British Columbia Medical Journal, December 2010 - Revisiting rectal cancer management in British Columbia
- 1. P. Terry Phang, MD, R. Cheifetz, MD, C.J. Brown, MD, C.E. McGahan, MSc, Manoj Raval, MD Revisiting rectal cancer management in British Columbia A high local recurrence rate for rectal cancer has been reduced with the help of new clinical practice guidelines. n 1996 a high local recurrence rate awareness among family doctors, out- I ABSTRACT: An audit of data from 1996 found a high rate of local recur- for rectal cancer was identified in comes analysis using data from pa- rence in patients treated for rectal an audit of outcomes for patients tient follow-up, and provision of feed- cancer in British Columbia. The Col- treated for rectal cancer in BC.1 Pelvic back to participating specialists and orectal Surgical Tumour Group of the recurrence at 4 years occurred in 16% family physicians. Surgical Oncology Network of the BC of rectal cancer patients for all stages Cancer Agency addressed the high and in 27% of Stage 3 patients. In con- Step 1: Outcomes review rate of local recurrence with treat- trast, local recurrence from colon can- Our review of 1996 rectal cancer man- ment strategies of short-course pre- cer is estimated at 5% to 10%. agement in BC1 determined that only operative radiation and total meso- Factors contributing to a higher about 10% of operative reports includ- rectal excision. Education sessions rate of local recurrence after surgical ed statements that the rectal cancer were given for surgeons, oncologists, resection of rectal cancer than after was resected with clear gross radial and pathologists. Initial outcomes resection of colon cancer include more margins and that all mesorectal lymph following implementation of this difficult surgical anatomy in the pelvis nodes were removed in keeping with management plan indicate a reduc- compared with the abdomen, nonstan- the tenants of oncological surgical tion in local recurrence in BC. Issues dardized technique for resection of the resection. Only about 50% of pathol- identified that require further im- rectum, and poor adherence to inter- ogy reports assessed whether radial provement include facilitation of pre- national standards in the provision of margins were histologically free of operative MRI staging and strategies adjuvant radiotherapy. cancer. The mean number of lymph to decrease high positive resection nodes identified at pathology evalua- margin rates for distal third rectal Management plan tion was 6 instead of 12, the minimum cancer location. This communica- Having recognized this significant recommended for accurate staging. tion to the BC medical community problem for rectal cancer patients, the completes the feedback loop for this Colorectal Surgical Tumour Group All authors are members of the Colorectal quality improvement project using a of the Surgical Oncology Network Surgical Tumour Group of the Surgical multidisciplinary approach. (SON) of the BC Cancer Agency de- Oncology Network of the BC Cancer signed a management plan aimed at Agency. Additionally, Dr Phang is an asso- standardizing care across the province ciate professor of surgery at the University and reducing local recurrence. The of British Columbia; Dr Cheifetz is an assis- plan included an outcomes review tant professor of surgery at UBC; Dr Brown to define the problem, strategy devel- is a clinical assistant professor of surgery at opment to address the problem, an UBC; Dr Raval is chair of the Colorectal Sur- education program for specialists, gical Tumour Group of the Surgical Oncolo- implementation of the strategy includ- gy Network and clinical assistant professor This article has been peer reviewed. ing an information campaign to raise of surgery at UBC. 510 BC MEDICAL JOURNAL VOL. 52 NO. 10, DECEMBER 2010 www.bcmj.org
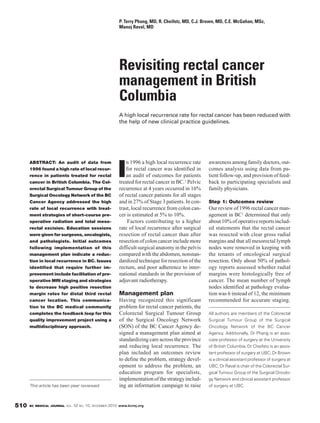
- 2. Revisiting rectal cancer management in British Columbia Adjuvant radiation was given to about 50% of eligible patients with Stages 2 1. Diagnosis is made on biopsy obtained during sigmoidos- and 3 disease. copy or colonoscopy. Step 2: Strategy development 2. Preoperative clinical stage is determined by CT (abdomen, After recognizing these management pelvis) to assess distant spread (clinical stage M) and by deficiencies, we recommended a new MRI (pelvis) or endorectal ultrasound to assess local surgical technique, total mesorectal invasion (clinical Stage T and N, and predicted radial excision (TME), for excision of the resection margin). rectal cancer and all mesorectal lymph nodes within an intact mesorectal fas- 3. Preoperative radiation is indicated for clinical Stages 2 cial envelope.2 Local recurrence rates and 3 (T3-4, N1-2). at 10 years for curative resections using a. Short-course preoperative radiation over 5 days is TME were reported to be as low as recommended for mobile lesions with clear predicted 4%. A new protocol for preoperative radial resection margins. short-course radiation recommended b.Long-course preoperative radiation (with concurrent by Pahlman and colleagues in Sweden reduced local recurrence to 11% from chemotherapy) over 5 weeks is recommended for 27% after follow-up for a minimum clinically fixed lesions or for close/involved predicted of 5 years.3 The combination of short- radial resection margins in order to maximize tumor course preoperative radiation and TME shrinkage prior to surgery. resulted in a 2-year local recurrence 4. Postoperative adjuvant chemotherapy over 4 to 6 months of 2.4% in a Dutch national trial.4 On is given for clinical Stages 2 and 3 lesions. the basis of this and other studies, the clinical guidelines for rectal cancer a. Postoperative adjuvant radiation is given for clinical management in BC (see Figure ) were Stages 2 and 3 lesions if radiation is not given changed to recommend short-course preoperatively. preoperative radiation for Stages 2 and 5. Surveillance is recommended in Stages 2 and 3 patients 3 rectal cancers followed by surgical for 5 years: office visits for rectal examination and resection using TME. The guidelines carcinogenic embryonic antigen testing every 3 to 4 also include preoperative clinical stag- ing using CT, MRI, and endorectal months for 3 years, then every 6 months for years 4 and 5; ultrasound in order to recommend pre- liver imaging (ultrasound or CT) every 6 to 12 months in operative radiation where appropri- the first 3 years, then annually for years 4 and 5; chest ate. Guidelines for pathology report- X-ray every 6 to 12 months; colonoscopy at year 1 and ing include assessment of the radial year 4, then every 5 years thereafter. Flexible sigmoidos- resection margin and examination of copy every 6 to 12 months should also be considered. at least 12 lymph nodes. The recom- mendations were not changed for long- course preoperative chemoradiation Figure. Clinical guidelines for rectal cancer management in BC. for clinically fixed tumors and lesions Adapted from BC Cancer Agency web site (www.bccancer.bc.ca).5 having predicted close resection mar- gins or for adjuvant postoperative care of patients with rectal cancer. (neoadjuvant) and postoperative (ad- chemotherapy for Stage 3 cancers.5 Held in 2002 and 2003, the education juvant) setting, pelvic anatomy, the sessions consisted of lectures, live sur- surgical technique of total mesorectal Step 3: Education program gery with a video link to the audience, excision,6 gross pathology of the resect- To implement the new treatment strat- and hands-on dissection of the pelvis ed TME specimen, and standardized egies, we designed an education pro- in cadaver labs. Session topics includ- operative reporting. A parallel course gram for surgeons, pathologists, and ed preoperative imaging, radiation, of lectures and live demonstration was radiation oncologists involved in the and chemotherapy in the preoperative held for pathologists, including TME www.bcmj.org VOL. 52 NO. 10, DECEMBER 2010 BC MEDICAL JOURNAL 511
- 3. Revisiting rectal cancer management in British Columbia Use of preoperative imaging mo- Use of preoperative imaging modalities dalities of MRI and endorectal ultra- sound continue to be limited because of MRI and endorectal ultrasound of resource limitations in BC and continue to be limited because of because radiologists have not yet adopted a standardized report form for resource limitations in BC and rectal cancer. BC Cancer Agency cen- because radiologists have not yet tres in Victoria, Vancouver, Surrey, Kelowna, and Abbotsford, and soon adopted a standardized report in Prince George, offer potential for form for rectal cancer. creating rectal cancer care pathways to improve accessibility of MR scan- ning and radiation. The Colorectal Surgical Tumour Group of the Surgi- cal Oncology Network has preopera- tive MR imaging on its working agen- specimen processing, gross and mi- for Stage 3 rectal cancers and from da and invites radiologists to join the crosopic findings, and standardized 9.6% to 6.9% overall.14 Use of adju- community of family physicians, sur- pathology reporting.7,8 World experts vant radiation increased to 65%, most- geons, oncologists, and pathologists from the UK, Sweden, the Nether- ly given preoperatively. Negative as integral contributors to the care of lands, and the US were invited to teach radial margins were achieved in 87% rectal cancer patients. at the sessions. Favorable feedback of cases. Pathology reporting showed Technical problems with surgical from course participants regarding the increased assessment of the radial resection of rectal cancer persist in educational value of the sessions and margin to 97% of cases and an aver- BC. Positive radial margins for rectal tests of knowledge retention suggest- age of 12 lymph nodes per case. These cancer location in proximity to the ed good knowledge transfer.9 improvements were statistically and anal sphincter were recorded in 35% clinically significant. of specimens with cancers in the Step 4: Implementation with distal-third of the rectum (located less information campaign Step 6: Feedback than 5 cm from the anus).15 Also, the Our next step was to implement the The final step of the quality improve- rate of permanent colostomy for distal- treatment plan and to inform family ment process involved providing feed- third rectal cancer location was not doctors in BC of the new rectal cancer back to participants. Ongoing reports decreased after the education courses. management strategy. This informa- were provided to BC surgeons at their It seems reasonable to recommend tion was transmitted via the BC Med- annual spring meeting (BC Surgical that surgeons who operate for rectal ical Journal in a two-part theme issue Society) and to oncologists at their cancer less frequently should consid- in July-August and September of annual fall meeting (BC Cancer Agen- er referral of difficult distal-third rec- 2003.10-13 cy), as well as through the SON news- tal cancers to subspecialist surgeons letter. A rectal cancer education course in higher-volume centres.16 Step 5: Outcomes analysis update was held in 2008 that reported Data on patient outcomes were col- on the final outcomes. Conclusions lected and analyzed by the Colorectal Feedback to family doctors in BC Quality improvement in rectal cancer Surgical Tumour Group of the SON. will continue to be provided through treatment will ideally continue in cy- We audited patients treated with cura- the BC Medical Journal. cles of assessment, strategy, and execu- tive-intent major resection of their tion. We have identified improvements rectal cancer in the year after the edu- Further improvements needed in the care of rectal cancer cation courses. This group of patients needed patients and hope to use the recently was compared with patients treated in As with many quality improvement developed cancer surgeon network to our initial study. The main finding of projects, important aspects of care promote these. With a multidisciplinary this audit was a decrease in 2-year requiring further attention have been approach to care, physicians and sur- pelvic recurrence from 18.2% to 9.2% identified. geons continue seeking to improve 512 BC MEDICAL JOURNAL VOL. 52 NO. 10, DECEMBER 2010 www.bcmj.org
- 4. Revisiting rectal cancer management in British Columbia patient outcomes. However, limita- tions in resources and geography pose challenges for quality improvement in our large province. Patient awareness, Surgeons who operate for rectal education, and advocacy will be im- cancer less frequently should portant drivers in the quest to beat col- orectal cancer in British Columbia. consider referral of difficult distal- third rectal cancers to subspecialist Competing interests None declared. surgeons in higher-volume centres. References 1. Phang PT, MacFarlane J, Taylor RH, et al. Effects of positive resection margin and tumour distance from anus on rectal can- cer treatment outcomes. Am J Surg 2002;183:504-508. 7. Quirke P, Durdey P, Dixon MF, et al. Local operative rectal cancer imaging. BCMJ 2. Heald RJ, Moran BJ, Ryall RDH, et al. recurrence of rectal adenocarcinoma due 2003;45:259-261. Rectal cancer: The Basingstoke experi- to inadequate surgical resection. Histo- 12. Phang PT, Law J, Toy E, et al. Pathology ence of total mesorectal excision, 1978- pathological study of lateral tumour audit of 1996 and 2000 reporting for rec- 1997. Arch Surg 1998;133:894-899. spread and surgical excision. Lancet tal cancer in BC. BCMJ 2003;45:319-323. 3. Pahlman L, Glimelius B, and the Swedish 1986;2(8514):996-999. 13. Phang PT, Strack T, Poole B. Proposal to Rectal Cancer Trial investigators. Improv- 8. Nagtegaal ID, van de Velde CJ, van der improve rectal cancer outcomes in BC. ed survival with preoperative radiothera- Worp E, et al.; Cooperative Clinical Inves- BCMJ 2003;45:330-335. py in resectable rectal cancer. N Engl J tigators of the Dutch Colorectal Cancer 14. Phang PT, McGahan CE, McGregor G, et Med 1997;336:980-987. Group. Macroscopic evaluation of rectal al. Effects of change in rectal cancer man- 4. Kapiteijn E, Marijnen CA, Nagtegaal ID, cancer resection specimen: Clinical sig- agement on outcomes in British Colum- et al.; Dutch Colorectal Cancer Group. nificance of the pathologist in quality con- bia. Can J Surg 2010;53:225-231. Preoperative radiotherapy combined with trol. J Clin Oncol 2002;20:1729-1734. 15. Phang PT, Kennecke H, McGahan CE, et total mesorectal excision for respectable 9. Cheifetz R, Phang PT. Evaluating learning al. Predictors of positive radial margin sta- rectal cancer. N Engl J Med 2001;234: and knowledge retention after a continu- tus in a population-based cohort of pa- 638-646. ing medical education course on total tients with rectal cancer. Curr Oncol 5. BC Cancer Agency. Management guide- mesorectal excision for surgeons. Am J 2008;15:1-6. lines for rectal cancer. www.bccancer.bc Surg 2006;191:687-690. 16. Martling AL, Holm T, Rutqvist LE, et al. .ca/HPI/CancerManagementGuidelines/ 10. Phang PT, MacFarlane J, Taylor RH, et al. Effect of a surgical training programme Gastrointestinal/06.Rectum/Manage Practice patterns and appropriateness of on outcome of rectal cancer in the Coun- ment (accessed 8 October 2010). care for rectal cancer management in BC. ty of Stockholm. Lancet 2000;356(9224): 6. Phang PT. Total mesorectal excision: Tech- BCMJ 2003;45:324-329. 93-96. nical aspects. Can J Surg 2004;47:130-137. 11. Malfair D, Brown JA, Phang PT. Pre- www.bcmj.org VOL. 52 NO. 10, DECEMBER 2010 BC MEDICAL JOURNAL 513
