilatation of the intrahepatic biliary radicles. Often, numerous cysts are present with interposed strictures that predispose the patient to intrahepatic stone formation, obstruction, and cholangitis. The cysts are typically found in both hepatic lobes. Occasionally, unilobar disease is found and most frequently involves the left lobe. Clinical Details: Some patients do not present until adulthood. In many adult patients, subclinical bile duct inflammation and biliary stasis have been ongoing for years. Adults with choledochal cysts can present with hepatic abscesses, cirrhosis, recurrent pancreatitis, cholelithiasis, and portal hypertension. The clinical history and presentation of a patient with a choledochal cyst varies with the patient's age. Overt dramatic signs and symptoms are more common in infancy, whereas manifestations are more subtle and protean in adulthood. Infants frequently come to clinical attention with jaundice and the passage of acholic stools. If this presentation occurs in early infancy, a workup to exclude biliary atresia may be initiated. Infants with choledochal cysts can have a palpable mass in the right upper abdominal quadrant; this may be accompanied by hepatomegaly.
- 34. Children in whom the condition is diagnosed after infancy present with a different clinical constellation, which includes intermittent bouts of biliary obstructive symptoms or recurrent episodes of acute pancreatitis. Children in whom biliary obstruction is present may also have jaundice and a palpable mass in the right upper quadrant. The correct diagnosis is occasionally more difficult in children with pancreatitis. Often, the only clinical symptoms are intermittent attacks of colicky abdominal pain. Eventually, an analysis of biochemical laboratory values reveals elevations in amylase and lipase levels. This leads to the proper diagnostic imaging workup. Adults with choledochal cysts frequently complain of vague epigastric or right upper quadrant abdominal pain. Indeed, the most common symptom in adults is abdominal pain. A classic clinical triad of abdominal pain, jaundice, and a palpable right upper quadrant abdominal mass has been described in adults with choledochal cysts, although this is found in only 10-20% of patients. Cholangitis can be part of the clinical presentation in adult patients with biliary obstruction. Choledochal cysts not appearing until adulthood can be associated with a number of serious complications resulting from long-standing biliary obstruction and recurrent bouts of cholangitis. These include cholelithiasis, severe pancreatitis, hepatic abscesses, hepatic cirrhosis, and portal hypertension. CT Findings: Abdominal CT scanning is useful in the diagnostic algorithm for choledochal cysts. CT is highly accurate and offers a great deal of information that is helpful not only in confirming the diagnosis but also in planning surgical approaches. CT scans of a choledochal cyst demonstrate a dilatated cystic mass with clearly defined walls, which is separate from the gallbladder. The fact that this mass arises from or actually is the extrahepatic bile duct usually is clear from its location and its relationships to surrounding structures. The cyst is typically filled with bile, which produces water-like attenuation. Depending on the patient's age and clinical history, the wall of the cyst can appear thickened, especially if multiple episodes of inflammation and cholangitis have occurred. Most patients with choledochal cysts have undergone abdominal US imaging prior to CT scanning. US findings suggest the diagnosis in most patients and may be conclusive in many. According to Lipsett and colleagues, CT scanning confirms the diagnosis if it is unclear and provides information concerning the relationships of the cyst to surrounding structures including the portal vein, duodenum, and liver. In addition, CT scanning is superior to US in defining the extent of the cyst in the extrahepatic biliary system and in detecting intrahepatic disease. Recently, CT cholangiography has been used in the diagnosis of choledochal cysts. Spinzi and colleagues published a case report describing CT cholangiography in the diagnosis of a type I choledochal cyst in an adult. The cyst and its extent were demonstrated clearly. The authors did note the need to use retrograde biliary contrast enhancement or intravenous contrast enhancement, and they stated that MR cholangiography may one day obviate CT cholangiography.
- 35. Large type I choledochal cyst and adjacent gallbladder. MRI Findings: Use of MRI and MRCP techniques is increasing dramatically for the noninvasive diagnosis of biliary and pancreatic diseases. Choledochal cysts are no exception. These cysts appear as large fusiform or saccular masses that may be extrahepatic, intrahepatic, or both, depending on the type of cyst. They produce a particularly strong signal on T2-weighted images. Associated anomalies of the pancreatic duct, its junction with the common bile duct, and the long common channel formed by the 2 are usually well demonstrated on MRI/MRCP images. Ultrasonic Findings: US is the initial screening examination of choice in patients with choledochal cysts. Pertinent findings include a cystic extrahepatic mass. Depending on the skill of the operator, the specific type or class of choledochal cyst may be identified. Newer high-resolution US machines help clinicians make such diagnoses. Furthermore, advances in US technology have enabled ultrasonographers to make the diagnosis in the antenatal period. US findings are diagnostic in many patients; however, in the preoperative period, complementary studies, such as ERCP, CT, or MRI/MRCP, may be helpful in delineating details of the surrounding anatomy, the location of an APBJ, and the length of the common pancreatobiliary channel. Abdominal US findings can help in detecting associated conditions and complications of choledochal cysts, such as choledocholithiasis, intrahepatic biliary dilatation, portal vein thrombosis, gallbladder or biliary neoplasms, pancreatitis, and hepatic abscesses. The importance of abdominal US in this disease process cannot be understated. This is highlighted by the fact that US findings initially suggested the diagnosis in many of the studies dealing with other diagnostic modalities referenced in this article.
- 36. Diagnostic sonogram demonstrating a type I choledochal cyst in a 4-month-old child presenting with elevated hyperbilirubinemia and hepatic transaminase levels. Isotopic Findings: Hepatobiliary scintigraphic modalities are used commonly in the setting of acute cholecystitis and in the investigation of neonatal jaundice. In addition, these techniques are useful in the diagnosis of choledochal cysts. Kao and co-investigators studied the significance of nonvisualization of the gallbladder on cholescintigraphy in 27 patients with choledochal cysts. Nonvisualization of the gallbladder occurred in 18 (67%) of 27 patients at 4 hours after injection of the radionuclide. Most of the patients did not have acute cholecystitis. The authors concluded that nonvisualization of the gallbladder in this patient population is not necessarily indicative of acute cholecystitis and that large choledochal cysts may compress the gallbladder, leading to nonvisualization. Surgical specimen
- 37. 7-Patient with Abdominal Pain Etiology : 1. Appendicitis. 2. Pancreatitis. 3. Crhon’s disease 4. Colitis :Ulcerative/Pseudomembranous/Neutropenic. 5. Meckel’s diverticulitis. 6. Cholecystitis. 7. Ovarian cyst complications (torsion/rupture/infection) 8. Urinary causes (stones/pyelonephritis) 9. Intussusception. 10. Volvulus (gastric-mid gut volvulus-caecal-sigmoid ) 11. hematocolpos 12. Sickle cell crisis (splenic /bowel infarction) 13. Referred from pneumonia US show dilated lind ended bowel loop segment :Appendicitis 8-Hypertensive Child Etiology : 1. Renal Cortex scarring (36%). 2. Glomerulonephritis (23%) 3. Co-arctation of Aorta (10% ) 4. Fibromuscular dysplasia of renal arteries (10%) 5. Phaeochromocytoma-functioning neuroblastoma (3%) 6. Polycystic renal disease (6%)
- 38. 7. Hemolytic Uremic syndrome (4%) 8. Renal tumors (2%) 9. Essential (3%). MCUG :Bilteral Grade 5 reflux with right duplex kidney 9-Child with scrotal Problems A-Scrotal Pain Etiology : 1. Epididymo-orchitis. 2. Testicular torsion. 3. Testicular abscess. 4. Varicoceke. 5. Complicated Hernia. 6. Hematoma. B-Scrotal Masses Etiology : 1. Neoplastic : • Primary :a) Germ Cell tumor (70-90%)..Yolk sac tumor-teratoma. b)Sex cord stromal tumors (10-30%) • Secondary :Leukemia-lymphoma- Wilm's tumor. 2. Non neoplastic : 3. Hydrocele. 4. Spermatocele. 5. Epididymal cyst.
- 39. III-CNS and Head &Neck 1.Patient with a neck mass Etiology : 1. Branchial cleft cyst. 2. Thyroglossal cyst. 3. Thyroid masses. 4. Lymphadenopthies. 5. Retropharyngeal abscess . 6. Fibromatosis Coli. 7. Dermoid and dermoid cysts. 8. Rhabdomyosarcoma. 9. 11 .Salivary gland origin (cysts-masses ) 2.Patient with abnormal skin findings Etiology : 1. Neurofibromatosis. 2. Tuberous Sclerosis. 3. Sturge Weber Syndrome. 4. Von-Hipplel Lindau syndrome. 5. Ataxia Telangiectasia. 6. Gorlin Syndrome. 7. Cowden syndrome. 8. Klippel –Trenauny syndrome. 9. Wyburn-Mason syndrome.
- 40. Sturge Weber syndrome :Small left cerebral hemisphere ,gyral calcifications. 3-Patient with Proptosis Etiology : A-Extraconal lesions : Dermoid cyst. Rhabdomyosarcoma. Dacryocystocele. Orbital Abscess. B-Intraconal Lesions: Orbital Pseudotumor. Hemangioma. Optic nerve glioma. Meningioma. Tolosa Hunt Syndrome. Retinoblastoma. Right intraconal mass -Rhabdomyosarcoma
- 41. CT:Persitent Hyperplastic primary vitreous Right orbital haemangioma 4-Patient with Epilepsy Etiology: 1. Perinatal accident (40%) 2. Congenital anomalies and phakomatosis (40%) 3. Post Hypoxic Ischemic Encephalopathy (10% ) 4. Cerebral trauma (10% ) 5. Cerebral tumors (1 % ) Causes of epilepsy according to age :
- 42. Age Causes Neonate Anoxia- Neural malformation- Post infectious. Infant Anoxia-malformation-post infectious –Sturge Weber Syndrome-Tuberous sclerosis- Aicardi syndrome-Mitochondrial diseases. Children Ischemia –infection-trauma Newly discovered Tumor –Vascular malformations (AVM-Cavernoma)-Neural malformation (Cortical epilepsy dysplasia- Hippocampal sclerosis)-Hypothalamic hamartoma. Specific diagnosis : 1.Holoprosencephaly: Holoprosencephaly denotes an incomplete or absent division of the embryonic forebrain (prosencephalon) into distinct lateral cerebral hemispheres. De Myer categorized holoprosencephaly into 3 types (from most severe to least severe): (1) alobar holoprosencephaly, or complete absence of midline forebrain division resulting in a monoventricle and fused cerebral hemispheres; (2) semilobar holoprosencephaly, or incomplete forebrain division resulting in partial separation of cerebral hemispheres, typically posteriorly; and (3) lobar holoprosencephaly, or complete ventricular separation with focal areas of incomplete cortical division or anterior falcine hypoplasia. 2.Schizencephaly : Schizencephaly is an uncommon disorder of neuronal migrational characterized by a cerebrospinal fluid– filled cleft, which is lined by gray matter. The cleft extends across the entire cerebral hemisphere, from the ventricular surface (ependyma) to the periphery (pial surface) of the brain. The clefts may be unilateral or bilateral and may be closed (fused lips), as in schizencephaly type I, or separated (open lips), as in schizencephaly type II. Open lip Schizencephaly 3.Heterotopia: Gray-matter heterotopia means collections of gray matter in abnormal locations. It can be nodular or laminar.
- 43. Heteropic gray matter 5-Patient in STROKE Etiology: 1. Hypoxic Ischemic encephalopathy. 2. Venous thrombosis ..(extension of infection) 3. Moya Moya disease . 4. Vein of Galen Malformation. 5. Arteriovenous malformations. 6. Cavernous hemangioma. Cerebral aneurysms. Hypoxic Ischemic Encephalopathy : In spite of major advances in monitoring technology and knowledge of fetal and neonatal pathologies, perinatal asphyxia or, more appropriately, hypoxic-ischemic encephalopathy (HIE), remains a serious condition, causing significant mortality and long-term morbidity. Brain hypoxia and ischemia due to systemic hypoxemia, reduced cerebral blood flow (CBF), or both are the primary physiological processes that trigger HIE. The initial compensatory adjustment to an asphyxial event is an increase in the CBF due to hypoxia and hypercapnia. In adults, CBF is maintained at a constant level despite a wide range in systemic BP. This phenomenon is known as the cerebral autoregulation, which helps to maintain the cerebral perfusion. Limited data on the preterm infant suggests that a range of blood pressures exist over which cerebral blood flow is stable. Some experts have postulated that in the healthy term newborn the BP range at which the CBF autoregulation is maintained is quite narrow (perhaps between 10-20 mm Hg, compared to the 40 mm Hg range in adults noted above). In the fetus and newborn suffering from acute asphyxia, after the early compensatory adjustments fail, the CBF can become pressure-passive, at which time brain perfusion is dependent on systemic BP. As BP falls, CBF falls below critical levels, and the brain continues to suffer from diminished blood supply and a lack of sufficient oxygen to meet its needs. This leads to intracellular energy failure. During the early phases of brain injury, brain temperature drops, and local release of the neurotransmitter, such as g-aminobutyric acid transaminase (GABA), increase. These changes reduce cerebral oxygen demand, transiently minimizing the impact of asphyxia. At the cellular level, neuronal injury in HIE is an evolving process. The magnitude of the final neuronal damage depends on both the severity of the initial insult and the damage due to reperfusion injury and apoptosis . The extent, nature, severity, and the duration of the primary injury are all important in affecting the magnitude of the residual neurological damage. Following the initial phase of energy failure from the asphyxial injury, cerebral metabolism may recover, only to deteriorate in the secondary phase, or reperfusion. This new phase of neuronal damage, starting at about 6-24 hours
- 44. after the initial injury, is characterized by cerebral edema and apoptosis. This phase has been called the "delayed phase of neuronal injury." Additional factors that influence outcome include the nutritional status of the brain, severe intrauterine growth restriction, preexisting brain pathology or developmental defects of the brain, and the frequency and severity of seizure disorder that manifests at an early postnatal age (within hours of birth). At the biochemical level, a large cascade of events follow HIE injury. Both hypoxia and ischemia increase the release of excitatory amino acids (EAAs), such as glutamate and aspartate, in the cerebral cortex and basal ganglia. EAAs cause neuronal death through the activation of receptor subtypes such as kainate, N-methyl-D-aspartate (NMDA), and amino-3-hydroxy-5-methyl-4 isoxazole propionate (AMPA). Activation of receptors with associated opening of ion channels (eg, NMDA) lead to increased intracellular and subcellular calcium concentration and cell death. A second important mechanism for the destruction of ion pumps is the lipid peroxidation of cell membranes, in which enzyme systems, such as the Na+/K+-ATPase, reside; this can cause cerebral edema and neuronal death. EAAs also increase the local release of nitric oxide (NO), which may exacerbate neuronal damage. The EAAs may also disrupt the factors that control apoptosis, increasing the pace and extent of programmed cell death. The regional differences in severity of injury may be explained by the fact that EAAs particularly affect the CA1 regions of the hippocampus, the developing oligodendroglia, and the subplate neurons along the borders of the periventricular region in the developing brain. This may be the basis for the disruption of long-term learning and memory faculties in infants with HIE. Role of Imaging : o A CT scan of the head can be especially useful to confirm cerebral edema (obliteration of cerebral ventricles, blurring of sulci) manifested as narrowness of the lateral ventricles and flattening of gyri. Areas of reduced density that indicate evolving zones of infarction may be present. Evidence of hemorrhage in the ventricles or in the cerebral parenchyma may also be seen.. An early diagnosis may help in obtaining early neurosurgical consultation and, possibly, surgical therapy. MRI is valuable in moderately severe and severe HIE, particularly to note the status of myelination, to note white-gray tissue injury, and to identify preexisting developmental defects of the brain. Diffusion-weighted MRI scans are also useful early in the course of treatment to identify those areas of the brain with edema. However the easy access to CT ,and its more accurate demonstration of bleeding put itself in a prominent position in evaluation of HIE . CT depicts focal, multifocal, and generalized ischemic lesions. In the first few days after a severe hypoxic-ischemic insult, bilateral hypoattenuations are seen and probably reflect both neuronal injury and edema. CT neuropathologic studies show that areas of edema are correlated with hypoattenuation lesions when autopsy is performed within 10 days of CT, but generalized edema may obscure focal ischemic lesions. Diffuse cortical injury is not initially detected on CT. After days to weeks, diffuse hypoattenuation may appear, with loss of the gray matter–white matter differentiation. Diffuse cerebral atrophy with ex vacuo ventricular dilatation due to severe hypoxemic insult may take several weeks to develop. Atrophy is a consequence of cortical and white-matter destruction. CT scanning can be performed to help reliably diagnose generalized edema in the premature newborn. In partial asphyxia ,there is relative preservation of blood flow to the basal ganglia and brain stem ,the “watershed zones “ between the major arterial territories being most affected . After 48 hours, CT may depict focal ischemic infarcts well. On the first day after a focal thromboembolic event, the ischemic area may not be visible on CT. A CT scan depicting hypoattenuation in the distribution of the left middle cerebral artery in the first day of life suggests prenatal-onset of ischemia. Symptoms of a focal infarct (usually seizures) on the first day of life with normal CT findings and with hypoattenuation developing over the first week suggest perinatal-onset ischemia. Hemorrhagic conversion of a focal ischemic lesion is uncommon in the neonatal period, but CT can depict it easily.
- 45. Rt occipital infarction A CT scan demonstrating generalized, diffuse hypoattenuation after a hypoxic-ischemic event is predictive of both neonatal death and long-term severe disability, whereas normal CT findings are predictive of mild disability or a normal outcome. Regions of high metabolic activity are at risk during profound asphyxia.Sites of active myelination ,such as the posterior limbs o internal capsule and perirolandic regions are particularly vulnerable . Severe cerebral edema may produce the so-called reversal sign The cerebral white matter has greater Ct density than the gray matter. This reversal of density is felt due to accumulation of blood in the capillaries and veins of the white matter because of increased intracranial and venous pressure. Status marmoratus is a rare manifestation of profound HIE ,that occurs in term infants. Hyprermyelination,neuronal loss ,and gliosis occur in the thalami and basal ganglia .There may be hypodensity seen acutely on CT due to edema and necrosis . Hyperdensity may then develop due to hemorrhage or mineralization in these anantomic regions . In somecases ,due to relative preservation of perfusion of the posterior fossa and brain stem ,these structures appear dense when compared with the rest of the brain producing the so-called White cerebellum sign . Status marmoratus . Reversal sign indicates an extremely poor prognosis ;profound atrophy frequently follows this severe asphyxic injury and there may be cystic or cavitary changes ,mineralization ,and gliosis . CT may depict hemorrhagic lesions, which are seen in 10-25% of patients with HIE .. These lesions include intraparenchymal, intraventricular, and subarachnoid hemorrhages. Occlusive disease may affect one or more specific vascular distribution. Emboli are flow directed and principally occlude vessels in the middle cerebral artery territory In vascular thrombosis the vessel may be hyperattenuating due to clotted blood . CT may also depict the delta sign (clot in the sinus) or the empty delta sign (partially recanalized clot in the sinus). On CT, PVL can be visualized around the frontal horns or posteriorly around the trigonal area of the lateral ventricles. PVL appears as a region of decreased attenuation, occasionally intermixed with areas of increased attenuation due to secondary hemorrhage. Periventricular hypoattenuations should be interpreted carefully because maturation and myelination processes increase the lipid and protein content but the water content of the white matter. These changes explain the findings of hypoattenuations in neonates with normal development.
- 46. 6-Patient with Deafness Etiology : A-Congenital causes: 1. External auditory canal atresia. 2. Middle ear cavity hypoplasia. 3. Absence, rotation ,fusion or dysplasia of ossicles. 4. Treacher Collins dysplasia. 5. Inner ear anomalies : 6. Malformation of lateral semicircular canal . 7. Michel deformity =complete labyrinthine aplasia. 8. Large common cavity (vestibule &cochlea). 9. Cochlear aplasia/hypoplasia. 10. Mondini Malformatiom(less than 21/2 turn of cochlea.-most common) 11. 6.Internal auditory canal atresia and stenosis. 12. 7.Vestibular aqueduct dilatation or obliteration. B-Inflammatory lesions: 1. Otitis media and mastoiditis. 2. Otitis externa. C-Neoplastic lesions: 1. Congenital Cholesteatoma. 2. Fibrous dysplasia. 3. Bony exostosis. 4. Nerve shealth tumors. 5. Glomus tumors. 6. Metastasis. 7. Rhabdomyosarcoma. 8. Langerhans cell histiocytosis. D-Traumatic lesions: E-Vascular causes:
- 47. Aberrant course of ICA. High jugular bulb position. 7-Child with neurological signs of a spinal cord lesion. Etiology : 1. Extradural causes. 2. Intradural/extramedullary causes. 3. Intramedullary causes. 8-Neonate with spinal dysraphism Pathophysiology: The defect of spinal dysraphism occurs in the first 8.5 weeks of fetal life. The neural tube develops from ectodermal cells, while mesoderm forms the bony elements, meninges, and muscle. The skin is separated from the neural tube by the mesoderm. Incomplete separation of ectoderm from the neural tube results in cord tethering, diastematomyelia, or a dermal sinus. Premature separation of the cutaneous ectoderm from the neural tube results in incorporation of mesenchymal elements between the neural tube and skin, which may result in the development of lipomas. If the neural tube fails to fuse in the midline posterior spinal abnormalities such as myelomeningoceles occur. Types : ===== 1. Spina bifida Aperta (open) Myeloschisis. Cranioschisis. Dorsal meningocele. Myelomeningocele. Myelocele. Chiari II malformation. 2. Spina bifida occulta ( occult) Lipomyelomeningocele. Lipoma. Congenital dermal sinus. Tethered cord . Myelocystocele. Meningocele. Split notochord syndrome. 3. Associations . Hydromelia. Hemimyelocele. Developmental tumor
- 48. Role of imaging: MRI findings: MRI findings include absent posterior bony elements at the site of the defect. The soft tissue sac containing CSF may be obvious, and the conus is invariably low, coursing dorsally within a capacious dural sac. Inclusion dermal tissue is generally evident as a rounded mass with variable signal intensity often greater than that of the surrounding CSF. Arnold-Chiari II malformations are noted in nearly all cases of myelomeningocele. The small posterior fossa, low insertion of the tentorium, and downward displacement of cerebellar tissue and medulla through a widened foramen magnum are obvious. When the medullary migration is not vertical, the characteristic cervicomedullary kink is noted. Syringomyelia of the cervical cord or syringobulbia and progressive dilatation of the fourth ventricle may account for worsening neurological deficit. Additional findings in Chiari II malformation include partial agenesis of corpus callosum, large massa intermedia, and a beaked tectum. Rarely, a Chiari I malformation is associated with myelomeningoceles in which only the tonsils herniate below the foramen magnum. A tethered cord manifests itself as a low conus and associated spinal lesions. By the age of 2 months, a conus below L2-L3 is considered abnormal. Axial T1-weighted images are most accurate in determining the conus level.A low cord invariably occurs with a myelomeningocele and retethering may occur after repair. Posterior neural arch defects and an increase interpedicular distance are often associated with a lumbosacral lipoma. T1-weighted images have high sensitivity in the detection of lipomas because of the short relaxation time of fat. The fat content may also be confirmed by using fat-saturation techniques. The diagnosis of a thickened filum is made when the filum measures more than 2 mm at the L5-S1 disk space. In diastematomyelia, MRI is used to evaluate the extent of cord clefting, a low position of the conus, scoliosis, other bony anomalies, and the commonly associated syringohydromyelia. The bony spur is well seen on T1-weighted MRIs when fatty marrow is present. Dermoids and epidermoids may be associated with a dermal sinus or occur in isolation. When not associated with dermal sinuses, they may occur with progressive compressive myelopathy or acute onset chemical meningitis due to the rupture of the cyst and the spread of cholesterol crystals in the CSF. The thoracic lumbar and sacral spine are affected, with a slight increase in incidence in the craniocaudal direction. Lipomas are hyperintense on T1-weighted MRIs. Spinal lipomas are usually found in the extradural space in the thoracic region.
- 49. T1- and T2-weighted sagittal MRIs of the lumbar spine show an extradural spinal lipoma communicating with the subcutaneous fat. 9-Abnormal skull shape Craniosynostosis: Background: Craniosynostosis is the premature fusion of the cranial sutures. Craniosynostosis can occur as an isolated defect or as part of a syndrome. Craniosynostosis is called simple when only 1 suture is involved and compound when 2 or more sutures are involved. Pathophysiology: In the recent literature, mutations in genes coding for fibroblast growth factor receptors (FGFRs) in affected families have been reported. The receptors mediate the effects of the fibroblast growth factors that modulate cellular processes, such as growth, differentiation, migration, and survival. FGFR2 mutations, located on chromosome 7, have been recognized in Crouzon disease and Apert, Jackson-Weiss, and Pfeiffer syndromes. Some cases of Pfeiffer syndrome and Crouzon disease involve mutations in both the FGFR1 and FGFR3 genes. These mutations account for a small fraction of cases of craniosynostosis, because most cases have an unclear etiology. With the use of immunocytochemistry techniques, abnormal osteoblastic activity has been observed within the synostotic bone, along with decreased growth rate and alkaline phosphatase production. Histopathologic examinations of resected sutures demonstrate new bone formation at various stages. These stages range from trabecular interdigitation across the fibrous tissue to complete bony fusion. Mortality/Morbidity: In most patients with craniosynostosis involving a single suture, the primary concern is cosmetic. Early diagnosis and surgical therapy are essential to prevent lifelong craniofacial deformity. Patients with diffuse craniosynostosis are at risk of developing increased intracranial pressure (ICP). Patients can have airway problems because of a hypoplastic maxilla or ophthalmologic problems related to shallow orbits. Anatomy: The bones of the cranium (frontal, parietal, temporal, and occipital) are well developed by the fifth month of gestation. The membranous skull bones are joined by connective tissue at the sagittal, coronal, metopic, lambdoid, and squamosal sutures. The anterior fontanel is at the junction of the frontal and parietal bones, and it represents the intersection of the metopic, coronal, and sagittal sutures. It normally closes in children by the age of 20 months. The posterior fontanel, located at the junction of the lambdoid and sagittal sutures, closes by the age of 3 months. Mature suture closure occurs by the age of 12 years, but completion of fusion continues into the third decade of life and beyond. Clinical Details: Skull growth is restricted in the plane perpendicular to the prematurely fused suture and enhanced in the plane parallel to it.
- 50. Synostosis of the sagittal suture produces a long and narrow skull, called scaphocephaly or dolichocephaly. The anteroposterior diameter of the skull is increased, whereas the transverse diameter is decreased. Sagittal synostosis is seen most commonly in males. Although the biparietal diameter is low, the actual head volume is normal; therefore, no increase in ICP, no hydrocephalus, and no neurologic deficits are usually present. Associated anomalies are seen in 26% of patients. Craniosynostosis. Sagittal synostosis. Markedly increased anteroposterior diameter of the head (dolichocephaly) with flattening of the superior contour is noted. Synostosis of the coronal suture can occur bilaterally or unilaterally and is called brachycephaly and plagiocephaly, respectively. Brachycephaly results in a short, wide skull, with a shortened anteroposterior diameter with a flattened occiput and forehead. Brachycephaly is seen more commonly in females and has a higher incidence of neurologic complications, including increased ICP, optic atrophy, and mental retardation. (In contrast, isolated sagittal synostosis is usually associated with normal intellectual function.) A higher incidence of anomalies also is associated, ie, 33% when 1 suture is affected and as high as 59% when both coronal sutures are affected. Craniosynostosis. Coronal synostosis. The anteroposterior diameter of the head is shortened (brachycephaly), with partially fused coronal sutures and a widened sagittal suture.
- 51. Craniosynostosis. Combined synostosis also demonstrating plagiocephaly. Anteroposterior view in a newborn with combined fusion of sagittal and coronal sutures Synostosis of the lambdoid sutures is less common than sagittal and coronal synostosis. A marked flattening and underdevelopment of the posterior fossa are present, and overgrowth of the bregma may occur, resulting in a tall shape called oxycephalic or turricephalic skull. Apert syndrome. Markedly deformed tower-shaped head resulting from premature fusion of all cranial sutures Synostosis of the metopic suture occurs in utero. It is rare and called trigonocephaly. It results in a pointed forehead and hypotelorism, with an increased risk for associated anomalies of the forebrain. Other anomalies often encountered include cleft palate, coloboma, and a wide array of urinary tract abnormalities.
- 52. Trigonocephaly. Oblique view of the skull shows a ridge or keel in the midline of the frontal bone due to early fusion of metopic suture (arrow). A combined synostosis of the coronal and sagittal sutures results in a severe form termed oxycephaly, which leads to microcephaly. In addition, increased ICP is associated with significant neurologic complications. The most severe form is called the kleeblattschنdel deformity or cloverleaf skull, in which the coronal, sagittal, and lambdoid sutures are all affected. The skull resembles a cloverleaf shape, and patients typically have a bulging forehead, proptotic eyes, and severe neurologic impairment. The most common syndrome-associated synostoses are Crouzon disease and Chotzen and Apert syndromes, which account for more than two thirds of syndrome-related craniosynostosis. • Asymmetric craniosynostosis and plagiocephaly characterize Chotzen syndrome, which is inherited as an autosomal dominant trait and associated with facial asymmetry, ptosis of the eyelids, shortened fingers, a low frontal hairline, a long pointed nose, and soft tissue syndactyly. Cervical fusion is often seen at the level of the C2-C3 vertebrae. • Crouzon disease is inherited as an autosomal dominant trait in 75% of patients, whereas the remaining cases are sporadic. The shape varies depending on the order of fusion, but it most commonly results in brachycephaly due to closure of the coronal and basal skull sutures. Associated findings include ocular proptosis, maxillary hypoplasia, parrot-beak nose, and ocular hypertelorism with normal limbs. Hydrocephalus is more common than in the other syndromes. Chronic tonsillar herniation is a common MRI finding that is seen in patients with Crouzon disease. • Apert syndrome (acrocephalosyndactyly) is an autosomal dominant disorder characterized by coronal synostosis in conjunction with a malformed and short cranial base. It is associated with extensive syndactyly of the second, third, and fourth fingers (mitten hands), broad thumbs with radial deviation, toe syndactyly (sock toes), and visual impairment. Risk of mental retardation is increased; one half of patients have an intelligence quotient lower than 70. Cervical vertebrae fusion, primarily at the C5-C6 vertebrae, occurs in 68% of patients. • Carpenter syndrome is inherited as a rare autosomal recessive trait and usually results in the kleeblattschنdel deformity. Soft tissue syndactyly is always present in the hands and feet. Mental retardation is common. o Pfeiffer syndrome is autosomal dominant and differs from Apert syndrome by the presence of polydactyly. • Jackson-Weiss syndrome is mapped to the same gene as Crouzon disease. It results from coronal and basal skull synostosis. Associated findings include enlarged great toes and craniofacial abnormalities similar to those found in Pfeiffer syndrome but in the absence of the thumb abnormalities. • Each syndrome has an increased risk of increased ICP, hydrocephalus, optic atrophy, respiratory problems due to a deviated septum, and disorders of speech and hearing. Surgical intervention
